Temporary transection of innominate vein in surgery of midtracheal tumor
Introduction
Primary tracheal tumors are rare and should be resected if the tumor can be removed and if the trachea can be reconstructed safely. Variations in size and location cause difficulty during complete resection of the tumor with reconstruction of the trachea, especially in cases of some large midtracheal tumors. We report a rare case of midtracheal carcinoma, where, following a median sternotomy, complete removal of the tumor and tracheal reconstruction was performed satisfactorily with transection and reanastomosis of the left innominate vein (LIV).
Case report
A 41-year-old man with no significant medical history presented with productive cough for half a year and developed a paroxysmal dyspnea for five days. Emergent tracheostomy was performed in the Emergency Department. The symptoms of dyspnea were then relieved, and mechanical ventilation became unnecessary. After admission, the patient suffered from several incidents of hemoptysis with a maximum of 10 mL.
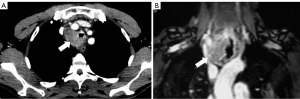
Chest computed tomography (CT) scan showed a 3.0 cm × 5.0 cm mass in the superior mediastinum (Figure 1A) involving the trachea. Magnetic resonance imaging (MRI) showed that the mass had an abundant blood supply (Figure 1B), and that it involved the trachea, brachiocephalic artery, and LIV. Bronchoscopy performed through the endotracheal tube demonstrated a midtracheal tumor, which caused infundibular stenosis. The tumor was confirmed as squamous cell carcinoma via bronchoscopic biopsy.
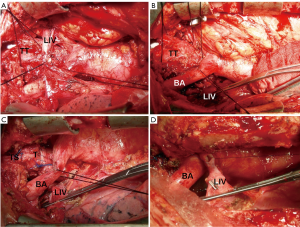
The operation was carried out under general anesthesia, and the patient was placed in supine position. Oral intubation was performed to replace the previous cervical tracheal intubation. After sternotomy, a 3.0 cm × 5.0 cm × 5.0 cm mass in the right superior mediastinum was found originating from the midtrachea, posterior to the LIV (Figure 2A). Intravenous heparin was administered through the left upper extremity to avoid blood coagulation when the LIV was temporarily blocked and transected (Figure 2B). The trachea was then carefully dissected with en block resection of the tumor. The 6th to 11th tracheal rings were also resected. A tube was inserted into the distal trachea through the operation field for temporary ventilation. Continuous end-to-end anastomosis was then performed using a 3-0 Prolene suture. The intubation in the distal trachea was replaced by the oral intubation before suturing the anterior wall of the midtrachea. Then, the tracheostomy fistula was closed (Figure 2C). The LIV was anastomosed with a running 5-0 Prolene suture (Figure 2D). Finally, we placed a mediastinal drainage tube.
The operation was uneventful. The patient recovered well and was discharged two weeks after surgery. Immunohistochemical analysis confirmed the diagnosis of moderately differentiated squamous cell carcinoma with metastasis of paratracheal lymph nodes. The reconstructed LIV continued to function properly during the two-month follow-up after surgery.
Discussion
Primary tracheal tumors are rare, and account for only about 0.1% of all malignancies (1). The most common tracheal malignancies are squamous cell carcinoma, followed by adenoid cystic carcinoma (2). Symptoms of primary tracheal tumors usually correlate with the size and invasion pattern of the tumor. The most common symptom of tracheal tumor is dyspnea, which appears when tumors occlude more than half of the tracheal tube (3). The most commonly used and helpful diagnostic method is chest CT or MRI combined with bronchoscopy rather than chest radiograph. Sometimes, a postoperative pathological evaluation is required to confirm the diagnosis.
Endobronchial stents that offer reliable and durable palliation in some properly selected patients are often useful for unresectable or medically inoperable lesions (4). However, surgical resection still remains the mainstay of treatment for benign and lesser tracheal malignancies (5). For upper-tracheal tumors, a cervical collar incision is recommended, and the upper sternum could be incised for better exposure. If the middle trachea is involved, Pearson et al. (6) recommended median sternotomy with a transpericardial approach. For most lower tracheal or carinal tumors, Grillo et al. (7) recommended right posterolateral thoracotomy.
In this case, we chose the median sternotomy approach because the tumor extended up to the neck. During the operation, we transected the LIV and pulled the brachiocephalic artery away from the tumor. This strategy provided excellent exposure and a suitable operating field for resection and reconstruction of the midtrachea. To avoid postoperative edema of the left upper extremity, face, and head, we decided to anastomose the transected LIV. As predicted, the patient recovered well without any severe complications. Most importantly, temporary transection of the LIV seems a reasonable alternative for surgical resection of this large cross-border midtracheal tumor.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Cai C, Jiang RC, Li ZB, et al. Two-stage tracheal reconstruction of primary tracheal non-Hodgkin lymphoma with nitino mesh stent and cervical myocutaneous flap. Ann Thorac Surg 2008;85:e17-9. [PubMed]
- Macchiarini P. Primary tracheal tumours. Lancet Oncol 2006;7:83-91. [PubMed]
- Gelder CM, Hetzel MR. Primary tracheal tumours: a national survey. Thorax 1993;48:688-92. [PubMed]
- Liu CC, Wang KM, Hsu LH. Tracheobronchial self-expanding metallic stent in patients with central airways obstruction. J Bronchol 2008;15:11-6.
- Honings J, Gaissert HA, van der Heijden HF, et al. Clinical aspects and treatment of primary tracheal malignancies. Acta Otolaryngol 2010;130:763-72. [PubMed]
- Pearson FG, Todd TR, Cooper JD. Experience with primary neoplasms of the trachea and carina. J Thorac Cardiovasc Surg 1984;88:511-8. [PubMed]
- Grillo HC, Mathisen DJ. Primary tracheal tumors: Treatment and results. Ann Thorac Surg 1990;49:69-77. [PubMed]


