Durvalumab after chemo-radiotherapy in stage III non-small cell lung cancer
Lung cancer is the most common cause of death worldwide. Non-small cell lung cancer (NSCLC) accounts for 85% of lung cancer and a third of NSCLC patients present with unresectable locally advanced disease (1). Concurrent chemo-radiotherapy [CRT (platinum-based doublet chemotherapy concurrent with RT)] is the standard treatment option for unresectable stage III NSCLC (2-4). Median progression free survival (PFS) for unresectable stage III disease is approximately 8 months and the 5-year survival rate is 15%.
Recent studies incorporating modern RT techniques and use of positron emission tomography-computed tomography (PET-CT) for staging have reported a median OS of 24 months for inoperable stage III NSCLC receiving concurrent CRT. Despite treatment is given with curative intent, 50% of patients will relapse with distant disease (5). Efforts to improve survival with induction or consolidation chemotherapy have failed to improve outcomes (6,7). A pooled analysis of the literature showed that consolidation chemotherapy following concurrent chemoradiotherapy doesn’t improve OS in unresectable locally advanced NSCLC (8).
Immune Checkpoint inhibitors targeting programmed death 1 (PD-1) and programmed death ligand 1 (PD-L1) now represent a standard option for advanced NSCLC. To date, Nivolumab, Pembrolizumab and Atezolizumab have been approved by FDA and EMA as a treatment option for pre-treated patients with advanced NSCLC. Pembrolizumab is also licensed as first-line treatment for advanced NSCLC patients with PD-L1 expression ≥50% (9).
Durvalumab (imfinzi) is a selective, human immunoglobulin G1 kappa (IgG1k) monoclonal antibody that blocks the interaction of PD-L1 with the PD-1 and CD-80 molecule. In a phase 1 trial durvalumab showed tolerability and efficacy irrespective of PD-L1 status (10). The recently reported ATLANTIC study (11,12) showed the activity of durvalumab in a heavily pre-treated (≥3 lines) NSCLC population.
PACIFIC is a phase III randomized, double-blind study comparing durvalumab vs. placebo as consolidation therapy with placebo in patients with stage III, locally advanced, unresectable NSCLC (according to TNM 7th edition) that had not progressed after platinum-based concurrent CRT. Eligible patients had ECOG PS of 0-1 and received two or more cycles of platinum-based doublet chemotherapy (containing etoposide, vinblastine, vinorelbine, taxane, pemetrexed) with concurrent radiotherapy (54–66 Gy) (13). The median age was 64 years and 91% patients were current or ex-smokers. PD-L1 expression was analyzed on archival tumour samples obtained before chemo-radiotherapy. About 22% patients had PD-L1 expression of ≥25% and 41% of patients had PD-L1 expression of <25%. PD-L1 expression was unknown in 36.7% patients. A total of 709 patients were randomized to receive durvalumab (10 mg/kg) or placebo every 2 weeks for up to 12 months. The co-primary endpoints were PFS (assessed by the blinded independent central review) and overall survival (OS), both calculated from the time of randomization.
The pre-planned interim analysis showed a median PFS of 16.8 [95% confidence interval (CI), 13.0–18.1] vs. 5.6 (95% CI, 4.6–7.8) months for durvalumab and placebo, respectively (HR for disease progression or death, 0.52; 95% CI, 0.42–0.65; P<0.0001). Improvement on PFS was seen irrespective of PD-L1 expression and was consistent across all pre-specified subgroups. The secondary endpoints of time to death or distant metastasis (23 vs. 14.6 months) and objective response rate (28.4% vs. 16%) were also improved with durvalumab. The incidence of new brain metastasis was also lower in the durvalumab arm (5.5% vs. 11%). The incidence of treatment-related adverse events (AEs) was slightly higher in the durvalumab arm (67.8% vs. 53.4%). Immune-related AEs were also more common in the experimental arm (24.2% vs. 8.1%) but it was reassuring to see there was no significant difference in the rates of severe immune-related AEs and pneumonitis between the two groups.
With survival benefit reaching a plateau with current CRT strategies, the introduction of immunotherapy into the treatment of locally advanced NSCLC has been enthralling. Immune checkpoint blockade has shown anti-tumor response and OS benefit in advanced NSCLC with long-term control achievable in a subset of patients (14). Radiation-induced tumour necrosis results in the release of tumor antigen inducing an anti-tumor response through upregulation of immunogenic cell surface markers. In the metastatic setting, the immunomodulatory effect of radiotherapy may enhance local control as well as systemic antitumor immune response. The inflammatory changes induced by RT may lead to the release of cytokines and infiltration of a tumour specific T cells (10).
RT enhances the immune system by directly upregulating tumor-associated antigen and MHC class 1 surface expression. Furthermore, RT stimulates the immune system via activating dendritic cells, increasing antigen presentation and modifying the tumor microenvironment. Several pre-clinical studies have already demonstrated that checkpoint inhibitors enhance the immunomodulatory effects of RT (15-18). In a mouse model, Dewann et al. tested the hypothesis that dose fractionation determines the synergistic ability of radiotherapy with CTLA4. This study concluded that fractioned RT induces significant growth inhibition of a tumor outside of the radiation field (19).
In the phase I KEYNOTE-001 (NCT01295827) study, a secondary analysis of 98 patients with advanced NSCLC demonstrated longer PFS and OS in the subgroup of patients who had previously received RT compared to patients who had not (20). This synergistic effect of immunotherapy and RT on both local and distant tumor control provides a strong rationale for introducing immunotherapy into protocols for locally advanced NSCLC.
Aside from PACIFIC, there is limited data that examines the role of consolidation immunotherapy following CRT in unresectable stage III NSCLC. START, a phase III randomized double-blind study randomized patients with stable disease or objective response after CRT (patients must have completed at least two cycles of platinum-based chemotherapy, given sequentially or concurrently, with a minimum of 50 Gy of radiation) to tecemotide, a mucin 1 antigen-specific cancer vaccine, or placebo. No significant difference in OS (25.6 vs. 22.3 months, HR =0.88; (95% CI, 0.75–1.03) or time to progression (10 vs. 8.4 months, HR =0.87; (95% CI, 0.75–1.00); P=0.053) was observed between the two groups. Notably, a subgroup analysis for patients who received concurrent CRT demonstrated longer OS in the tecemotide group compared to placebo (30.8 vs. 20.6 months, HR =0.78, P=0.016). This difference was not found in the group of patients who received sequential chemo-radiotherapy (19.4 vs. 24.6 months, HR =1.12, P=0.038) (21).
At present, further data is needed to clarify the relevance of timing of immune checkpoint blockade with chemotherapy and thoracic radiotherapy and several clinical trials are ongoing (Table 1).
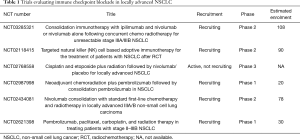
Full table
OS remains the most clinically relevant endpoint for trials in locally advanced NSCLC. PFS has been demonstrated to be a valid surrogate endpoint for OS in studies of locally advanced NSCLC patients treated with chemotherapy and thoracic RT (22). For this reason, even if OS data is still immature, the unprecedented benefit in PFS demonstrated by durvalumab warrants consideration as a new standard of care for patients treated with concurrent chemo-radiotherapy. Until further data is available, we feel that this data cannot be extrapolated to justify the use of durvalumab as consolidation therapy for patients treated with sequential chemotherapy and radiotherapy to the chest.
Acknowledgements
None.
Footnote
Conflicts of Interest: R Califano has received honoraria for consultancy and advisory boards from AstraZeneca/Medimmune. Other authors have no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin 2017;67:7-30. [Crossref] [PubMed]
- Furuse K, Fukuoka M, Kawahara M, et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with mitomycin, vindesine, and cisplatin in unresectable stage III non-small-cell lung cancer. J Clin Oncol 1999;17:2692-9. [Crossref] [PubMed]
- Albain KS, Swann RS, Rusch VW, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomised controlled trial. Lancet 2009;374:379-86. [Crossref] [PubMed]
- Curran WJ Jr, Paulus R, Langer CJ, et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: randomized phase III trial RTOG 9410. J Natl Cancer Inst 2011;103:1452-60. [Crossref] [PubMed]
- Senan S, Brade A, Wang LH, et al. PROCLAIM: Randomized Phase III Trial of Pemetrexed-Cisplatin or Etoposide-Cisplatin Plus Thoracic Radiation Therapy Followed by Consolidation Chemotherapy in Locally Advanced Nonsquamous Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:953-62. [Crossref] [PubMed]
- Vokes EE, Herndon JE 2nd, Kelley MJ, et al. Induction chemotherapy followed by chemoradiotherapy compared with chemoradiotherapy alone for regionally advanced unresectable stage III Non-small-cell lung cancer: Cancer and Leukemia Group B. J Clin Oncol 2007;25:1698-704. [Crossref] [PubMed]
- Hanna N, Neubauer M, Yiannoutsos C, et al. Phase III study of cisplatin, etoposide, and concurrent chest radiation with or without consolidation docetaxel in patients with inoperable stage III non-small-cell lung cancer: the Hoosier Oncology Group and U.S. Oncology. J Clin Oncol 2008;26:5755-60. [Crossref] [PubMed]
- Tsujino K, Kurata T, Yamamoto S, et al. Is consolidation chemotherapy after concurrent chemo-radiotherapy beneficial for patients with locally advanced non-small-cell lung cancer? A pooled analysis of the literature. J Thorac Oncol 2013;8:1181-9. [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Berman AT, Simone CB 2nd. Immunotherapy in locally-advanced non-small cell lung cancer: releasing the brakes on consolidation? Transl Lung Cancer Res 2016;5:138-42. [PubMed]
- Garassino MC, Vansteenkiste J, Kim JH, et al. Durvalumab in ≥3rd-Line Locally Advanced or Metastatic, EGFR/ALK Wild-Type NSCLC: Results from the Phase 2 ATLANTIC Study. Available online: http://www.jto.org/article/S1556-0864(16)31253-9/fulltext
- Garassino M, Cho B, Gray JE, et al. Durvalumab in ≥ 3rd-line EGFR mutant/ALK+, locally advanced or metastatic NSCLC: Results from the phase 2 ATLANTIC study. Ann Oncol 2017;28:ii28-51. [Crossref]
- Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after Chemoradiotherapy in Stage III Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:1919-29. [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Postow MA, Callahan MK, Barker CA, et al. Immunologic correlates of the abscopal effect in a patient with melanoma. N Engl J Med 2012;366:925-31. [Crossref] [PubMed]
- Deng L, Liang H, Burnette B, et al. Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest 2014;124:687-95. [Crossref] [PubMed]
- Sharabi AB, Nirschl CJ, Kochel CM, et al. Stereotactic Radiation Therapy Augments Antigen-Specific PD-1-Mediated Antitumor Immune Responses via Cross-Presentation of Tumor Antigen. Cancer Immunol Res 2015;3:345-55. [Crossref] [PubMed]
- Dovedi SJ, Adlard AL, Lipowska-Bhalla G, et al. Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res 2014;74:5458-68. [Crossref] [PubMed]
- Dewan MZ, Galloway AE, Kawashima N, et al. Fractionated but not single-dose radiotherapy induces an immune-mediated abscopal effect when combined with anti-CTLA-4 antibody. Clin Cancer Res 2009;15:5379-88. [Crossref] [PubMed]
- Shaverdian N, Lisberg AE, Bornazyan K, et al. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol 2017;18:895-903. [Crossref] [PubMed]
- Butts C, Socinski MA, Mitchell PL, et al. Tecemotide (L-BLP25) versus placebo after chemoradiotherapy for stage III non-small-cell lung cancer (START): a randomised, double-blind, phase 3 trial. Lancet Oncol 2014;15:59-68. [Crossref] [PubMed]
- Mauguen A, Pignon JP, Burdett S, et al. Surrogate endpoints for overall survival in chemotherapy and radiotherapy trials in operable and locally advanced lung cancer: a re-analysis of meta-analyses of individual patients' data. Lancet Oncol 2013;14:619-26. [Crossref] [PubMed]


