A long-term evaluation of postoperative moist hands after R4/R4+5 sympathectomy for primary palmar hyperhidrosis
Introduction
Primary palmar hyperhidrosis (PPH) is an idiopathic disease characterized by episodically excessive palmar perspiration, and this benign disorder may interfere with a patient’s social activity, professional life and psychological state (1). The gold standard of treatment for PPH is endoscopic thoracic sympathectomy (ETS) (2) because it provides stable long-term results compared to conservative methods.
In 2011, both the International Society of Sympathetic Surgery (ISSS) and the Society of Thoracic Surgeons (STS) committee proposed the use of rib-oriented nomenclature to describe the transected position on the sympathetic chain (2). Therefore, the operation that transects the sympathetic chain on the fourth rib is denoted as R4. Currently, R4 sympathectomy has been validated by several randomized control trials (3-7) as one of optimized procedures on treatment of PPH. For those combined with axillary hyperhidrosis, additional R5 sympathectomy is recommended (2,8).
However, after a large scale of clinical application, a phenomenon was observed that some patients had obtained postoperative moist hands (PMH) rather than completely dry hands after receiving R4 sympathectomy (3). Thus, the exact effect of this surgical procedure remains controversial. To evaluate the long-term results of PMH after R4 and R4+5 sympathectomy, 506 consecutive patients with PPH were retrospectively reviewed and followed-up.
Methods
A total of 506 consecutive patients with severe PPH (264 males, 242 females, average age 25.5±6.5 years), who were treated by video-assisted thoracoscopic R4 or R4+5 sympathectomy between January 2005 and December 2014, were enrolled in this study and retrospectively reviewed. Inclusion and exclusion criteria as follow: (I) age between 12–60 years old; (II) severe palmar sweating was the major complaint with or without axillary and plantar sweating; (III) patients with other diseases which may cause secondary hyperhidrosis or severe postoperative complications such as neurologic disease, hyperthyroidism, diabetes mellitus, severe cardiovascular disease (severe arrhythmia etc.), severe infections, malignancy were excluded; (IV) patients with a history of severe thoracic infection or thoracic surgery were excluded. Among all the patients, 51 individuals had only PPH, 273 individuals were combined with plantar sweating and 182 individuals were combined with plantar and axillary sweating.
The study was approved by the ethics committee on human research of our institution. Follow-up was completed via telephone and e-mail on February 2015. We interviewed patients using a pre-designed questionnaire based on the materials offered and recommended by The Society of Thoracic Surgeons Expert Consensus Documents (2). This modified questionnaire included the following three critical aspects: the degree of sweating improvement, the grade of compensatory hyperhidrosis (CH) and the grade of satisfaction. Sweating improvement was classified into four degrees: (I) sweating had completely vanished, 100% improvement; (II) sweating was greatly reduced, over 50% improvement; (III) sweating was partially reduced, 20–50% improvement; and (IV) sweating was either minimally improved or recurred. The CH was classified into the following four grades: (I) none; (II) mild, not bothersome; (III) moderate, bothersome but tolerable; and (IV) severe, intolerable and expressed regret for surgery. Satisfaction was also classified into four grades: (I) highly satisfied; (II) partially satisfied; (III) dissatisfied; (IV) regret for surgery.
Surgical techniques
All procedures were performed by uniportal thoracoscopy under general anesthesia with endotracheal intubation. Patients were placed in the semi-Fowler’s position, and a 1.5 cm incision was made in the fourth intercostal space on the middle axillary line of both sides. The sympathetic chain was carefully identified and amputated at the fourth/fifth rib via electrocautery. The transection range was laterally extended approximately 2 centimeters along the surface of the corresponding rib to amputate any potential bypass nerve fibers (Kuntz fibers). Both the upper and lower lacerated ends of the sympathetic chain were properly cauterized to prevent nerve regeneration. We applied R4+5 sympathectomy for those patients with concomitant axillary hyperhidrosis. According to the surgical levels on sympathetic chain, patients were divided into group R4 and group R4+5.
Statistical analysis of the comparisons was performed using SPSS 23.0 (SPSS, Inc., Chicago, IL, USA). For continuous variables, descriptive statistics were calculated and reported as the mean ± SD; whereas categorical variables were described using frequency distributions. The Chi-square test was used to detect differences among the qualitative variables. All P values <0.05 were considered statistically significant.
Results
A total of 316 patients underwent bilateral R4 sympathectomy, and 155 patients underwent bilateral R4+5 sympathectomy. There were 35 individuals who underwent different procedures on each side (R4 and R4+5). Severe pleural adhesions and physical interference by either aorta or adjacent intercostal vessels were the primary causes leading to bilateral differences in the procedures.
All procedures were successfully completed without any severe perioperative complications. There was no conversion to thoracotomy or serious intraoperative complication such as massive hemorrhage, arrhythmia or sudden cardiac arrest. Five patients had a small unilateral pneumothorax on X-ray radiography following surgery and resolved on conservative management. There was no Horner’s syndrome, bradycardia, or hemothorax. All patients were discharged 1–2 days after the operations.
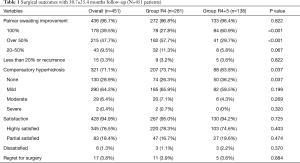
Four hundred and fifty-one patients (89.1%) completed the follow-up with the average follow-up time of 30.7±25.4 months. Among these patients, 281 individuals were in group R4 and 138 individuals were in group R4+5. All results were showed in Table 1.
Full table
Palmar sweating was completely eliminated in 178 patients (39.5%). The incidence of PMH was 57.2%, among which 215 (47.7%) individuals achieved greater than 50% improvement, and 43 (9.5%) individuals achieved 20–50% improvement. These patients presented mild to moderate PMH either during very hot weather or while under stress. Fifteen individuals (3.3%) suffered from recurrence, which instantly developed PMH after surgery but the palmar sweating symptom exacerbated gradually.
A total of 321 patients (71.2%) showed emergence of CH. The most frequent areas affected were the chest, back and abdomen. Mild CH was observed in 290 individuals (64.3%) who were not bothered. Moderate CH, which is described as “annoying but tolerable”, was observed in 29 individuals (6.4%). Only two patients (0.4%) suffered from severe CH and expressed regret for surgery.
Regarding satisfaction, the overall satisfaction rate was 94.9%, among which 345 (76.5%) and 83 (18.4%) patients were highly satisfied and partially satisfied with the surgical results respectively. Six patients (1.3%) were dissatisfied because of frequent PMH. Seventeen patients (3.8%) expressed regret for surgery as 15 individuals suffered from recurrence and 2 individuals developed intolerable CH.
In the subgroup analysis, the group R4+5 had a significantly higher frequency of 100% improvement of palmar sweating compared with the group R4 (27.8% vs. 60.9%, respectively; P<0.001). However, there was no significant difference between two groups regarding the overall effective rate (96.4% vs. 96.8%, P=0.822). As to the side effect, the incidence of CH was significantly lower in the group R4+5 than in the group R4 (63.8% vs. 73.7%, respectively; P=0.037). Lastly, there was no significant difference in the overall satisfaction rate between these two groups (95.0% vs. 94.2%, respectively; P=0.725).
Discussion
ETS has been proved to be a safe and effective treatment for PPH. However, extremely unbearable CH may frequently present among patients who underwent a traditional R2–R4 sympathectomy (9). After decades of exploration, CH could be significantly alleviated by preserving the T2 ganglion and shifting the surgical site lower on sympathetic chain (2). Through December 2014, nearly 30 RCTs, cohort studies and case series describing R4 sympathectomy had been reported with a total of approximately 2,000 individuals. In general, the effective rate of R4 was approximately 70–100% and the satisfaction rate was approximately 94–100%. Regarding CH, the total reported incidence ranged from 0% to 88% (which is a large discrepancy), but less than 1% of those individuals suffered from severe CH. These results demonstrated that R4 sympathectomy was a safe and effective procedure that could be recommended as one of the standard treatment methods for PPH.
However, there were 6 studies in total described the phenomenon of PMH with incidences ranging from 35.5% to 81.0% after R4 sympathectomy and recurrence occurred individually (3,5,10-13). Choi et al. (13) and Kim et al. (11) indicated that trivial hand sweating after R4 could improve the quality of the patient’s hand maneuvering. Compared with the dryness experienced after R3, slight moisture may be more comfortable and easily tolerated by patients. In the reports by Neumayer et al. (10) and Abd Ellatif et al. (12), the satisfaction rate after R4 was significantly higher than that after R3 exactly because of mild PMH. But in the reports of Liu et al. (3) and Wolosker et al. (5), they both demonstrated that whether PMH was beneficial remains unclear and the relationship between PMH and recurrence requires further observation. Based on these findings, the long-term effects of R4 sympathectomy remains controversial.
To date, our cohort in the present study, which comprising 451 R4 and R4+5 cases with an average follow-up time of over 30 months, is the largest single-center R4 case series described worldwide. We performed this retrospective study to re-evaluate the long-term results of PMH after R4 and R4+5 sympathectomy in a large-scale population of individuals clinically treated for PPH.
In the present study, the overall effective rate was 96.7% and the overall satisfaction rate reached 94.9%, which both were comparable to previous studies. However, 258 patients (57.2%) presented PMH and sweating symptoms recurred in 15 patients (3.3%). Among them, 215 (47.7%) achieved greater than 50% improvement and only developed mild- or moderately moist hands either during very hot weather or while under stress, neither of which were reported to disturb their life at all. A total of 43 individuals (9.5%) achieved improvement less than 50%, but only 6 of these patients (1.3%) expressed dissatisfaction after surgery. Recurrence manifested in 15 patients within the first two years after surgery, which highlights the risk of recurrence after R4 or R4+5 sympathectomy.
The reason for varying degree of PMH remains unclear. Anatomical variations may be one cause for this phenomenon. Because the surgical site on the sympathetic chain is still identified by the ribs, the exact spatial relationship between sympathetic ganglions and ribs inconsistent, i.e., when we dissect the sympathetic chain at R4, we do not know whether the T4 sympathetic ganglion has been severed. Due to this situation, treatment results may vary with anatomical variation. To address this issue, we could use indocyanine green near-infrared fluorescence to precisely locate the sympathetic ganglions (14).
Intraoperative monitoring of changes in palmar temperature and blood flow may be a viable method to avoid the PMH phenomenon (15). Li et al. (16) reported that the level of transection should be adjusted by monitoring the temperature change for each individual patient during the operation to achieve the optimal effect. This is an interesting approach, but different reports described highly variable results because there are too many factors that may interfere with intraoperative temperature changes (17). More evidence regarding the value of this novel technique is necessary for further clinical application.
From our perspective, there are another three possible facets to address when solving the problem of PMH. First of all, adequate preoperative communication outlining the possible risks and benefits of PMH is critical to ensure that patients have a correct and appropriate understanding of R4 or R4+5 sympathectomy. Secondly, a shared decision-making pattern allows patients to participate in selecting which level to cut off to achieve a more personalized treatment. Lastly, additional R3 re-sympathectomy is a feasible remedy for individuals who suffered from recurrence after either R4 or R4+5.
In the subgroup analysis, we found that R4+5 sympathectomy appears to be associated with better results compared with R4 sympathectomy. 60.9% of patients in the group R4+5 achieved 100% improvement, which was significantly higher than the corresponding rate observed in the group R4 (27.8%; P<0.001). On the other hand, the incidence of CH in the group R4+5 was significantly lower than that in the group R4 (64% vs 74%, respectively, P=0.037). Therefore, R4+5 sympathectomy may be an effective choice to solve the problems of PMH and CH at the same time. But this conclusion needs to be verified by prospective randomized trial in future.
Generally speaking, we tend to consider the PMH is an advantage for patients with PPH after R4 or R4+5 sympathectomy. As early as 2001, Hashmonai et al. (18) regarded a dry hand as the expected positive outcome of sympathectomy for hyperhidrosis. However, the real goal of treatment for PPH should be improving the patient’s quality of life (3). We must clarify that the ideal result of ETS is to rehabilitate the patient’s palmar sweating function to a normal state but not to eliminate this physiological function from the patient.
The primary limitations of this study include its retrospective design and the lack of randomization. Moreover, the results after comparing R4 and R4+5 should be cautiously interpreted because there was obvious selection bias when dividing the groups.
We concluded that the PMH occurred in over half of patients after R4 or R4+5 sympathectomy, but most of these patients were satisfied with the surgical results. This phenomenon deserves close attention because of its relatively high incidence. Moreover, R4+5 sympathectomy appears to be a better option for PPH with lower incidence of PMH and CH.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethics committee on human research of our institution (2018PHB008-01). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Solish N. Assessing hyperhidrosis disease severity and impact on quality of life. Cutis 2006;77:17.
- Cerfolio RJ, De Campos JR, Bryant AS, et al. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 2011;91:1642-8. [Crossref] [PubMed]
- Liu Y, Yang J, Liu J, et al. Surgical treatment of primary palmar hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg 2009;35:398-402. [Crossref] [PubMed]
- Mahdy T, Youssef T, Elmonem HA, et al. T4 sympathectomy for palmar hyperhidrosis: looking for the right operation. Surgery 2008;143:784-9. [Crossref] [PubMed]
- Wolosker N, Yazbek G, Ishy A, et al. Is sympathectomy at T4 level better than at T3 level for treating palmar hyperhidrosis? J Laparoendosc Adv Surg Tech A 2008;18:102-6. [Crossref] [PubMed]
- Yang J, Tan JJ. T3/T4 thoracic sympathictomy and compensatory sweating in treatment of palmar hyperhidrosis. Chin Med J (Engl) 2007;120:1574-7. [PubMed]
- Ishy A, De Campos JR, Wolosker N, et al. Objective evaluation of patients with palmar hyperhidrosis submitted to two levels of sympathectomy: T3 and T4. Interact Cardiovasc Thorac Surg 2011;12:545-8. [Crossref] [PubMed]
- Lin CC, Telaranta T. Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol 2001;90:161-6. [PubMed]
- Neumayer C, Zacherl J, Holak G, et al. Limited endoscopic thoracic sympathetic block for hyperhidrosis of the upper limb: reduction of compensatory sweating by clipping T4. Surg Endosc 2004;18:152-6. [Crossref] [PubMed]
- Neumayer C, Zacherl J, Holak G, Jakesz R, Bischof G. Experience with limited endoscopic thoracic sympathetic block for hyperhidrosis and facial blushing. Clin Auton Res 2003;13:i52-7. [Crossref] [PubMed]
- Kim WO, Kil HK, Yoon KB, et al. Influence of T3 or T4 sympathicotomy for palmar hyperhidrosis. Am J Surg 2010;199:166-9. [Crossref] [PubMed]
- Abd Ellatif ME, Hadidi AE, Musa AM, et al. Optimal level of sympathectomy for primary palmar hyperhidrosis: T3 versus T4 in a retrospective cohort study. Int J Surg 2014;12:778-82. [Crossref] [PubMed]
- Choi BC, Lee YC, Sim SB. Treatment of palmar hyperhidrosis by endoscopic clipping of the upper part of the T4 sympathetic ganglion. Preliminary results. Clin Auton Res 2003;13:i48-51. [Crossref] [PubMed]
- Weng W, Liu Y, Zhou J, et al. Thoracoscopic Indocyanine Green Near-Infrared Fluorescence for Thoracic Sympathetic Ganglions. Ann Thorac Surg 2016;101:2394. [Crossref] [PubMed]
- Ng I, Yeo TT. Palmar hyperhidrosis: intraoperative monitoring with laser Doppler blood flow as a guide for success after endoscopic thoracic sympathectomy. Neurosurgery 2003;52:127-30. [PubMed]
- Li X, Tu YR, Lin M, et al. Minimizing endoscopic thoracic sympathectomy for primary palmar hyperhidrosis: guided by palmar skin temperature and laser Doppler blood flow. Ann Thorac Surg 2009;87:427-31. [Crossref] [PubMed]
- Liu Y, Li H, Zheng X, et al. Sympathicotomy for Palmar Hyperhidrosis: The Association between Intraoperative Palm Temperature Change and the Curative Effect. Ann Thorac Cardiovasc Surg 2015;21:359-63. [Crossref] [PubMed]
- Hashmonai M, Assalia A, Kopelman D. Thoracoscopic sympathectomy for palmar hyperhidrosis. Ablate or resect? Surg Endosc 2001;15:435-41. [Crossref] [PubMed]


