Uniportal thoracoscopy combined with laparoscopy as minimally invasive treatment of esophageal cancer
Introduction
Video-assisted thoracoscopic surgery (VATS) is widely used for treating lung, pleural and mediastinal diseases. Compared to standard open approach, it presents the same oncological results but several advantages as better cosmetic results and significant reduction of post-operative pain, length of hospital stay (LOS), post-operative morbidity and mortality. In the last years, several authors showed the feasibility of performing also complex thoracic procedures using a single small thoracic incision (uniportal VATS) rather than multi-port incision (standard VATS) (1-4). Herein, we reported an Ivor Lewis esophagectomy for management of adenocarcinoma of the esophago-gastric junction performed using an uniportal approach.
Case presentation
A 67-year-old man was referred to our attention for management of esophageal adenocarcinoma. Chest computed tomography and endoscopy showed that the tumor was localized at the level of the esophagogastric junction and obstructed the 1/3 of the esophageal lumen. Due to the extension of the disease (T2N1M0-Stage IIIA), the patient underwent neo-adjuvant chemo-radiation therapy and after a multidisciplinary meeting he was scheduled for a minimally invasive surgical procedure including laparoscopic gastroplasty, uniportal thoracoscopic esophageal dissection and intrathoracic end-to-end esophago-gastric anastomosis. He was a high risk surgical patient for the presence of several co-morbidities including cardiac disease, COPD and weight loss, thus we supposed that a less invasive approach could reduce the surgical trauma and minimize the risk of postoperative complications. A signed written informed consent was obtained from the patient for the procedure and for publication of this case report and any accompanying images.
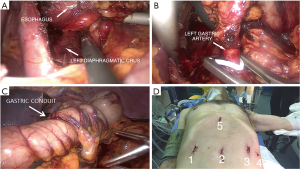
The procedure, summarized in Figure 1, was performed under general anaesthesia with left lung selective ventilation; a nasogastric tube was inserted under endoscopic view. The patient was placed in the supine position and a pneumoperitoneum was performed in a standard fashion. A 30-degree camera was introduced via a 10-mm supra umbilical port. Following, four ports were placed as following: a 10-mm port in the mesogastrium, a 10-mm port in the right upper quadrant, and a 5-mm and a 10-mm port in left upper quadrant. First, we resected the gastro-hepatic ligament, and the right and left diaphragmatic crus to free the abdominal esophagus. Second, to mobilize the stomach we sectioned the gastrocolic omentum, the left gastric artery at level of its origin from celiac trunk, the gastric epiploic vessels, and all posterior adhesions taking care to preserve the right gastro-epiploic vessels during these manoeuvres. All lymph nodes around the vessels were included in the resection. Third, a gastric tube was created in a standard manner leaving part of the fundus connected with the esophago-gastric junction (the procedure is summarized in Figure 2).

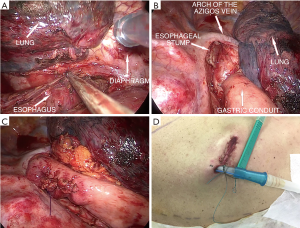
The patient was then placed in the standard left lateral decubitus position with surgeon and assistant placed behind the patient and the scrub nurse on the opposite side. A 5-cm skin incision was performed in the 8th intercostal space at the level of the posterior axillary line and through that a 30° camera and conventional thoracoscopic instruments were inserted. Camera was placed in the posterior part of the incision and no rib spreading was used during the entire procedure. The dissection started from the mediastinal pleura posteriorly and anteriorly to the esophagus from the arch of azygos vein to the diaphragm. After completing esophageal mobilization, the gastric conduit was pulled up into the thorax through the hiatus and rotated in an organ-axial fashion. A standard mediastinal lymphadenectomy was performed and the esophagus was sectioned at the level of the arch of azygos vein. The distal esophageal stump was then closed with a linear stapler as well as the distal portion of gastric tube. The specimen was then removed with an endobag through the uniportal incision. Esophagectomy was completed using a circular-stapled anastomosis between esophagus and gastric conduit. Attention was made to avoid anastomotic tension. A single 28 fr chest tube was inserted through the same incision (the procedure is summarized in Figure 3). No intraoperative and post-operative complications were seen. The patient was extubated in the Intensive Care Unit 2 hours after surgery. In post-operative day 7, chest drainage and nasogastric tube were removed after negative gastrografin swallow and semi-liquid diet was started. The patient was discharged 2 days later. Pathological study diagnosed a T2N1M0-Stage IIB adenocarcinoma, therefore, patient underwent adjuvant chemotherapy. At the time of present paper, he is alive and well without signs of recurrence or metastasis.
Discussion
Minimally invasive surgery has reported as a safe and feasible alternative to traditional open surgery for the treatment of esophageal cancer in selected patients. The first thoracoscopic esophagectomy was described by Cuschieri in 1992 and then several authors have reported their experience with good results (6-8). Uniportal VATS was firstly proposed by Rocco et al. (9) for minor thoracic procedures but with the increasing experience complex procedure using this approach thoracic has been reported in the management of pleural, lung and mediastinal diseases (1-4). Despite conventional multi-port VATS greatly reduces the intensity of post-operative pain compared to open approach, however Passlick et al. (10) showed that up to 32% of patients still have some residual discomfort for up to years after conventional VATS. In theory, the use of a single incision rather than multi-incisions could reduce the thoracic paraesthesia that persisted 19 months after conventional VATS in 53% of patients (11). Thus, the minimal surgical trauma related to uniportal VATS could be particularly useful for management of esophageal cancer especially in high risk surgical patients as the present. However, uniportal VATS remained underused for treatment of esophageal disease and few reports described this technique for resection of esophageal cancer (6-8). From a technical point of view, the main advantages of uniportal compared to standard multi-ports VATS is the different surgical perspective. Multiple port incisions force the surgeon to an unnatural eye to hand coordination compared to what he is used to do in open surgery. Conversely, during uniportal VATS, surgeon works with his eyes and hands in the same plane. The instruments and camera moved in the direction of two parallel lines, allowing maximal convergence of working instruments from each side of the target lesion without interference with the camera. In this way, the esophageal cancer was approached from a cranio-caudal perspective and the operative fulcrum was brought inside the chest in a fashion similar to open surgery. However, our technique differed from standard uniportal VATS for the surgeon position. In standard uniportal VATS, the surgeon and the assistant stand anterior to the patient while in our case the surgeon with the assistant designated to manage the camera were behind the patient. With this distribution, surgeon had the same view of standard open approach and reproduced the same manoeuvres performed during thoracotomy. In addition, assistant had the same field of vision with improvement of coordination and ergonomics. Yet, the eye-hand coordination with uniportal VATS is similar to that of MIE with prone position but the conversion to thoracotomy, if necessary, is difficult in prone position.
As observed for other uniportal thoracic procedures (1-4), our approach compared to standard open procedure (12) would help reduce post-operative pain and favors early return to normal activity. Despite feasible and attractive, our technique is challenging and needing a steep learning curve with long operative time. The use of transorally inserted anvil (OrVilM) and the angulation of the circular-stapler for intrathoracic anastomosis may be difficult at beginning. To perform the incision at the level of the posterior axillary line allows a better exposure of posterior mediastinum and facilitates the dissection of subcarinal lymph nodes compared to the anterior incision but the insertion of the chest tube at this level increases the discomfort for the patient and reduce the cosmetic result compared to a more anteriorly placed tube. For the success of the procedure, the selection of patients is crucial. Calcified mediastinal lymph nodes and tenacious pleural adhesions are the main contraindications. Thus, our initial experience should be corroborated by future and large experiences before it can be widely used.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Caronia FP, Fiorelli A, Santini M, et al. Uniportal Video-Assisted Thoracoscopic Surgery Resection of a Giant Midesophageal Diverticulum. Ann Thorac Surg 2017;103:e365-e7. [Crossref] [PubMed]
- Caronia FP, Fiorelli A, Santini M, et al. Uniportal bilateral video-assisted thoracoscopic extended thymectomy for myasthenia gravis: A case report. J Thorac Cardiovasc Surg 2015;150:e1-3. [Crossref] [PubMed]
- Caronia FP, Fiorelli A, Ruffini E, et al. A comparative analysis of Pancoast tumour resection performed via video-assisted thoracic surgery versus standard open approaches. Interact Cardiovasc Thorac Surg 2014;19:426-35. [Crossref] [PubMed]
- Caronia FP, Arrigo E, Fiorelli A, et al. The main steps of minimally invasive Ivor Lewis esophagectomy performed through a combined laparoscopic and thoracic approach. Asvide 2018;5:441. Available online: http://www.asvide.com/article/view/24503
- Cuschieri A, Shimi S, Banting S. Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 1992;37:7-11. [PubMed]
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [Crossref] [PubMed]
- Levy RM, Trivedi D, Luketich JD. Minimally invasive esophagectomy. Surg Clin North Am 2012;92:1265-85. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Passlick B, Born C, Sienel W, et al. Incidence of chronic pain after minimal-invasive surgery for spontaneous pneumothorax. Eur J Cardiothorac Surg 2001;19:355-8; discussion 358-9. [Crossref] [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Fiorelli A, Izzo AC, Frongillo EM, et al. Efficacy of wound analgesia for controlling post-thoracotomy pain: a randomized double-blind study†. Eur J Cardiothorac Surg 2016;49:339-47. [Crossref] [PubMed]


