Is nutritional status associated with the level of anxiety, depression and pain in patients with lung cancer?
Introduction
Lung cancer is a serious health care problem. It is one of the most malignant cancers and is responsible for 17.6% of total cancer-related deaths. Lung cancer has a poor survival rate despite recent advances in treatment. The overall 5-year survival rate only reaches about 15%, even in well developed countries (1,2). The severity of lung cancer significantly affects both the physical and the emotional condition of patients.
Lung cancer patients often experience nutritional deficiencies, especially those in whom the disease is at an advanced stage and those with a metastatic disease. Disorders such as a subjective sense of poor appetite (anorexia) and symptoms of muscle catabolism and weight loss (cachexia) often occur together and are described as cancer anorexia-cachexia syndrome (CACS). The development of this syndrome contributes significantly to a fatal outcome in cancer patients and it is diagnosed in 80% of them at the terminal stage of the disease (3-5).
Cancer patients who fulfill the criteria of CACS suffer a significant burden of symptoms which reduce quality of life, worsen response to treatment and shorten survival (3,6). Therefore, nutritional risk screening is undertaken to identify patients at risk for malnutrition in order to implement proper interventions to prevent the development and progress of CACS (4). Although these initiatives are effective, the pathogenesis of the development of nutritional disorders in cancer patients as well as the relationship between malnutrition and other factors have not been fully explained. Therefore, we undertook our study to examine associations between malnutrition and emotional status and pain. The aim of the study was to assess the relationship between nutritional status and the level of anxiety, depression and perceived pain in patients with lung cancer.
Methods
For the study, 257 patients with lung cancer who had been hospitalised in the Department of Internal Medicine at the Lower Silesian Centre for Pulmonary Diseases in Wroclaw were recruited. All the patients gave written informed consent to participate in the study and to answer the questionnaires. The study was approved by the Military Medical Chamber Bioethics Committee (No. 152/17). The study aimed to assess nutritional status, pain, depression and anxiety therefore patients were asked to fill the relevant questionnaires after admittance to the hospital, but before the treatment.
To assess the nutritional status, the Mini-Nutritional Assessment (MNA) questionnaire was used. The original MNA system was developed by Guigoz (7,8) and currently it is widely used in the USA and Europe. It comprises questions related to anthropometric measures (BMI, mid-arm and calf circumference), weight loss in the past 3 months, lifestyle, dietary habits (number of meals; protein, fruits, vegetables, and fluid intake), degree of mobility, and self-assessment of health and nutrition status. The maximum possible outcome is 30 points. Normal nutritional status ranges from 24 to 30 points. Results between 17 and 23.5 points indicate that a patient is at risk of malnutrition and below 17 points indicate that they are malnourished (9).
Depression was assessed using the Hospital Anxiety and Depression Scale (HADS). This questionnaire was developed to identify non-somatic depressive symptoms in patients undergoing general medical care. This mood scale has been extensively studied in cancer patients and its use is common in palliative settings. In this study, the 7-item HADS questionnaire for anxiety and depression was used (10). Each item on the scale was scored from 0 to 3, so the total score ranges between 0 and 21. A score below 8 indicates the absence of depressive disorders; between 8 and 10—possible depression and above 10—probable depression. This scale was adapted to polish conditions and validated for use in various groups of patients (11-13).
For the assessment of pain, the Visual Analog Scale for pain (VAS) was used. This single-item scale is simple, easy to complete and widely used among cancer patients and those suffering from post-operative pain. It also gives reliable results in patients with lung cancer (14). It has to be self-completed by patients, who select a point between a 0 score value (no pain) and a 10 score value (the worst pain ever) on a 10-cm horizontal line corresponding to their pain intensity. Results between 1 and 4 are classified as mild pain, between 5 and 6 as moderate pain, and 7 and 10 as severe pain (15).
Statistical analysis
The results of the study were collected in an Excel spreadsheet and statistically analysed. For the purpose of the statistical analysis, the R Package for Statistical Computing v. 3.4.1 was used. The normality of distribution was checked with the Shapiro-Wilk test. Correlations between the level of pain and nutritional status and the level of anxiety and pain were assessed using Spearman’s rank correlation coefficient. For the comparison of more than two groups, the Kruskal-Wallis test with the Duncan’s for post-hoc test were used. A P value of below 0.05 was considered statistically significant.
Results
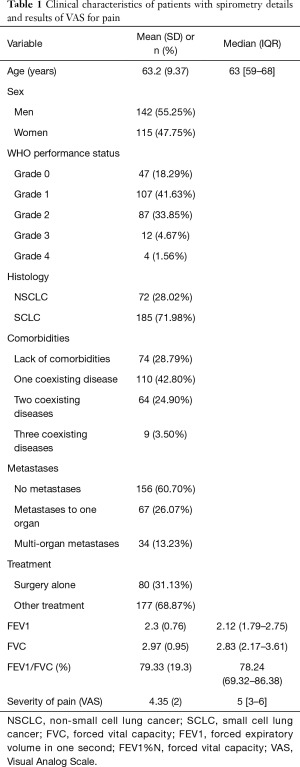
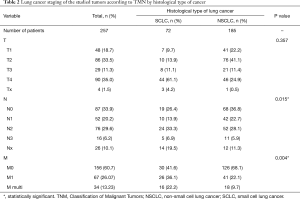
The analysis included 257 patients with lung cancer (115 women and 142 men), with a mean age of 63.2 (SD=9.37) years. The majority of them (154, 59.92%) lived in a relationship, were retirees (181, 70.43%), and had vocational education (118, 45.91%). One hundred and eighty-five (71.98%) of the study group suffered from non-small cell lung cancer (NSCLC), while 72 (28.02%) of them from small cell lung cancer (SCLC). The diagnosis was confirmed by histology. Concomitant diseases were frequent in the study group; 74 (28.79%) had no comorbidities and 183 (71.21%) had one to three other chronic diseases. In 101 (39.30%) patients, metastases were diagnosed, either to one organ or multi organ. Eighty (31.13%) patients were treated exclusively with surgery, while others were offered other types of therapy or combined therapy. Clinical characteristics of patients with spirometry details are presented in Table 1. Lung cancer staging in the study groups is presented in Table 2.
Full table
Full table
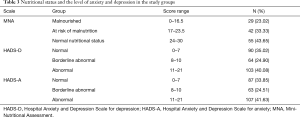
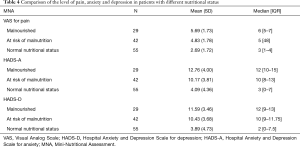
The average result for levels of pain was on the borderline of mild and moderate levels of pain (Table 1). Over half of the study group were discovered to have nutritional disorders. Two thirds of the patients had various degrees of anxiety and depressive disorders (Table 3). A significant negative correlation between nutritional status and the level of perceived pain was observed (r=−0.65; P<0.001), which means that the better the nutrition status, the lower the pain. The comparison of perceived pain among groups of patients with different nutritional status revealed that malnourished patients reported a significantly higher level of pain than patients with a normal nutritional status (Table 4).
Full table
Full table
Similar relationships were found between nutritional status and the HADS score. Better nutritional status was significantly associated with lower levels of anxiety and depression (r=−0.68; P<0.001 and r=−0.60; P<0.001, respectively). Correlations between nutritional status and HADS or VAS are also presented in Figure 1.
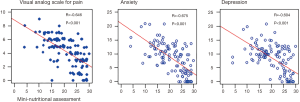
A comparison of the level of anxiety, depression and perceived pain among patients with the three MNA nutritional statuses revealed significant differences, with P<0.001 for each variable. The level of anxiety, depression and perceived pain differed significantly between patients with a normal nutritional status and patients at risk of malnutrition and between patients with a normal nutritional status and malnourished subjects (all P<0.001). Differences between malnourished patients and those at risk of malnutrition were insignificant.
Discussion
Our study showed that nutritional disorders and the presence of anxiety and depression are common among patients with lung cancer. Additionally, patients with a normal nutritional status showed lower levels of perceived pain and lower levels of anxiety and depression than patients with nutritional disorders. The strong association between nutritional status and the latter symptoms indicate that poor nutritional status affects factors which lead to increased mortality and morbidity among lung cancer patients.
The importance of assessing nutritional status in lung cancer patients arises both from the high prevalence of malnutrition in this groups of patients and the association of malnutrition with poor outcomes. Reports from the literature show that many patients with lung cancer experience nutritional deficits and weight loss. The Eastern Cooperative Oncology Group focused on weight assessment in cancer patients. They revealed that patients with favourable subtypes of cancer have the lowest frequency of weight loss, while aggressive tumours had the highest frequency of weight loss (30% vs. 87%). Patients with lung cancer were classified in a group of diseases that have an intermediate frequency of weight loss (SCLC, 57% and NSCLC, 61%) (16). Bagan et al. examined 86 consecutive patients with NSCLC referred for a pneumonectomy. In this group, 39% of the patients were already malnourished before treatment, as measured by biological markers (16). The assessment of nutritional status conducted by Gioulbasanis et al., among patients with metastatic lung cancer who were referred to their institution for the initiation of systemic therapy, revealed that only 27.8% had an adequate nutritional status according to the MNA, while 46.2% were at risk of malnutrition and 26.0% were malnourished (17). In the present study, the percentage of patients with nutritional disorders was also high, as malnourished patients and patients at risk of malnutrition constituted over half of the study group (23.02% and 33.33%, respectively). It is also worth noting that in many lung cancer patients weight loss can already be observed at diagnosis, which worsens their health condition even before they start treatment.
Malnutrition negatively affects the prognosis. Mori et al. analysed data from 406 patients treated surgically for primary lung cancer who were followed-up for a median of 55.1 months. In this group, nutritional status was assessed using prognostic nutritional index (PNI) and analysed together with other clinical-pathological factors. A PNI result of above 50 was associated with a younger age and pathological stage I. The 5-year survival rate was significantly higher in patients with a PNI above 50 than in those with a PNI below 50 (84.4% vs. 70.7%, respectively). Postoperative complications occurred more often in patients with a lower PNI and additionally, the PNI together with the pathological stage of the disease were identified as independent prognostic factors (18). Dewys et al. showed that in both histological subtypes of lung cancer, weight loss had a prognostic effect in patients with tumours of a limited extent. Interestingly, in patients with a more advanced tumour extent who were undergoing chemotherapy, weight loss had no effect on survival (19). In Bagan et al.’s study, malnutrition appeared to be the predictive factor for major postoperative complications, with an odds ratio (OR) of 1.76 and 90-day mortality with an OR of 6.5 in patients undergoing a pneumonectomy due to NSCLC (16). Similarly, in 52 patients undergoing curative resection for lung carcinoma, the complication risk after a pneumonectomy was associated with their nutritional status, as reported by Jagoe et al. In their study, poor nutritional indices (weight and skin-fold thickness) significantly increased the risk of death and reventilation. These parameters also increased the rate of development of pneumonia and other pulmonary complications, but to a lesser extent (20).
Identifying factors which contribute to a worsening nutritional status in cancer patients is important for the planning of treatment. Patients at risk of malnutrition and malnourished patients often report a higher level of perceived symptoms than those with a normal nutritional status. Persistent distress, depression, and pain are among the predisposing risk factors for CACS; however, controversies remain as to the scope of the specific causative factors of this symptom (4). Pain in lung cancer patients can be associated both with the progression of the disease and surgical treatment. Gonzalez et al. found that in their cohort of 2,390 patients, 40% of lung cancer patients suffered from pain and 46% reported treatment of pain. Additionally, depression, along with other factors, was significantly associated with more pain-related interference (21). Park et al. conducted their study among 278 patients undergoing curative surgical resection for primary lung cancer. They reported that severe pain was identified as a risk factor for postoperative depression after adjusting for preoperative depression (OR=3.9; P=0.001) (22). The assessment of nutritional status in patients with metastatic NSCLC stage IV or extended stage SCLC referred for chemotherapy, which was performed by Giannousi et al., revealed significant correlations between the MNA score and depression (r=0.275; P=0.002) while the correlation between the MNA score and anxiety was insignificant (23). The results from the present study are consistent with previous reports; however, the associations between nutritional status and the severity of symptoms such as anxiety, depression, and pain are stronger than in former studies. Interestingly, our study showed that the deterioration in nutritional status found at diagnosis is associated with a significant worsening in terms of depression, anxiety, and pain. This suggests that there is a need to examine nutritional status and psychological well-being at diagnosis in order to introduce interventions aimed at the improvement of nutritional status, mental health and perceived symptoms as early as possible in the treatment process. Inconsistent reports from the literature on the efficacy of nutritional interventions on the improvement of patients’ well-being (24) highlight the need for novel approaches to the problem. Possibly the analyses of symptoms may help to find the underlying causes of associations among clusters of symptoms. Identifying patients at risk who show specific symptoms and assessing the role of genetic polymorphisms may facilitate the development of tailored therapies for lung cancer patients (25).
Limitations of the study
There are several limitations of the study. First of all the study includes heterogeneous group of patients. The study group encompasses both types of lung cancer: NSCL and SCLC. Patients from the study group received various types of treatment and as a result it was not possible to compare groups with one type of treatment.
Conclusions
The prevalence of nutritional disorders and the degree of intensity of somatic symptoms and psychological distress is high among lung cancer patients. The significant levels of depression, anxiety and pain in patients at risk of malnutrition which were highlighted in comparison to patients with a normal nutritional status indicate the need for early supportive psychotherapy or pharmacological interventions.
Acknowledgements
Funding: This study was performed within the project of Wroclaw Medical University number ST.E020.17.050.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Military Medical Chamber Bioethics Committee (No. 152/17). All the patients gave written informed consent to participate in the study and to answer the questionnaires.
References
- Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med 2011;32:605-44. [Crossref] [PubMed]
- Didkowska J, Wojciechowska U, Mańczuk M, et al. Lung cancer epidemiology: contemporary and future challenges worldwide. Ann Transl Med 2016;4:150. [Crossref] [PubMed]
- LeBlanc TW, Samsa GP, Wolf SP, et al. Validation and real-world assessment of the Functional Assessment of Anorexia-Cachexia Therapy (FAACT) scale in patients with advanced non-small cell lung cancer and the cancer anorexia-cachexia syndrome (CACS). Support Care Cancer 2015;23:2341-7. [Crossref] [PubMed]
- Del Ferraro C, Grant M, Koczywas M, et al. Management of Anorexia-Cachexia in Late Stage Lung Cancer Patients. J Hosp Palliat Nurs 2012.14. [PubMed]
- Nelson KA. The cancer anorexia-cachexia syndrome. Semin Oncol 2000;27:64-8. [PubMed]
- Moreland SS. Nutrition screening and counseling in adults with lung cancer: a systematic review of the evidence. Clin J Oncol Nurs 2010;14:609-14. [Crossref] [PubMed]
- Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev 1996;54:S59-65. [Crossref] [PubMed]
- Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature--What does it tell us? J Nutr Health Aging 2006;10:466-85; discussion 485-7. [PubMed]
- Vellas B, Villars H, Abellan G, et al. Overview of the MNA--Its history and challenges. J Nutr Health Aging 2006;10:456-63; discussion 463-5. [PubMed]
- Mitchell AJ, Meader N, Symonds P. Diagnostic validity of the Hospital Anxiety and Depression Scale (HADS) in cancer and palliative settings: a meta-analysis. J Affect Disord 2010;126:335-48. [Crossref] [PubMed]
- Watrowski R, Rohde A. Validation of the Polish version of the Hospital Anxiety and Depression Scale in three populations of gynecologic patients. Arch Med Sci 2014;10:517-24. [Crossref] [PubMed]
- Karakuła H, Grzywa A, Spila B, et al. Use of Hospital Anxiety and Depression Scale in psychosomatic disorders. Psychiatr Pol 1996;30:653-67. [PubMed]
- Wichowicz HM, Wieczorek D. Screening post-stroke depression using the Hospital Anxiety and Depression Scale. Psychiatr Pol 2011;45:505-14. [PubMed]
- Hollen PJ, Gralla RJ, Kris MG, et al. A comparison of visual analogue and numerical rating scale formats for the Lung Cancer Symptom Scale (LCSS): does format affect patient ratings of symptoms and quality of life? Qual Life Res 2005;14:837-47. [Crossref] [PubMed]
- Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain 2003;4:407-14. [Crossref] [PubMed]
- Bagan P, Berna P, De Dominicis F, et al. Nutritional status and postoperative outcome after pneumonectomy for lung cancer. Ann Thorac Surg 2013;95:392-6. [Crossref] [PubMed]
- Gioulbasanis I, Baracos VE, Giannousi Z, et al. Baseline nutritional evaluation in metastatic lung cancer patients: Mini Nutritional Assessment versus weight loss history. Ann Oncol 2011;22:835-41. [Crossref] [PubMed]
- Mori S, Usami N, Fukumoto K, et al. The Significance of the Prognostic Nutritional Index in Patients with Completely Resected Non-Small Cell Lung Cancer. PLoS One 2015;10:e0136897. [Crossref] [PubMed]
- Dewys WD, Begg C, Lavin PT, et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med 1980;69:491-7. [Crossref] [PubMed]
- Jagoe RT, Goodship TH, Gibson GJ. Nutritional status of patients undergoing lung cancer operations. Ann Thorac Surg 2001;71:929-35. [Crossref] [PubMed]
- Gonzalez A, Japuntich S, Keating NL, et al. Pain experiences among a population-based cohort of current, former, and never regular smokers with lung and colorectal cancer. Cancer 2014;120:3554-61. [Crossref] [PubMed]
- Park S, Kang CH, Hwang Y, et al. Risk factors for postoperative anxiety and depression after surgical treatment for lung cancer†. Eur J Cardiothorac Surg 2016;49:e16-21. [Crossref] [PubMed]
- Giannousi Z, Gioulbasanis I, Pallis AG, et al. Nutritional status, acute phase response and depression in metastatic lung cancer patients: correlations and association prognosis. Support Care Cancer 2012;20:1823-9. [Crossref] [PubMed]
- Rueda JR, Solà I, Pascual A, et al. Non-invasive interventions for improving well-being and quality of life in patients with lung cancer. Cochrane Database Syst Rev 2011.CD004282. [PubMed]
- Reyes-Gibby CC, Swartz MD, Yu X, et al. Symptom clusters of pain, depressed mood, and fatigue in lung cancer: assessing the role of cytokine genes. Support Care Cancer 2013;21:3117-25. [Crossref] [PubMed]


