Unhealthy alcohol use is associated with postoperative complications in veterans undergoing lung resection
Introduction
Lung resections come with substantial risk of post-operative complications including mortality (1). Extensive research across diverse populations has identified factors that contribute risk to complications of lung resections (2-14). Among patient level factors, demographics, including age and gender, and comorbidities of preoperative functional status and lung disease consistently demonstrate association with lung resection outcomes.
National recommended limits of alcohol consumption are 14 alcoholic drinks per week in men and 7 alcoholic drinks per week in women (15,16). Unhealthy alcohol use—the spectrum from drinking above national recommended limits to meeting diagnostic criteria for alcohol use disorders (17)—is known to be associated with complications of various surgical procedures (18-22). Further, it is possible that reduction of alcohol use in the perioperative period may mitigate risk (23,24).
Among U.S. veterans, both unhealthy alcohol use and indication for lung cancer screening are relatively common, making this a potentially high yield area for quality improvement in lung resections. Approximately 20% of veterans receiving care in the Veterans Health Administration (VHA) drink at unhealthy levels (25) and it is estimated that nearly 1 in 7 meet eligibility for annual lung cancer screening with low-dose computed tomography (26). With increasing adoption of screening guidelines, the volume of lung resections will climb (27). We performed a retrospective analysis to investigate whether unhealthy alcohol use, defined dichotomously as drinking more than 2 drinks per day, is associated with postoperative complications among VHA patients undergoing lung resection.
Methods
Data sources and study sample
The Veterans Affairs Surgical Quality Improvement Program (VASQIP) database was used for this study. The VASQIP database resides in the Veterans Affairs National Surgery Office and was developed in the 1980s to prospectively record data to inform risk adjustment for perioperative quality improvement (28,29). Data for the VASQIP database are entered by nurse data managers using Veterans Health Information Systems and Technology Architecture at VHA surgical facilities. Patients were included in this study if they underwent pulmonary resection between fiscal years 2007 and 2011. Pulmonary resections were identified using Current Procedural Terminology codes for bilobectomy, lobectomy, and wedge resection or segmentectomy. This study was approved by the VA Puget Sound Health Care System Institutional Review Board, MIRB #00517.
Measures
Independent variable: unhealthy alcohol use, was defined dichotomously as consumption of more than 2 drinks per day. This measure was selected a priori to reflect drinking above national recommended limits and was measured in VASQIP by a preoperative nurse, who records whether patients report drinking more than 2 drinks per day, on average, in the 2 weeks prior to admission. When administering the question, a standard drink is defined consistent with National Institute of Alcohol Abuse and Alcoholism (NIAAA) definitions, as 1 ounce of hard liquor, one 12-ounce can of beer, or one 6-ounce glass of wine.
Outcomes: post-operative complications and mortality. Three outcomes were used to assess post-operative complications and mortality, all of which were measured within 30 days of surgery. Two measures of post-operative complications were used. First, any complication was defined dichotomously as documentation of any of nine post-operative complications within 30 days after surgery. The nine conditions were pre-selected from the VASQIP database for their clinical impact and relevance to lung resection surgery: cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, cerebral vascular accident, systemic sepsis, failure to wean from respirators for more than 48 hours, pneumonia, reintubation for respiratory or cardiac failure, deep surgical site infection, and superficial surgical site infection. Second, post-operative pneumonia within 30 days was individually selected a priori for assessment due to its known relatively high prevalence and clinical impact in this setting (9,30). Mortality was defined as death within 30 days of surgery. Deaths recorded into VASQIP include those that occurred in the hospital and any deaths identified only using VHA Vital Status file data.
Other measures: covariates analyzed included the following variables recorded in VASQIP: patient age in years on the date of surgery; sex; race, as recorded by nurse data manager review patient of charts; functional status, recorded as: (I) independent if the patient does not require assistance; (II) partially dependent if the patient requires assistance for some activities of daily living; (III) totally dependent if the patient cannot perform any activities of daily living independently; American Society of Anesthesiologists (ASA) classification on anesthesia record, defined as: (I) a normal healthy patient; (II) a patient with mild systemic disease; (III) a patient with severe systemic disease; (IV) a patient with severe systemic disease that is a constant threat to life; dyspnea, according to patient describing difficult, painful, or labored breathing: (I) not at all; (II) with minimal exertion, or (III) at rest; smoking status, according to whether the patient has smoked cigarettes in the year prior to admission for surgery; weight loss, defined as >10% unintentional decrease body weight in the 6 months immediately preceding surgery as manifested by serial weights in the chart, as reported by the patient, or as evidenced by change in clothing size or severe cachexia; surgical procedure, according to Current Procedural Terminology code for bilobectomy, lobectomy, or wedge resection/segmentectomy; intraoperative blood loss, as measured by the number of packed or whole red blood cell units given during the operation per the anesthesia record; neoadjuvant chemotherapy, according to receipt of chemotherapy in the 30 days prior to surgery; and neoadjuvant radiation therapy, according to receipt of radiation therapy in the 90 days prior to surgery.
Analyses
Descriptive statistics were run to characterize the cohort overall and frequency of all adverse events by unhealthy alcohol use categorization. Pearson’s chi-square and Welch’s two-sided sample t-test were used to assess differences between groups, as appropriate. Descriptive statistics were not performed in instances in which insufficient events (<10) were recorded.
To evaluate whether unhealthy alcohol use was associated with post-operative complications and mortality within 30 days, we ran multivariate logistic regression models with unhealthy alcohol use as the independent variable and 30-day complications and mortality, respectively, as dependent variables. Models were first unadjusted and then adjusted for all covariates. Covariates included in the fully adjusted model were selected a priori for established or suspected confounding based on associations between each and both unhealthy alcohol use and outcomes of lung resections (3,4,8,10). Analyses were performed using R software version 3.4.2, Vienna, Austria.
Because smoking is associated with lung resection outcomes (8,9), as well as frequently comorbid with unhealthy alcohol use (31), we conducted secondary analyses to assess associations between unhealthy alcohol use and complications and mortality among patients who did and did not report current smoking.
Results
Study population characteristics
We identified 4,719 cases of lung resections performed between fiscal years 2007 and 2011 at 86 VHA Medical Centers recorded in VASQIP. In four cases, data on comorbidities including ASA classification or current smoking status were missing so these were excluded from the final cohort of 4,715 (Table 1). Among these 4,715 patients, the mean age was 65.8 years and the majority were male (96.9%) and white (65.4%). A total of 630 (13.4%) patients reported unhealthy alcohol use (consumption of more than 2 drinks per day). Compared with those not meeting criteria for unhealthy alcohol use, this group was younger (mean of 63.6 versus 66.1 years, P<0.001) and more likely to report current smoking (74.1% versus 52.9%, P<0.001) and to undergo lobectomy (89.8% versus 87.3%, P=0.039). There was no difference between the groups in comorbidities as measured by ASA classification, functional status, and history of dyspnea or weight loss, nor was there a difference in the frequency of administration of neoadjuvant chemotherapy or radiation.

Full table
Association of unhealthy alcohol use with post-operative complications and mortality
Overall, 896 patients (19.0%) experienced post-operative complications within 30 days; 524 (11.1%) had documented pneumonia, and 123 (2.6%) died within 30 days of pulmonary resection. Several complications occurred at a higher frequency among patients meeting study criteria for unhealthy alcohol use (Table 2). These included pneumonia (16.5% versus 10.0%, P<0.001); systemic sepsis (7.1% versus 4.8%, P=0.017); failure to wean from the ventilator within 48 hours of surgery (11.3% versus 7.2%, P=0.001) and re-intubation for respiratory or cardiac failure (13.5% versus 9.2%, P=0.001).
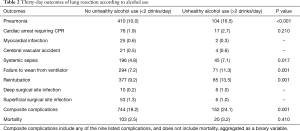
Full table
In unadjusted analyses, consuming more than 2 drinks per day was associated with increased risk of post-operative complications [odds ratio (OR), 1.43; 95% confidence interval (CI), 1.17–1.74] and pneumonia specifically (OR, 1.72; 95% CI, 1.36–2.17) (Table 3). These associations persisted after adjustment for all covariates (OR, 1.42; 95% CI, 1.15–1.74 for all complications; OR, 1.69; 95% CI, 1.32–2.15 for pneumonia). No statistically significant association was identified between consuming more than 2 alcoholic drinks per day and post-operative mortality in the unadjusted (OR, 1.27; 95% CI, 0.75–2.02) or adjusted models. Complete results of the multivariate model are reported in Table S1.
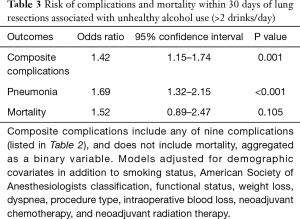
Full table
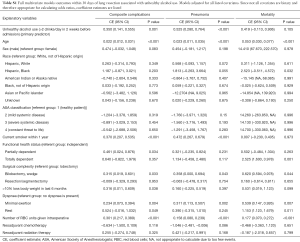
Full table
Secondary analyses stratified by smoking status are presented in Table 4. Unhealthy alcohol use was associated with increased risk of post-operative complications among patients reporting current smoking (OR, 1.51; 95% CI, 1.18–1.91 for all complications; OR, 1.79; 95% CI, 1.36–2.35 for pneumonia) but not among those who did not (OR, 1.23; 95% CI, 0.79–1.85 for all complications; OR, 1.39; 95% CI, 0.80–2.29 for pneumonia). No statistically significant association with mortality was shown in either smoking subgroup (OR, 1.78; 95% CI, 0.96–3.18 in those reporting current smoking; OR, 1.09; 95% CI, 0.32–2.75 in those without current smoking).
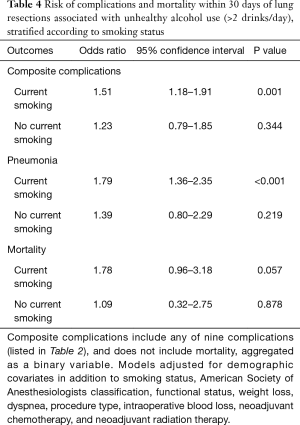
Full table
Discussion
In this large national study of patients that underwent lung resection in the VHA, we found that unhealthy alcohol use, defined dichotomously as consuming more than 2 drinks per day, was associated with increased risk of 30-day post-operative complications but not with 30-day mortality. This risk may be of enhanced significance in patients reporting current smoking (Table 4), perhaps indicative of synergistic influences on immunity, wound healing, and pulmonary reserve (32). These results suggest that identification of unhealthy alcohol use prior to lung resection may assist in risk stratification and present a target for perioperative risk mitigation.
Though unhealthy alcohol use is a well-known risk factor for surgical complications (22), it is not included among the 19 variables used to predict surgical complications by the American College of Surgeons (33). In studies of lung resections specifically, several prior multi-center analyses did not report alcohol consumption as a risk factor for complications (4,8,34). An earlier analysis of VASQIP described 3,516 veterans that underwent lobectomy or pneumonectomy between 1991 and 1995; sub-lobectomies and wedge resections, which constitute 6.9% of the cases here, were not routinely performed in that era (4). In this prior study, unhealthy alcohol use (defined as in the present study) was recorded in a larger proportion of patients (18.7) than in the present study, and did not meet the threshold for significance (P<0.2) in the univariate model for association with postoperative complications.
However, in single-center studies of lung resections, alcohol use has been more prominently identified as associated with surgical risk. Poullis et al. described a single institution experience of lung resections wherein alcohol consumption measured as a linear variable independently associated with in-hospital mortality (6); both Neuenschwander et al. and Paull et al. showed that alcohol consumption at a level of more than 5 drinks per day or meeting criteria for abuse according to standard criteria were associated with postoperative complications (20,35).
Given differences in findings across studies, it may be unsurprising that investigators inconsistently identify unhealthy alcohol use as a risk for postoperative complications: it is a listed comorbidity in the Thoracic Surgery Scoring System (Thoracoscore) but not included as a variable in either the Society of Thoracic Surgeons or European Society Objective Score models, for example (3,8,10,14). Findings from the present study and previous single site studies, however, suggest that unhealthy alcohol use may be a key risk factor for postoperative complications. The variability across studies may reflect differences in populations and illustrates the challenges in defining and accurately describing unhealthy alcohol use (17). While the VASQIP measure is simplistic and therefore comparable across institutions, it is a binary assessment of a behavioral spectrum and only captures drinking habits during the immediate pre-operative period. Moreover, the assessment relies on a question that has not been validated as a screen for unhealthy alcohol use. Further investigations, therefore, should use validated measures of unhealthy alcohol use and account for alcohol use severity and changes in use patterns over time relative to lung resection.
In our adjusted analyses, unhealthy alcohol use was not statistically significantly associated with 30-day post-operative mortality (OR, 1.27; 95% CI, 0.75–2.02). As these events were relatively uncommon (N=123), it is possible that the study was underpowered to measure an association. While the secondary data available for the present study limited assessment of mortality over a longer timeframe, further work is needed to examine whether longer follow-up, for example at any point during the index hospitalization or up to 90 days after surgery, better reflects operative mortality risk (36,37).
We found that, even after adjustment for other factors likely in the pathway, unhealthy alcohol use, defined as consuming more than 2 drinks per day, was associated with postoperative pneumonia. This is consistent with a speculated role for its attenuating pulmonary immunity and pathogen clearance (38). Pneumonia is the most common major complication following lung resection, and is particularly prevalent in cases of lung resection in VA centers (39). Schussler et al. examined factors that predispose to pneumonia after lung resections, identifying pre-existing lung disease, extent of resection, male sex, and presence of intraoperative bronchial colonization as independent risk factors on multivariate analysis (40). Unhealthy alcohol use, defined in their work as the same measure of consuming more than 2 drinks per day, was recorded in 17% of their cohort of 168 patients and was associated with pneumonia in univariate (OR, 3.1; 95% CI, 1.37–7.0) but not multivariate analysis. Post-operative intensive pulmonary hygiene programs are universally implemented after lung resections and include targeted chest physiotherapy, incentive spirometry, and early ambulation to promote clearance of secretions and prevent atelectasis (41). Further research is needed to assess whether patients with unhealthy alcohol use may benefit from modifications to perioperative pneumonia prophylaxis, either by intensification of pulmonary hygiene programs or adjustment of antibiotics to account for differential pathogenic profiles (42).
This study has several important limitations. First, the study is observational and thus cannot attribute causality in the identified associations. While we adjusted for multiple measured factors that may confound the association between unhealthy alcohol use and post-operative complications and mortality, the possibility of residual confounding exists. Smoking is a known risk factor for complications of lung resection and is often associated with increased alcohol use (8,9,31). It is possible that our multivariate and secondary models did not fully account for its confounding effect since measures of smoking volume and time course (e.g., pack years) were not included. Future investigation should examine with more granular assessments the risks that both smoking and alcohol consumption contribute to lung resection, ideally in a prospective fashion. Moreover, as mentioned above, our dichotomous measure of unhealthy alcohol use accurately reflects drinking above recommended limits for men but does not enable assessment of severity of unhealthy alcohol use and does not identify patients with alcohol use disorders. Moreover, given differential recommended limits for women than men per NIAAA, this measure likely identifies women with much more severe unhealthy alcohol use than men. As multiple previous studies have identified increased risk for medical and surgical outcomes with greater severity of unhealthy alcohol use, further research is needed to assess ways in which severity of unhealthy alcohol use influences lung resection outcomes. Further, while the present study had too few women to enable stratified analyses, future research should be stratified by gender when possible. The VASQIP database does not comprehensively capture patient factors, such as other substance use, mental health diagnoses, and socioeconomic determinants, which are known to be associated with unhealthy alcohol use and may also influence post-operative complications (18,43). Similarly, laboratory measures that may be associated with alcohol use and surgical complications, such as tests of liver function and coagulopathy, are not consistently available in VASQIP. Also, details of surgical technique and complexity are limited in this dataset to the anatomical extent of resection. Certain post-operative complications, including changes in mental status less severe than coma or not caused by cerebral vascular accidents, are not directly recorded herein. Comprehensive assessment of post-operative neurological changes in future investigations may strengthen the understanding of mechanisms responsible for poor outcomes associated with unhealthy alcohol use. Additionally, whether a history of alcohol use resulted in nonoperative management for patients otherwise candidates for lung resection cannot be determined from this data. Finally, the use of VHA data enabled this very large retrospective cohort study; however, generalizability may be limited to Veterans and to men given the very small proportion of women included.
Despite these limitations, this study is the largest retrospective cohort study to date to assess the association between unhealthy alcohol use and post-operative complications and mortality in veterans treated with lung resection. The results of this investigation call attention to the potential impact of unhealthy alcohol use, particularly in the setting of ongoing smoking, on costly outcomes after lung resection. While not easily tractable, unhealthy alcohol use stands out among other risk factors including smoking as potentially modifiable. Major surgery may generate a teachable or learnable moment and provide an important opportunity for interventions aimed at reducing alcohol and mitigating post-operative risk (23,44,45).
Acknowledgements
Funding: This work was supported in part by a seed grant from the Veterans Affairs Puget Sound Health Care System office of Research and Development to Dr. Graf; Dr. Williams is supported by a VA Health Services Research & Development Career Development Award (No. CDA 12-268).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the VA Puget Sound Health Care System Institutional Review Board (No. MIRB #00517).
References
- Seder CW, Raymond DP, Wright CD, et al. The Society of Thoracic Surgeons General Thoracic Surgery Database 2017 Update on Outcomes and Quality. Ann Thorac Surg 2017;103:1378-83. [Crossref] [PubMed]
- Bernard A, Rivera C, Pages PB, et al. Risk model of in-hospital mortality after pulmonary resection for cancer: a national database of the French Society of Thoracic and Cardiovascular Surgery (Epithor). J Thorac Cardiovasc Surg 2011;141:449-58. [Crossref] [PubMed]
- Falcoz PE, Conti M, Brouchet L, et al. The Thoracic Surgery Scoring System (Thoracoscore): risk model for in-hospital death in 15,183 patients requiring thoracic surgery. J Thorac Cardiovasc Surg 2007;133:325-32. [Crossref] [PubMed]
- Harpole DH Jr, DeCamp MM Jr, Daley J, et al. Prognostic models of thirty-day mortality and morbidity after major pulmonary resection. J Thorac Cardiovasc Surg 1999;117:969-79. [Crossref] [PubMed]
- Jean RA, DeLuzio MR, Kraev AI, et al. Analyzing Risk Factors for Morbidity and Mortality after Lung Resection for Lung Cancer Using the NSQIP Database. J Am Coll Surg 2016;222:992-1000.e1. [Crossref] [PubMed]
- Poullis M, McShane J, Shaw M, et al. Prediction of in-hospital mortality following pulmonary resections: improving on current risk models. Eur J Cardiothorac Surg 2013;44:238-42; discussion 242-3. [Crossref] [PubMed]
- Bach PB, Cramer LD, Schrag D, et al. The influence of hospital volume on survival after resection for lung cancer. N Engl J Med 2001;345:181-8. [Crossref] [PubMed]
- Fernandez FG, Kosinski AS, Burfeind W, et al. The Society of Thoracic Surgeons Lung Cancer Resection Risk Model: Higher Quality Data and Superior Outcomes. Ann Thorac Surg 2016;102:370-7. [Crossref] [PubMed]
- Agostini P, Cieslik H, Rathinam S, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax 2010;65:815-8. [Crossref] [PubMed]
- Kozower BD, Sheng S, O'Brien SM, et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg 2010;90:875-81; discussion 881-3. [Crossref] [PubMed]
- Strand TE, Rostad H, Damhuis RA, et al. Risk factors for 30-day mortality after resection of lung cancer and prediction of their magnitude. Thorax 2007;62:991-7. [Crossref] [PubMed]
- Lee JY, Jin SM, Lee CH, et al. Risk factors of postoperative pneumonia after lung cancer surgery. J Korean Med Sci 2011;26:979-84. [Crossref] [PubMed]
- Stephan F, Boucheseiche S, Hollande J, et al. Pulmonary complications following lung resection: a comprehensive analysis of incidence and possible risk factors. Chest 2000;118:1263-70. [Crossref] [PubMed]
- Brunelli A, Varela G, Van Schil P, et al. Multicentric analysis of performance after major lung resections by using the European Society Objective Score (ESOS). Eur J Cardiothorac Surg 2008;33:284-8. [Crossref] [PubMed]
- Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Substance Abuse and Mental Health Services Administration 2013.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. December 2015. Available online: https://health.gov/dietaryguidelines/2015/guidelines/
- Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med 2005;352:596-607. [Crossref] [PubMed]
- Bradley KA, Rubinsky AD, Sun H, et al. Alcohol screening and risk of postoperative complications in male VA patients undergoing major non-cardiac surgery. J Gen Intern Med 2011;26:162-9. [Crossref] [PubMed]
- Rubinsky AD, Bishop MJ, Maynard C, et al. Postoperative risks associated with alcohol screening depend on documented drinking at the time of surgery. Drug Alcohol Depend 2013;132:521-7. [Crossref] [PubMed]
- Neuenschwander AU, Pedersen JH, Krasnik M, et al. Impaired postoperative outcome in chronic alcohol abusers after curative resection for lung cancer. Eur J Cardiothorac Surg 2002;22:287-91. [Crossref] [PubMed]
- Nath B, Li Y, Carroll JE, et al. Alcohol exposure as a risk factor for adverse outcomes in elective surgery. J Gastrointest Surg 2010;14:1732-41. [Crossref] [PubMed]
- Eliasen M, Grønkjær M, Skov-Ettrup LS, et al. Preoperative alcohol consumption and postoperative complications: a systematic review and meta-analysis. Ann Surg 2013;258:930-42. [Crossref] [PubMed]
- Kaka AS, Zhao S, Ozer E, et al. Comparison of Clinical Outcomes Following Head and Neck Surgery Among Patients Who Contract to Abstain From Alcohol vs Patients Who Abuse Alcohol. J JAMA Otolaryngol Head Neck Surg 2017;143:1181-6. [Crossref] [PubMed]
- Oppedal K, Møller AM, Pedersen B, et al. Preoperative alcohol cessation prior to elective surgery. Cochrane Database Syst Rev 2012.CD008343. [PubMed]
- Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US Veterans: A systematic review and analysis of assessment methods. Am J Addict 2016;25:7-24. [Crossref] [PubMed]
- Kinsinger LS, Anderson C, Kim J, et al. Implementation of Lung Cancer Screening in the Veterans Health Administration. JAMA Intern Med 2017;177:399-406. [Crossref] [PubMed]
- Stiles BM, Pua B, Altorki NK. Screening for Lung Cancer. Surg Oncol Clin N Am 2016;25:469-79. [Crossref] [PubMed]
- Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs' NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 1998;228:491-507. [Crossref] [PubMed]
- Alluri RK, Leland H, Heckmann N. Surgical research using national databases. Ann Transl Med 2016;4:393. [Crossref] [PubMed]
- Liu GW, Sui XZ, Wang SD, et al. Identifying patients at higher risk of pneumonia after lung resection. J Thorac Dis 2017;9:1289-94. [Crossref] [PubMed]
- Manhapra A, Rosenheck R. Tobacco Use Disorder Among Patients With Smoking-related Chronic Medical Disease: Association With Comorbid Substance Use Disorders. J Addict Med 2017;11:293-9. [Crossref] [PubMed]
- Tonnesen H, Nielsen PR, Lauritzen JB, et al. Smoking and alcohol intervention before surgery: evidence for best practice. Br J Anaesth 2009;102:297-306. [Crossref] [PubMed]
- Bilimoria KY, Liu Y, Paruch JL, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 2013;217:833-42.e1-3.
- Brunelli A, Morgan-Hughes NJ, Refai M, et al. Risk-adjusted morbidity and mortality models to compare the performance of two units after major lung resections. J Thorac Cardiovasc Surg 2007;133:88-96. [Crossref] [PubMed]
- Paull DE, Updyke GM, Davis CA, et al. Complications and long-term survival for alcoholic patients with resectable lung cancer. Am J Surg 2004;188:553-9. [Crossref] [PubMed]
- McMillan RR, Berger A, Sima CS, et al. Thirty-day mortality underestimates the risk of early death after major resections for thoracic malignancies. Ann Thorac Surg 2014;98:1769-74; discussion 1774-5.
- Pezzi CM, Mallin K, Mendez AS, et al. Ninety-day mortality after resection for lung cancer is nearly double 30-day mortality. J Thorac Cardiovasc Surg 2014;148:2269-77. [Crossref] [PubMed]
- Yeligar SM, Chen MM, Kovacs EJ, et al. Alcohol and lung injury and immunity. Alcohol 2016;55:51-9. [Crossref] [PubMed]
- Geraci T, Baratta V, Young J, et al. Lobectomy for Lung Cancer at Veterans Administration Medical Center Versus Academic Medical Center. Ann Thorac Surg 2017;103:1715-22. [Crossref] [PubMed]
- Schussler O, Alifano M, Dermine H, et al. Postoperative pneumonia after major lung resection. Am J Respir Crit Care Med 2006;173:1161-9. [Crossref] [PubMed]
- Mulligan MS, Berfield KS, Abbaszadeh RV. Management of Postoperative Respiratory Failure. Thorac Surg Clin 2015;25:429-33. [Crossref] [PubMed]
- Schussler O, Dermine H, Alifano M, et al. Should we change antibiotic prophylaxis for lung surgery? Postoperative pneumonia is the critical issue. Ann Thorac Surg 2008;86:1727-33. [Crossref] [PubMed]
- Williams EC, Peytremann-Bridevaux I, Fan VS, et al. The association between alcohol screening scores and health status in male veterans. J Addict Med 2010;4:27-37. [Crossref] [PubMed]
- Williams EC, Palfai T, Cheng DM, et al. Physical health and drinking among medical inpatients with unhealthy alcohol use: a prospective study. Alcohol Clin Exp Res 2010;34:1257-65. [PubMed]
- Pedersen B, Oppedal K, Egund L, et al. Will emergency and surgical patients participate in and complete alcohol interventions? A systematic review. BMC Surg 2011;11:26. [Crossref] [PubMed]


