Coronary-pulmonary artery fistula—multiple diagnostic imaging modalities
Introduction
Coronary artery fistula is a rare anomaly of the coronary artery. Most adult patients are usually asymptomatic. There are various imaging modalities to detect coronary artery anomaly such as echocardiography, coronary angiography and multidetector computed tomography (MDCT) angiography. Therefore, we present a case of a 53-year-old woman with coronary-pulmonary fistula, diagnosed by echocardiography, coronary angiography, MDCT angiography.
Case report
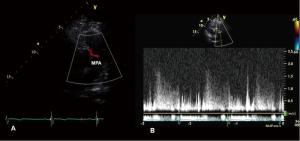
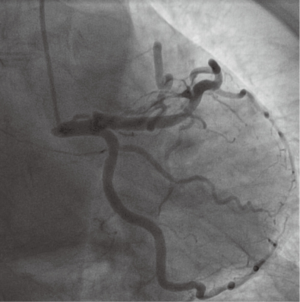
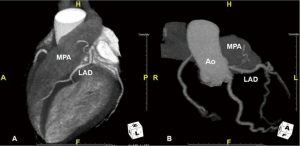
A 53-year-old woman was referred to our hospital for evaluation of increasing dyspnea on exertion. On physical examination, a continuous murmur was heard at the left mid sternal border. Electrocardiogram and chest X-ray were normal. Transthoracic echocardiography revealed a turbulent color flow signal during diastole along the antero-lateral wall of the pulmonary trunk (Figure 1A and Video 1). Pulsed-wave Doppler echocardiography revealed a diastolic signal imaging the main pulmonary artery through the fistula (Figure 1B). The direction and distribution of this abnormal flow was different from that of patent ductus arteriosus. There were no atrial and ventricular dilations with normal systolic function. The coronary artery malformation was confirmed by coronary angiography. Coronary angiography demonstrated a coronary artery fistula in the proximal portion of the left anterior descending artery (LAD) which seemed to drain into the main pulmonary artery (Figure 2 and Video 2). MDCT angiography showed a small, tortuous side artery from the LAD in cranial view; the exact termination could be seen in the main pulmonary artery (Figure 3A). The volume rendered image demonstrates the fistulous communication to the LAD and the main pulmonary artery just like coronary angiography (Figure 3B). Additionally, an exercise stress test was performed and was normal. Therefore, the patient was discharged and followed closely.
Discussion
Coronary artery fistula is a rare anomaly of the coronary artery. The overall population prevalence of coronary artery fistula is estimated at 0.002%. It occurs as an incidental finding in 0.1-0.2% of the coronary artery angiography (1,2). The majority of coronary artery fistulae are related to right coronary artery (55%), while 35% arise from the LAD. The fistula communicated with the right side of the heart in 90% of the case (3). Low-pressure structures are the most common sites of drainage of the coronary artery fistula. Most adult patients are usually asymptomatic; a fistula is incidentally identified in the adult. Nowadays, different cardiac imaging modalities are utilized for diagnosis and optional management of coronary artery fistula. Transthoracic echocardiography showed continuous turbulent flow in the pulmonary artery during diastolic phase in short axis view. However, it is difficult to find the origin of the turbulent color flow (1). Coronary angiography remains the gold standard method for coronary fistulas. It can be used to evaluate the size, number of fistulas and anatomical features of the fistulous tract, but it is expensive and invasive. We cannot find the apparent relation of coronary artery fistula and other structures. MDCT is a minimally invasive, accurate imaging tool for the detection of coronary anormaly (4). The 3D image enables determination of vessel origin and course. The major limitation of MDCT is radiation exposure, which can be substantially lowered by advanced technique. Therefore, MDCT is considered a good alternative to echocardiography and coronary angiography (5). The management of coronary artery fistula is controversial. There is no urgent treatment in asymptomatic cases like this patient. Patients treated conservatively should be followed closely for symptoms.
Conclusions
Coronary pulmonary fistula is a rare congenital disease. Nowadays, different cardiac imaging modalities help us diagnose and optionally manage coronary artery fistula. MDCT should be considered as a non-invasive diagnostic modality to evaluate the localization, anatomy of coronary fistula.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Gowda RM, Vasavada BC, Khan IA. Coronary artery fistulas: clinical and therapeutic considerations. Int J Cardiol 2006;107:7-10. [PubMed]
- Vavuranakis M, Bush CA, Boudoulas H. Coronary artery fistulas in adults: incidence, angiographic characteristics, natural history. Cathet Cardiovasc Diagn 1995;35:116-20. [PubMed]
- Said SA, van der Werf T. Dutch survey of congenital coronary artery fistulas in adults: coronary artery-left ventricular multiple micro-fistulas multi-center observational survey in the Netherlands. Int J Cardiol 2006;110:33-9. [PubMed]
- Manghat NE, Morgan-Hughes GJ, Marshall AJ, et al. Multidetector row computed tomography: imaging congenital coronary artery anomalies in adults. Heart 2005;91:1515-22. [PubMed]
- Zenooz NA, Habibi R, Mammen L, et al. Coronary artery fistulas: CT findings. Radiographics 2009;29:781-9. [PubMed]


