A comparison between two lung ventilation with CO2 artificial pneumothorax and one lung ventilation during thoracic phase of minimally invasive esophagectomy
Introduction
Esophageal cancer is one of the most common cancers in china, whose incidence rate and mortality rate were as high as 4.8‰ and 3.8‰ in 2015 (1). Surgical resection is considered to be the most effective treatment for early stage esophageal cancer. Researches indicated that open esophagectomy is related to significantly higher morbidity of perioperative complications, while minimally invasive esophagectomy (MIE) is proved to have better short term outcome and has gradually become a standard surgical approach for esophageal cancer in recent years (2,3).
Double lumen endotracheal tube (DLET) is commonly adopted for the anesthesia of MIE, which allows one lung ventilation in order to provide enough surgical space and good exposure. However, disadvantages of DLET anesthesia include rigorous requirement of pulmonary function, sophisticated procedure of intubation, high incidence of displacement during surgery, and frequent respiratory complications after surgery (4,5). Some patients with esophageal cancer are smokers and suffer from chronic respiratory diseases. These patients with poor pulmonary function have higher incidence of perioperative respiratory complications. Some even cannot bear one lung ventilation. Single lumen endotracheal tube (SLET) with CO2 insufflation artificial pneumothorax, which is an alternative for DLET, allows two lung ventilation during surgery, and provides good exposure as well. However, Reports of SLET anesthesia in MIE are rare. Only Zhang et al. and Cai et al. reported 42 and 83 cases (6,7). In video-assisted thoracoscopic surgery (VATS), most application of two lung ventilation with SLET are found in endoscopic sympathectomy and spontaneous pneumothorax which do not require sophisticated surgical operation (4,8-13). As one of the largest esophageal center in china, we adopted SLET with CO2 insufflation artificial pneumothorax and two lung ventilation in MIE since 2013. Here, we retrospectively studied patients who underwent MIE surgery in our center from February 2006 to December 2016, and assessed the safety and feasibility of application of SLET with CO2 insufflation artificial pneumothorax in MIE.
Methods
Patients
Eleven hundred and sixty-six patients with esophageal cancer, who accepted minimally invasive McKeown three-phase esophagectomy in our center from February 2006 to December 2016 (Figure S1), were retrospectively studied. Seven hundred and five patients of them, who accepted general anesthesia with one lung ventilation using a DLET during the thoracic phase of surgery, were assigned to DLET group. Other 461 patients accepted anesthesia with two lung ventilation using a SLET and CO2 insufflation (CO2 pressure =8 mmHg) artificial pneumothorax and were assigned to SLET group. This study has been approved by the Ethics Committee of Zhongshan Hospital (No. B2017-153), and all patients signed informed consent.

Anesthetic and surgical procedure
Combined general-epidural anesthesia is adopted. All the patients adopted the minimally invasive McKeown three-phase esophagectomy (14), which includes the extracorporeal gastric conduit creation and cervical anastomosis between gastric conduit and esophagus. Patients were placed in the left lateral prone position during the thoracic phase and in the supine position during other two phases. The changes of heart rate (HR), blood pressure, SpO2, PetCO2 were collected from the anesthesia note. During surgery, artery blood sample was taken for blood gas analysis once in the thoracic phase (generally 30–60 minutes after the initiation of thoracic phase) and again after thoracic phase (generally 30–60 minutes after thoracic phase) by anesthetist. These data were also collected from the anesthesia note.
Statistical analysis
Data are presented as the mean ± SD. All statistical analysis was performed using SPSS 13.0, with P<0.05 considered statistically significant.
Results
Clinical characteristics of two groups were summarized in Table 1. There were no significant differences in clinical characteristics between two groups, including age, gender, American Society of Anesthesiologists (ASA) grading, smoker number, TNM staging, tumor location, pulmonary function, and concomitant disease.
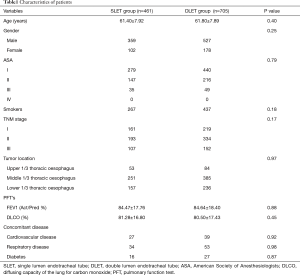
Full table
Surgical variables and postoperative complications were compared between two groups (Table 2). SLET group seemed to have shorter total operative time, shorter thoracic phase time, shorter postoperative hospital stay, more harvested left recurrent laryngeal nerve (RLN) lymph nodes, and more total RLN lymph nodes than DLET group, which might be attributed to experienced surgeons in 2013–2016. However, there were no significant differences of complications between two groups. SLET group seemed to have the symptom of intraoperative hypotension during thoracic phase in a few patients, which could be relieved immediately by the removal of CO2 insufflation.
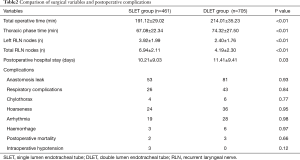
Full table
Clinical parameters, including HR, systolic blood pressure (SBP), diastolic blood pressure (DBP), SpO2, PetCO2, and results of blood gas analysis (pH, PO2, PCO2) were investigated in three time points of surgery (before anesthesia, during thoracic phase, and after thoracic phase). Before anesthesia, there were no differences of these parameters between two groups, except the DBP. During thoracic phase, patients in SLET group had lower blood pressure, and pH value, but higher SpO2, PO2, PCO2, and PetCO2 than patients in DLET group. After thoracic phase, most of these changes were alleviated. Most variables showed no significant differences between two groups. Significant differences were only observed in SpO2 and pH value.
Discussion
Originally, one lung ventilation with DLET was the only choice during the anesthesia of patients who accepted MIE for the purpose of good exposure. However, researches have indicated some disadvantages of one lung ventilation with DLET (15-17), including airway injuries, intraoperative hypoxaemia, tracheobronchial injury, and so on. Many institutions have attempted to replace DLET with SLET in MIE nowadays, in order to avoid these defects. However, it’s still controversial whether patients benefit from SLET with artificial pneumothorax. Most studies were too small to provide meaningful statistical results.
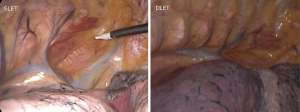
One defect of one lung ventilation with DLET is complicated preoperative intubation and perioperative management. During the placement of DLET, the assistant of a fiber-optic bronchoscope is necessary. Besides, intra-operative translocation of DLET is frequent observed, and replacement is then required which might interrupt surgery. If a patient suffers from tracheostenosis or tracheal malformation, application of DLET seems very hard, and sometimes even impossible. The application of SLET, with easy access and management, does not have these defects. SLET with artificial pneumothorax has been adopted for more than 400 cases of MIE in our center. And its exposure of surgical area is as good as DLET (Figure 1).
Another defect of one lung ventilation with DLET is the requirement of good pulmonary function (18). Patients with poor pulmonary function might not tolerate one lung ventilation during surgery. Arterial oxygen tension decrease was sometimes observed during surgery with one lung ventilation. Although hypoxic pulmonary vasoconstriction of the nonventilated lung might decrease the hypoxia effect, it’s still not as good as two lung ventilation and occasionally develops to severe hypoxemia. This complication is commonly observed in elderly patients with poor pulmonary function (19). Some respiratory complications of MIE are related to one lung ventilation and intraoperative hypoxemia. A few patients would even develop postoperative pulmonary atelectasis and infection after one lung ventilation with DLET. We compared the intraoperative PO2 level between patients in SLET group and DLET group, and found the incidence of hypoxemia was greatly decreased in SLET group. In the 461 patients in SLET group, none was observed with intraoperative hypoxemia. Statistical analysis also proved significantly higher PO2 level during thoracic phase in SLET group (Table 2).
Safety is the main concern of surgical anesthesia. Artificial pneumothorax with CO2 insufflation helps exposure the surgical area needed, but also might cause severe complications as reported (7,12), including cardiovascular collapse, ventricular arrhythmias, and contralateral pneumothorax. However, reported cases of severe complications are rare and most of these studies have some limitations, like small amount of enrolled patient, inappropriate pressure of insufflated CO2, unstandardized protocols, and so on. Further evaluation is necessary. In our study, we retrospectively studied 461 patients underwent artificial pneumothorax with CO2 as SLET group retrospectively. Eight mmHg of CO2 insufflation pressure was adopted during thoracic phase of MIE. No severe respiratory and circulatory complications were observed. We compared the circulatory and respiratory data between SLET group and DLET group. In SLET group, slight change of blood pressure and HR could be found, which was induced by 8 mmHg pressure of CO2 insufflation. Three cases of intraoperative hypotension were observed, but immediately reversed by removal of CO2 insufflation. The pH value was greatly decreased, while PO2, PCO2, and PetCO2 were greatly increased after CO2 insufflation (Table 3). CO2 absorption could induce respiratory acidosis and increase the PCO2 and PetCO2. But these changes did not last long and returned to normal level after removal of CO2 insufflation. Thus, our research indicates that artificial pneumothorax with CO2 insufflation is safe under limited pressure of insufflated CO2 and standardized protocol.
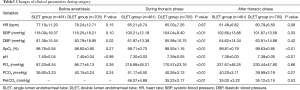
Full table
Another possible defect of SLET is the requirement of consistent CO2 insufflation and stable pressure. When the surgeon decided to change to open surgery or Ivor Lewis esophagectomy during McKeown MIE, it would be hard to maintain good surgical exposure without CO2 pressure. Under this condition, SLET needs to be changed to DLET during surgery.
In order to evaluate the clinical feasibility of two lung ventilation in MIE, we compared the surgical variables and complications between SLET group and DLET group. With similar background of patient characteristics, SLET group seemed to have shorter total operative time, shorter thoracic phase time, shorter postoperative hospital stay, more harvested left RLN lymph nodes, and more total RLN lymph nodes than DLET group. Our data included MIE cases from 2006 to 2016, but SLET was only applied since 2013. Thus, the better outcome of surgical variables of SLET group might be related to more experienced thoracic surgeon in recent years.
In conclusion, our data presented that two lung ventilation with artificial pneumothorax is a safe and feasible choice for MIE. It has the advantages of simple management, good exposure, few complications, and so on. Circulatory inhibition might be a focus of SLET disadvantages, while our study showed no case of severe circulatory complications under limited CO2 pressure and standardized protocol.
Acknowledgements
Funding: This study was supported by the National Nature Science Foundation of China (grant numbers: 81370587, 81500568, 81400681).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study has been approved by the Ethics Committee of Zhongshan Hospital (No. B2017-153), and all patients signed informed consent.
References
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Straatman J, van der Wielen N, Cuesta MA, et al. Minimally Invasive Versus Open Esophageal Resection: Three-year Follow-up of the Previously Reported Randomized Controlled Trial: the TIME Trial. Ann Surg 2017;266:232-6. [Crossref] [PubMed]
- Takeuchi H, Miyata H, Ozawa S, et al. Comparison of Short-Term Outcomes Between Open and Minimally Invasive Esophagectomy for Esophageal Cancer Using a Nationwide Database in Japan. Ann Surg Oncol 2017;24:1821-7. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Sheils TM, et al. Video-assisted thoracoscopic surgery using single-lumen endotracheal tube anesthesia. Chest 2004;126:281-5. [Crossref] [PubMed]
- Cantwell SL, Duke T, Walsh PJ, et al. One-lung versus two-lung ventilation in the closed-chest anesthetized dog: a comparison of cardiopulmonary parameters. Vet Surg 2000;29:365-73. [Crossref] [PubMed]
- Cai L, Li Y, Sun L, et al. Better perioperative outcomes in thoracoscopic-esophagectomy with two-lung ventilation in semi-prone position. J Thorac Dis 2017;9:117-22. [Crossref] [PubMed]
- Zhang R, Liu S, Sun H, et al. The application of single-lumen endotracheal tube anaesthesia with artificial pneumothorax in thoracolaparoscopic oesophagectomy. Interact Cardiovasc Thorac Surg 2014;19:308-10. [Crossref] [PubMed]
- Wong RY, Fung ST, Jawan B, et al. Use of a single lumen endotracheal tube and continuous CO2 insufflation in transthoracic endoscopic sympathectomy. Acta Anaesthesiol Sin 1995;33:21-6. [PubMed]
- Cheng YL, Huang TW, Lee SC, et al. Video-assisted thoracoscopic surgery using single-lumen endotracheal tube anaesthesia in primary spontaneous pneumothorax. Respirology 2010;15:855-9. [Crossref] [PubMed]
- Misthos P, Katsaragakis S, Milingos N, et al. Postresectional pulmonary oxidative stress in lung cancer patients. The role of one-lung ventilation. Eur J Cardiothorac Surg 2005;27:379-82; discussion 382-3. [Crossref] [PubMed]
- Knoll H, Ziegeler S, Schreiber JU, et al. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology 2006;105:471-7. [Crossref] [PubMed]
- Harris RJ, Benveniste G, Pfitzner J. Cardiovascular collapse caused by carbon dioxide insufflation during one-lung anaesthesia for thoracoscopic dorsal sympathectomy. Anaesth Intensive Care 2002;30:86-9. [PubMed]
- Wolfer RS, Krasna MJ, Hasnain JU, et al. Hemodynamic effects of carbon dioxide insufflation during thoracoscopy. Ann Thorac Surg 1994;58:404-7; discussion 407-8. [Crossref] [PubMed]
- Lin M, Shen Y, Feng M, et al. Minimally invasive esophagectomy: Chinese experiences. J Vis Surg 2016;2:134. [Crossref] [PubMed]
- Frölich MA, Janelle GM. Postoperative atelectasis after one-lung ventilation with the Univent tube in a child. J Clin Anesth 2003;15:159-63. [Crossref] [PubMed]
- Roth JV. Complications of One-lung Ventilation: Is It the Blood Flow or the Ventilation? Anesthesiology 2016;125:1253-4. [Crossref] [PubMed]
- Durkin C, Schisler T, Lohser J. Current trends in anesthesia for esophagectomy. Curr Opin Anaesthesiol 2017;30:30-5. [PubMed]
- Benumof JL. One-lung ventilation and hypoxic pulmonary vasoconstriction: implications for anesthetic management. Anesth Analg 1985;64:821-33. [Crossref] [PubMed]
- Lin F, Pan L, Huang B, et al. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation in elderly patients with poor pulmonary function. Ann Thorac Med 2014;9:203-8. [Crossref] [PubMed]


