Isolated traumatic phrenic nerve injury treated with video-assisted thoracoscopic diaphragmatic plication—a case report
Introduction
Diaphragm paralysis caused by a traumatic phrenic nerve injury is rare in adults and can result from any wound that involves the nerve tissue (1). Herein, we present the case of a patient who sustained an accidental stab wound when garden shears pierced her neck and penetrated the spinal canal. This traumatic event resulted in a rare isolated phrenic nerve injury with unilateral diaphragm palsy. The patient was successfully treated with video-assisted thoracoscopic diaphragm plication without any sequelae.
Case presentation
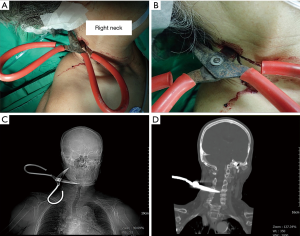
A 76-year-old woman with hypertension fell while working in her garden and was accidentally stabbed in the right side of her neck by her gardening shears during the incident. The patient was hemodynamically stable and had clear consciousness when she arrived at our emergency department. Our examination of the patient revealed no neurological deficits. Her arterial blood gas analysis results were: pH, 7.39; partial pressure of oxygen (PaO2), 91.3 mmHg; partial pressure of carbon dioxide (PaCO2), 37.8 mmHg; bicarbonate (cHCO3), 22.6 mmol/L; and base excess (BE), −1.9 mmol/L. Computed tomography examination of her neck revealed that the shears had pierced deep into the spinal canal through the posterior neck at the level of the fourth cervical (C) vertebra. No vascular injury was identified (Figure 1A,B,C,D, Figure 2A). We performed emergency surgical exploration of her neck and found no vascular, esophageal, or tracheal injuries. One Penrose drain was placed after removing the shears because we suspected there was mild cerebrospinal fluid leakage. We did not perform a dissection to examine the phrenic nerve due to the risk of exacerbating this leakage. Empirical antibiotics were administered postoperatively.

In the following days, her condition remained stable, and no new neurological deficits developed. Screening magnetic resonance imaging of the neck revealed no spinal cord injuries. The Penrose drain was removed from her neck on postoperative day four. However, progressive respiratory distress developed on postoperative day seven; computed tomography and plain radiography of the chest disclosed right diaphragm elevation (Figure 2A,B). Right phrenic nerve injury with diaphragm paralysis was suspected and confirmed by ultrasonography-guided fluoroscopy. The results of her pulmonary test showed her forced expiratory volume 1 (FEV1) was 0.28 L and 17.2% of the predicted value.
Video-assisted thoracoscopic diaphragmatic plication using a stapler was performed. The right intrathoracic phrenic nerve was intact, and no perineural hematoma was identified. The patient was extubated 2 days later without respiratory distress. Her postoperative course was uneventful, and follow-up plain radiography of the chest revealed reduced right diaphragm elevation (Figure 2C). The patient was discharged seven days after the last operation. At her 1-year follow-up, she was doing well and had no oxygen supplementation requirement. At that time, her pulmonary function test showed her FEV1 was 1.54 L and 145% of the predicted value.
Discussion
The phrenic nerve receives contributions from the C3–C5 nerve roots, and it lies directly anterior to the anterior scalene muscle as it courses inferiorly and slightly medially between the levels of the midbody of the C5 vertebra and the midbody of the C7 vertebra (2).
Diaphragm palsy secondary to phrenic nerve palsy is a rare disease with various etiologies, more than two-thirds of which are considered idiopathic (3). Other causes include malignancy, trauma, infectious diseases, neuromuscular diseases, and iatrogenesis (4). The palsy can involve either the whole diaphragm (bilateral) or only one leaflet.
Unilateral phrenic nerve palsy often presents with subtle symptoms, such as exertional dyspnea and is frequently diagnosed incidentally on plain radiographs of the chest. Other diagnostic tools include pulmonary function tests in both the upright and supine positions and paradoxical diaphragm movement in the “sniff test” using ultrasonography or fluoroscopy (1).
Treatment of phrenic nerve palsy depends on the severity of symptoms. There are numerous studies suggesting that prolonged conservative treatment is appropriate for mildly symptomatic patients diagnosed with diaphragm palsy (4). Surgical intervention, i.e., “diaphragm plication” is recommended for patients with unilateral diaphragm palsy and deranged lung function, gas exchange, or both (5). The surgical approaches for diaphragm plication vary from limited lateral thoracotomy through the eighth intercostal space (5) to three-port or uniportal video-assisted thoracoscopic plication (6,7), and these procedures are associated with excellent long-term results.
In conclusion, we present the case of a patient with an isolated phrenic nerve injury secondary to a right neck stab wound that penetrated deep into the spinal canal at the C4 level. Imaging studies showed no associated vascular, esophageal, tracheal, or even spinal cord injury. With early detection, the complication of right diaphragm palsy was successfully treated with video-assisted thoracoscopic diaphragm plication without any sequelae.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: The patient gave written informed consent to publish this case report and any accompanying images.
References
- Versteegh MI, Braun J, Voigt PG, et al. Diaphragm plication in adult patients with diaphragm paralysis leads to long-term improvement of pulmonary function and level of dyspnea. Eur J Cardiothorac Surg 2007;32:449-56. [Crossref] [PubMed]
- Abdunnur SV, Kim DH. Phrenic Nerve Stimulation: Technology and Clinical Applications. Prog Neurol Surg 2015;29:64-75. [Crossref] [PubMed]
- Piehler JM, Pairolero PC, Gracey DR, et al. Unexplained diaphragmatic paralysis: a harbinger of malignant disease? J Thorac Cardiovasc Surg 1982;84:861-4. [PubMed]
- Nelson R, Haydock MD, Haydock DA. Spontaneous Recovery Following Traumatic Phrenic Nerve Palsy. Heart Lung Circ 2016;25:e165-7. [Crossref] [PubMed]
- Dernaika TA, Younis WG, Carlile PV. Spontaneous recovery in idiopathic unilateral diaphragmatic paralysis. Respir Care 2008;53:351-4. [PubMed]
- Stamenovic D. New technique of diaphragmatic plication by means of uniportal video-assisted thoracoscopic surgery. Interact Cardiovasc Thorac Surg 2017;25:162-3. [Crossref] [PubMed]
- Visouli AN, Mpakas A, Zarogoulidis P, et al. Video assisted thoracoscopic plication of the left hemidiaphragm in symptomatic eventration in adulthood. J Thorac Dis 2012;4 Suppl 1:6-16. [PubMed]


