Individualized clopidogrel suspension strategy coronary artery bypass surgery: what is the best choice?
We read with the interest the work of Mannacio et al. (1).
Recent guideline suggests clopidogrel suspension 5 days before non-emergent cardiac surgery (Class IIa, Level B); ticagrelor and prasugrel should be suspended after 3 and 7 days, respectively (Class IIa, Level B). Recommendations could not be extended to emergent and semi-elective urgent cases.
Conceptually, there are three types of patients’ population that we have to deal with see Figure 1:
- Patients for emergency coronary artery bypass surgery (CABG);
- Semi-elective and urgent CABG;
- Elective CABG.
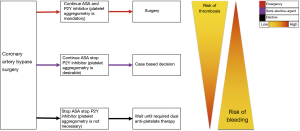
Patients’ management on double antiplatelet therapy (DAPT) who has been referred for surgical interventions mainly depends on emergency status and the thrombotic/bleeding risk of the every single patient [see list above and Figure 1, adopted from (2)].
Majority of surgical interventions can be performed on double or on aspirin alone with acceptable percentage or volume of bleeding (3). However, a multi-specialist approach is strictly required and necessary (for example cardiologist, anaesthesiologist, haematologist and surgeon) in order to be able to estimate the patients’ possible bleeding risk and to be confident to adopt the best/optimal available strategy based on single clinical case. After a certain experience an institutional protocol can be developed base and every single institution.
In preparation for surgery with high/very high bleeding risk patients, it is generally recommended that clopidogrel has to be discontinued 5 days before surgery in order to reduce bleeding and consequently the need for blood transfusion, while maintaining aspirin in perioperative period.
However, in our experience more than 90% cases of coronary artery bypass surgery cases is done in urgency or emergency regime (not published data).
Clopidogrel should be stopped (if intervention is programmable) 5 days and ticagrelor 3 days before the programmed surgical interventions. Prasugrel, however, should be stopped 7 days before since its prolonged and more effective platelet inhibition than clopidogrel demonstrated and documented in literature (2). In semi-elective and urgent cases, it is a best practice, if patients are not already in DAPT, to start immediately short half-life P2Y12 inhibitors infusion (for example tirofiban or eptifibatide). It is enough to suspend their infusion 4 hours before the surgery; this strategy is also supported by guidelines (2).
In emergency coronary artery bypass surgery there we suggest always do platelet aggregometry prior to surgery if possible, or in the operating room.
In semi-elective cases where there is more time available we suggest to do platelet aggregometry prior to surgery.
In elective cases when suspension of each component of DAPT is possible without adverse events, we believe platelet aggregometry is not necessary.
Withdrawal or suspension of P2Y12 receptor inhibitors is not generally recommended in high risk patients’ cohorts, such as those with ongoing ischaemia and high risk coronary artery anatomy (LM or severe multivessel disease), recent angioplasty for culprit lesion.
In our experience we follow the strategy designed on Figure 1.
This kind of patients should undergo coronary artery bypass surgery while maintaining P2Y12 receptor inhibitors, while paying particular and detailed attention to hemostasis and bleeding prevention. In our institution we rarely cancel postpone semi-elective or urgent case bases on antiaggregation profile.
It may be reasonable and prudent to suspend or withhold only in high risk patients the P2Y12 receptor inhibitors before surgical intervention. Dual antiplatelet therapy should be reintroduced as soon as possible (within 24 hours after surgery), although the optimal timing for resumption of therapy following bypass surgery remains to be defined and published in international guidelines; however, every institution should have its own internal protocols based their own experience.
Inhibitory response of thrombocytes to clopidogrel therapy determines bleeding after coronary artery bypass surgery, and a strategy based on preoperative aggregometry, in order to determine the timing of coronary artery bypass surgery, led to about 50% lesser waiting time than recommended in the current international guidelines (2). Therefore, the 2012 update of the Society of Thoracic Surgeons (STS) guidelines suggests that a postponing of even a few days might be reasonable, in order to decrease bleeding probability and thrombotic risk in acute coronary artery syndrome patients (4).
In very high risk situations, such as following few days of stent implantation, has been suggested that patients might be switched from clopidogrel to a reversible, and as a consequence, short acting platelets inhibitors (for example tirofiban, eptifibatide); suspending them 4 hours before surgery (2). Currently it is our strategy of choice for high risk patients with fresh stenting procedures.
In BRIDGE (Bridging Anticoagulation in Patients who Require Temporary Interruption of Warfarin Therapy for an Elective Invasive Procedure or Surgery) study, the usage of cangrelor was tested against a placebo (5). Oral P2Y12 receptor inhibitors were stopped in about 48 hours before coronary artery bypass surgery and cangrelor resulted in a higher rate of platelet inhibition. The change of DAPT with low molecular weight heparin or unfractionated heparin was resulted to be ineffective. In surgical procedures with low/moderate bleeding risk, surgeons should be encouraged to operate while maintaining DAPT; in our institution we approach critically the hemostasis in this category of patients.
Resuming clopidogrel therapy after coronary artery bypass surgery appears to be safe and effective according to a recent studies when clopidogrel was added to aspirin, as opposed to aspirin alone, showed a better early vein graft patency and lower in-hospital or 30-day mortality (2).
In summary, three above mentioned strategies suggest the best practice today in order to deliver best healcather today. We encourage the surgeons operate patients in emergency and elective conditions using aggregometry in order to be able to face problems and to find the best way to resolving them.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mannacio VA, Mannacio L, Pinna GB, et al. Individualized strategy for clopidogrel suspension in patients undergoing coronary surgery: is it the best choice? Eur J Cardiothorac Surg 2016;50:189-90. [Crossref] [PubMed]
- Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2018;39:213-60. [Crossref] [PubMed]
- van Diepen S, Fuster V, Verma S, et al. Dual Antiplatelet Therapy Versus Aspirin Monotherapy in Diabetics With Multivessel Disease Undergoing CABG: FREEDOM Insights. J Am Coll Cardiol 2017;69:119-27. [Crossref] [PubMed]
- Ferraris VA, Saha SP, Oestreich JH, et al. 2012 update to the Society of Thoracic Surgeons guideline on use of antiplatelet drugs in patients having cardiac and noncardiac operations. Ann Thorac Surg 2012;94:1761-81. [Crossref] [PubMed]
- Douketis JD, Kaatz S. Bridging Anticoagulation in Patients Who Require Temporary Interruption of Warfarin for Surgery. In: Crowther et al. editors. Evidence-Based Hematology. Hoboken: John Wiley & Sons, 2009;24-30.


