What does the Acute Respiratory Distress Syndrome trial (ART) teach us?—it is time for precision medicine and precision trials in critical care!
Acute respiratory distress syndrome (ARDS) affects a remarkable proportion of patients admitted to the intensive care unit (ICU) and according to a recent international survey, mortality attributable to ARDS remains high (≈40%) (1).
Ventilatory support is a life sustaining treatment utilized to treat hypoxemia as well as enable patients to sustain the increased ventilatory requirement. However, mechanical ventilation, as with any medical therapy, needs to be carefully titrated to improve respiratory function without causing harm. The lung damage that mechanical ventilation can cause in both healthy and previously injured lungs has been named ventilator induced lung injury (VILI) (2). The clinical relevance of VILI was initially revealed by the pivotal ARDS Network trial demonstrating the benefit of lower tidal volume ventilation (and consequently lower airway pressure) in patients with ARDS (3). Since the publication of the ARDS Network trial, the majority of the research in the field of ARDS has been focused on identifying ventilatory strategies developed to protect lungs from VILI while aiming to improve patient survival.
Among the intervention proposed, the application of a positive end expiratory pressure (PEEP) was recognized to reduce alveolar collapse and, consequently, improve hypoxemia. Whether a lower or higher level of PEEP is beneficial in ARDS patients was investigated in three different trials (4-6). None of these trials alone showed beneficial effects of high PEEP versus low PEEP. However, when the results of these trials were taken together in a meta-analysis, they suggested that higher PEEP levels reduced mortality in ARDS patients with severe hypoxemia (PaO2/FIO2 ≤200) (7). Furthermore, additional evidence showed that among patients enrolled in major ARDS randomized clinical trials, decreases in driving pressure (ΔP = the difference between plateau pressure and PEEP) were associated with increased rates of survival (8). Values of driving pressure correlate directly with the size of the lungs available to ventilate and indicates the degree of strain to which the lung parenchyma is subjected to while receives ventilation during ARDS.
Based on these observations, different authors hypothesized that maintaining high levels of lung aeration in patients with ARDS would have reduced VILI by minimizing driving pressure. The “open lung approach” (OLA) aims to achieve high levels of lung aeration in patients with ARDS by first conducting recruitment maneuvers (RMs) to reverse alveolar collapse and then applying the level of PEEP required to keep the alveoli recruited. The OLA strategy provided promising results in preclinical and pilot clinical trials (9-12).
In a recent issue of JAMA, the Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators reported the results of the randomized clinical trial “Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs. Low PEEP on Mortality in Patients with Acute Respiratory Distress Syndrome” (13).
The study has been conducted in 120 ICUs in nine countries (Brazil, Argentina, Colombia, Italy, Poland, Portugal, Malaysia, Spain, and Uruguay). A cohort of 1,010 hemodynamically stable patients affected with moderate to severe ARDS, receiving mechanical ventilation, have been enrolled in the study within 72 hours since the diagnosis of ARDS.
In both the control and experimental groups the strongholds of protective mechanical ventilation were respected: low tidal volume ventilation was applied (6 mL/kg predicted body weight) and plateau pressure was limited to below 30 cmH2O. Patients assigned to the “low-PEEP” group were managed according to the ARDSnet lower PEEP/FiO2 strategy where the focus of care was to ensure a minimum level of oxygen saturation. Patients assigned to the experimental group received a RM followed by a decremental PEEP trial aimed to identify the PEEP level determining the highest value of compliance of the respiratory system representing the optimal balance between alveolar collapse and hyperdistension (14). Apart from the lung RM and PEEP titration scheme, other aspects of care were similar for both groups.
The authors reported that ≈80% of patients assigned to the experimental group completed the whole study procedures, while only 38% received further RMs during the first 7 days of the study. Patients enrolled in the experimental arm of the study received more neuro-muscular blocking agents, had higher requirements of vasopressor and a more positive fluid balance on study day 1. No other differences in co-interventions were detected. During the first 7 days of the study, patients assigned to the study group received a higher (≈3–4 cmH2O) PEEP level compared to the control group, determining a higher average PaO2/FiO2 ratio and a better compliance in the experimental group.
The primary outcome showed an increased rate of death in the experimental group at 7 (31.9%), 28 days (55.3%) and 6 months (65.3%), against a rate of mortality of at 7 days (25.5%) at 28 days (43.3%) and at 6 months (59.9%) of the control group. While the investigators did not detect any difference in the incidence of death due to refractory hypoxemia, acidosis or cardiorespiratory arrest, a higher rate of barotrauma and pneumothorax was detected in the experimental group. Length of stay in the ICU or hospital were also not significantly different. The experimental group had fewer ventilator-free days during the first 28 days. Furthermore, the authors declared that after enrollment of half of the study population the data safety monitoring board requested to limit the maximum airway pressure reached during the RM from 60 to 50 cmH2O due to the occurrence of three cardiac arrest episodes during the maneuver in the experimental group.
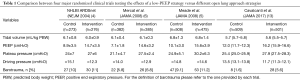
The negative result of the trial is probably even more unexpected when considering that a similar (or even more aggressive) ventilatory approach has been demonstrated improved clinical relevant outcomes in post cardiac surgical patients without a primitive pulmonary disease (15). A potential explanation for the negative trial, pointed out by the researchers of the trial themselves, is that the driving pressure in the experimental group decreased on average only of about 1.5 cmH2O more than the driving pressure of the control group (Table 1). This result might be explained by the average PEEP level applied in the control group, ≈3 cmH2O higher than that reported in the control group of the previous studies. While these reasons might explain the non-superiority of the OLA strategy they do not completely explain the harm attributable to the experimental strategy.
Full table
The unexpected negative result could be tied to the higher incidence of barotrauma and hemodynamic side effects of the high airway pressure strategy used during the RMs in the experimental group. However, when comparing the rate of barotrauma in the present study with respect to those obtained in the previous trials testing different PEEP approaches in ARDS, the incidence of barotrauma in the experimental group is not different from those reported in the previous trials.
At our institutions RMs and decremental PEEP trials, performed both for clinical and research related purposes, are considered invasive procedures and thus are managed only by adequately trained physicians and personnel. Furthermore, thorough respiratory and hemodynamic monitoring is used to prevent potential complications. Esophageal pressure measurement might be beneficial in the calculation of both inspiratory and expiratory transpulmonary pressure, as well as chest wall and lung compliance. Online respiratory imaging such as electrical impedance tomography has been applied to monitor hyperdistention and the percentage of collapse reversal avoiding stretching of lung parenchyma.
Regarding the hemodynamic implications of the RMs and titrated PEEP according to a decremental PEEP trial, to address the incidence of a potential lethal event (cardiac arrest) during a not lifesaving maneuver (RM), the data safety and monitoring board appropriately corrected an overly aggressive recruitment strategy.
The authors reported the requirement of a fluid bolus immediately before the performance of a RM in 89% of the patients enrolled in the experimental arm and increased vasopressor requirement within 1 hour from PEEP titration. This observation confirms that the timing of adjustment of ventilatory settings with respect to the hemodynamic instability of critically ill patients is crucial. Different mechanisms have been postulated to be responsible for hemodynamic related injury during mechanical ventilation using high levels of airway pressures (16-18). However, these hypotheses have not been clearly demonstrated in clinical settings. The availability of monitoring tools (pulmonary artery catheter and/or echocardiography) particularly those used to investigate right heart performance and pulmonary artery pressures could not be avoided in the management of severe ARDS patients to clarify the effects of the modifications of the ventilator settings.
In conclusion, the results of the ART trial, together with evidence derived from the previous trials regarding the high- vs. low-PEEP strategy in ARDS, have led many physicians-scientists to abandon the OLA approach, advocating minimization of VILI and hemodynamic adverse events.
In 2015, the US government launched the precision medicine program with an aim towards classifying individuals with differentiating susceptibilities to certain diseases and their responses to specific treatments into subpopulations of differentiating susceptibilities Therapeutic interventions can then be concentrated on those who will benefit, sparing expense and side effects for those who will not. While this approach is being widely applied in oncologic and cardiovascular treatments, the clinical trials run in the critical care field still apply standardized treatments. Similarly, in the ART trial the approach to select PEEP during mechanical ventilation is individualized because PEEP is selected at the highest value of compliance. However, the decision to randomize patients into the OLA group or a low-PEEP strategy did not consider patient response to lung recruitment. Also, the fixed level of inspiratory pressure during the RM might be useful to homogenize patient treatment but not helpful in improving patient care.
The ART trial was a vast effort across multiple nations and suggests that in order to optimize resources and obtain fruitful information, future clinical trials should test research hypotheses in patients that are responders to the treatment rather than unselectively randomize the entire population.
Acknowledgements
We thank Lisa Alan, Division of General Surgery Anesthesia, for the linguistic revision of the manuscript.
Footnote
Conflicts of Interest: L Berra received research grants from Venner Medical and is supported by NIH/NHLBI 1 K23 HL128882-01A1 for the project titled “Hemolysis and Nitric Oxide”. J Fumagalli has no conflicts of interest to declare.
References
- Bellani G, Laffey JG, Pham T, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016;315:788-800. [Crossref] [PubMed]
- Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med 2013;369:2126-36. [Crossref] [PubMed]
- Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. [Crossref] [PubMed]
- Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 2004;351:327-36. [Crossref] [PubMed]
- Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008;299:637-45. [Crossref] [PubMed]
- Mercat A, Richard JC, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008;299:646-55. [Crossref] [PubMed]
- Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA 2010;303:865-73. [Crossref] [PubMed]
- Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372:747-55. [Crossref] [PubMed]
- Kacmarek RM, Villar J, Sulemanji D, et al. Open Lung Approach for the Acute Respiratory Distress Syndrome: A Pilot, Randomized Controlled Trial. Crit Care Med 2016;44:32-42. [Crossref] [PubMed]
- Amato MB, Barbas CS, Medeiros DM, et al. Beneficial effects of the "open lung approach" with low distending pressures in acute respiratory distress syndrome. A prospective randomized study on mechanical ventilation. Am J Respir Crit Care Med 1995;152:1835-46. [Crossref] [PubMed]
- Cinnella G, Grasso S, Raimondo P, et al. Physiological Effects of the Open Lung Approach in Patients with Early, Mild, Diffuse Acute Respiratory Distress Syndrome: An Electrical Impedance Tomography Study. Anesthesiology 2015;123:1113-21. [Crossref] [PubMed]
- Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095-104. [Crossref] [PubMed]
- Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura ÉA, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA 2017;318:1335-45. [Crossref] [PubMed]
- Suarez-Sipmann F, Böhm SH, Tusman G, et al. Use of dynamic compliance for open lung positive end-expiratory pressure titration in an experimental study. Crit Care Med 2007;35:214-21. [Crossref] [PubMed]
- Costa Leme A, Hajjar LA, Volpe MS, et al. Effect of Intensive vs Moderate Alveolar Recruitment Strategies Added to Lung-Protective Ventilation on Postoperative Pulmonary Complications: A Randomized Clinical Trial. JAMA 2017;317:1422-32. [Crossref] [PubMed]
- Mekontso Dessap A, Boissier F, Charron C, et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med 2016;42:862-70. [Crossref] [PubMed]
- Katira BH, Giesinger RE, Engelberts D, et al. Adverse Heart-Lung Interactions in Ventilator-induced Lung Injury. Am J Respir Crit Care Med 2017;196:1411-21. [Crossref] [PubMed]
- Cambiaghi B, Vasques F, Mörer O, et al. Effects of regional perfusion block in healthy and injured lungs. Intensive Care Med Exp 2017;5:46. [Crossref] [PubMed]


