Sleep-disordered breathing in the elderly: is it distinct from that in the younger or middle-aged populations?
Introduction
Sleep-disordered breathing (SDB) is characterized by repetitive suspension or reduction of breathing, causing nocturnal intermittent hypoxia, which is followed by re-oxygenation. There is a growing evidence that SDB, particularly obstructive sleep apnea (OSA), is associated with cardiovascular (CV) risk factors, morbidity and mortality (1). Continuous positive airway pressure (CPAP) is the gold-standard for management of SDB, and its adequate use has a remarkable efficacy in the management of CV diseases (1). Currently, the data available regarding SDB is related to young or middle-aged patients and there is a lack of evidence in the elderly. Hence, there is a critical need for large scale population-based studies and clinical trials involving a broad range of elderly patients who represent the real-world patients in the aging society (2). The relationship between SDB and CV risk factors, morbidity, and mortality in the elderly still remains to be explored.
The prevalence and characteristics of SDB in the elderly
The prevalence of SDB is high in elderly patients, while its prevalence in general population varies from 20% to 40%; that is a large variation and a more conservative estimate would suggest that the prevalence of SDB in elderly patients is at least double of that seen in the younger population (3). According to a cross-sectional study involving 741 men aged >20 years [mean body mass index (BMI): 26.9], the prevalence of SDB [apnea hypopnea index (AHI) >10] increased with age (20–44 years: 3.2%; 45–64 years: 11.8%; 65–100 years: 23.9%), while the odds ratio of the prevalence of SDB in the oldest age group (65–100 years) compared with the middle age group was 2.3 (4). Furthermore, a separate analysis of 1,000 women (mean BMI: 29.6) from the same cohort revealed that the prevalence of SDB was highest among the oldest group of women (5). In a community-based longitudinal study, which followed 30 patients (mean entry age: 57.8 years) for 23.4 years, the rates of change in AHI were characterized by positive slopes along with aging; the mean rate of change was +0.43 events per hour per year (6). These findings suggest that aging is one of the significant predictors of SDB. In addition to the correlation between SDB and aging, there are several unique characteristics of elderly SDB. First, the effect of obesity on risk for SDB in elderly, was lower than that in other age groups (7). A review article which evaluated the interaction between SDB and obesity noted that this interaction in elderly subjects differed from that in younger adults. The risk of SDB between overweight (BMI: 25–29.9 kg/m2) and normal-weight (BMI: 20–24.9 kg/m2) groups in the elderly was not different (7). Secondly, self-reported breathing pause or snoring was less prevalent in the elderly than in middle-aged individuals with SDB (8). Therefore, it can be suggested that, SDB in the elderly is quite common, but is under-recognized partly due to the absence of some well-known signs of SDB (e.g., obesity, breathing pause, and snoring).
Impact of SDB on cognitive function, CV morbidity and mortality in the elderly
Despite its high prevalence, the distinct phenotype of SDB in elderly has led to the debate on its clinical implications on aspects such as cognitive function, CV morbidity and mortality in elderly patients. Several studies have suggested that SDB is associated with the occurrence of cognitive impairment. Among 298 older women (mean age: 82.3 years), those with SDB, had an increased risk of developing cognitive impairment, compared to those without SDB (9). A 5-year population-based cohort study involving nearly 8,000 subjects, also demonstrated that SDB patients had 1.70-times greater risk of developing dementia compared to age- and sex-matched non-SDB patients, and its statistical significance persisted in the 50–59 [adjusted hazard ratio (HR): 3.63; 95% CI, 1.67–7.88] years old and ≥70 (adjusted HR: 1.53; 95% CI, 1.01–2.33) years old groups (10). Because of the limited data on the relationship between SDB and CV morbidity or mortality in the elderly, the applicability of the results derived from the younger or middle-aged population is uncertain. According to the Sleep Heart Health Study (SHHS), a multi-center prospective cohort study, which followed 4,422 adults for a median of almost 9 years, the statistical association between increased risk of coronary artery disease (myocardial infarction, revascularization procedure, or coronary heart disease death) and untreated SDB appeared stronger in men aged ≤70 years than men >70 years (11). In contrast to the association with coronary artery disease, both the men older and younger than 70 years with severe untreated SDB, exhibited a trend toward higher incidence of heart failure than men of the same age who did not have SDB (11).
The data related to the impact of SDB on mortality in the elderly is limited and inconsistent. A retrospective cohort study revealed that elderly patients (≥65 years) with severe SDB (respiratory disturbance index >40) had the same mortality as the age-, gender-, and ethnicity-matched general population cohorts (12). Another population-based probability sample of 426 elderly individuals (mean age: 72.5 years) reported that only age, CV disease and pulmonary disease, but not the degree of SDB, were independent predictors of death (13). A prospective cohort study from the SHHS, which followed 6,294 adults for a median of almost 8 years, revealed that statistical association between all-cause mortality and untreated SDB noted in men younger than 70 years (n=2,169), was not evident in men over 70 years (n=773) and in women of any age (n=3,352) (14). Conversely, another prospective cohort which followed 939 older patients (≥65 years) being evaluated for suspected OSA for 69 months, revealed that the patients with untreated severe SDB (AHI ≥30) had an increased risk of all-cause and CV mortality (15). Although the reasons for these discrepancies remains unknown, it might be due to the difference in study population (population- or clinically-based) and CV risk profile. Nevertheless, most of the evidence related to elderly is from the subgroups of studies that include adults of all ages, which did not have enough events to either confirm or exclude the clinical significance of SDB in terms of CV morbidity and mortality in the elderly.
There also has been limited evidence for SDB treatment in elderly patients, with only few randomized control trials (RCTs) specifically related to the elderly. In the observational cohort study of elderly patients (≥65 years) mentioned earlier, the risk of CV mortality reduced to a greater extent in the group with severe SDB which used CPAP compared to the group with severe SDB without CPAP therapy (15). Two recent RCTs have focused specifically on the elderly. One was an open-labelled randomized treatment with CPAP in 224 elderly patients with severe OSA (≥70 years; mean entry age: 75.5 years) which demonstrated the effectiveness of CPAP in improving the quality of life, sleep apnea-related symptoms, symptoms of depression and anxiety, and certain neurocognitive aspects (16). The PREDICT study, was the other 12-month, multicenter, randomized trial involving 278 elderly patients with OSA syndrome (≥65 years; mean entry age: 71.1 years), which revealed that CPAP reduced objective sleepiness and was cost-effective among older people. The incidence of new CV events did not differ between groups at 3 and 12 months (17).
Impact of SDB on CV risk factors in the elderly
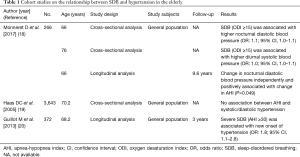
Few studies have simultaneously followed the parameters of CV risk factors and SDB in elderly subjects. We read with interest Dr. Monneret et al.’s article “Serum lipid profile, sleep-disordered breathing and blood pressure in the elderly: a 10-year follow-up of the PROOF-SYNAPSE cohort” published in November 2017 in the Sleep Medicine (18). This study was designed to follow the evolution of the serum lipid profile and its relationships with SDB and blood pressure (BP) in healthy elderly individuals who were followed by general practitioners (18). The study conducted cross-sectional analyses at the two point; at the pre- and post-cohort of the trial for the same participants. Furthermore, the participants were followed for 10 years as a longitudinal cohort study for assessing the association between change of BP, serum lipid profile, and SDB severity. The study included 266 subjects with a mean age of 66 years and 44% women. The nocturnal oxygen desaturation index, a surrogate marker of SDB, was the main predictor of the likelihood of having hypertension at baseline and follow-up (Table 1). The nocturnal oxygen desaturation index increased (mean +2.3±6.7 events/hour) between 66 and 76 years of age. However, these variations were not associated with serum lipid variations, with or without lipid-lowering treatments. While the BP decreased in the overall group mainly due to an increased use of antihypertensive drugs, systolic BP increased in the absence of antihypertensive treatments. The relationship between SDB and hypertension was supported by the positive correlation between changes in nocturnal diastolic BP and AHI during the observation period (Table 1) (18).
Full table
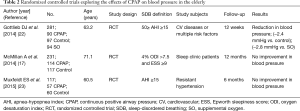
Despite the significant impact of SDB on the development of CV risk factors in younger or middle-aged populations (1), the association between SDB and hypertension, the most common CV risk factors, is controversial in the elderly. Table 1 summarize several incongruous evidences related to their correlation in the elderly. In the cross-sectional analysis of 6,120 participants from the SHHS, SDB was not associated with hypertension in subjects older than 60 years (19). On the contrary, the presence of severe OSA was associated with new onset hypertension after a period of 3 years in the normotensive elderly (PROOF-SYNAPSE cohort, mean age: 68.2 years) (20). A meta-analysis of 51 studies (4,888 patients) demonstrated that both CPAP and mandibular advancement devices were associated with reductions in BP (21); however, there were only 9 studies involving patients with a mean age ≥60 years (most of which had small sample size). Top three studies with the highest number of patients are listed in Table 2. Two randomized trials reported no significant difference in the changes in BP between CPAP therapy and non-CPAP therapy groups (17,23), whereas one RCT exhibited more effective BP reduction following CPAP therapy (22). In terms of the lipoprotein metabolism, the SHHS study demonstrated that the association between SDB and cholesterol level diminished in older individuals, while there was a trend of a modestly higher cholesterol in men <65 years with severe SDB (24). In the PREDICT study, significant improvement in total cholesterol levels was noted at 3 months in the CPAP group; but was not sustained at 12 months. There may be several unknown factors in the elderly which influence the interactions between serum lipid profile, SDB, and hypertension. Therefore, more and larger cohort studies are warranted clarify these interactions.
Full table
Key points in the management of SDB in the elderly
The limited but emerging evidence regarding SDB in elderly has led researchers to consider whether SDB in elderly individuals is distinct from that in middle-aged people. The key points in the management of SDB in the elderly depending on the clinical endpoints such as patient-reported outcome, intermediate CV endpoints, and CV mortality can be summarized as follows. The main aim of SDB treatment in the elderly is to improve quality of life and well-being. Despite the lower prevalence of daytime sleepiness due to fragmented sleep, which is common in the elderly (3), medical providers still need to be careful about the presence of daytime sleepiness as a therapeutic target in the SDB management in elderly. The treatment of SDB with CPAP improves intermediate CV endpoints, such as blood pressure and cardiac ejection fraction in middle-aged population (1), but these effects were not established in the elderly population. In middle aged population with OSA, CPAP has been shown to reduce blood pressure levels (1), but not in OSA patients who were minimally symptomatic (25), which is one of the characteristics of elderly SDB. Further studies to evaluate whether the impact of CPAP on hypertension in elderly with SDB could be modulated by the presence of SDB-related symptom are required. Current data from large-scale RCTs do not support the role of CPAP treatment in the reduction of CV mortality, even in younger or middle-aged populations (1). Collectively, it can be suggested that CPAP treatment has not proved its efficacy in terms of major clinical endpoints in the elderly, despite its efficacy in patient-reported outcomes.
In addition to clinical endpoints, issues related to aging should also be considered. For instance, shorter life expectancy could modify the economic benefits of CPAP in the elderly; therefore, the magnitude of treatment and economic benefits of CPAP shown in middle-aged populations cannot be extrapolated to older populations. Additionally, inadequate CPAP adherence, which is known to be more apparent in elderly individuals, might dilute the significant effect and hence, a strategy to improve adherence in elderly should also be considered. Furthermore, because of the anatomical and physiological predisposition for developing SDB with increasing age (3), elderly SDB patients could be heterogeneous. Therefore, careful identification of subgroups among the elderly who are most likely to respond to CPAP, might be the key to establish the efficacy of CPAP in this population.
In conclusion, despite high prevalence of SDB in elderly, as well as, its worsening during aging, there is uncertainty about the relationship between SDB and CV risk factors, morbidity, and mortality. Further research is needed to clarify the impact of CPAP treatment on clinical outcomes including CV risk factors, morbidity, and mortality in elderly with SDB.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Javaheri S, Barbe F, Campos-Rodriguez F, et al. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. J Am Coll Cardiol 2017;69:841-58. [Crossref] [PubMed]
- Rich MW, Chyun DA, Skolnick AH, et al. Knowledge Gaps in Cardiovascular Care of the Older Adult Population: A Scientific Statement From the American Heart Association, American College of Cardiology, and American Geriatrics Society. Circulation 2016;133:2103-22. [Crossref] [PubMed]
- McMillan A, Morrell MJ. Sleep disordered breathing at the extremes of age: the elderly. Breathe (Sheff) 2016;12:50-60. [Crossref] [PubMed]
- Bixler EO, Vgontzas AN, Ten Have T, et al. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 1998;157:144-8. [Crossref] [PubMed]
- Bixler EO, Vgontzas AN, Lin HM, et al. Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 2001;163:608-13. [Crossref] [PubMed]
- Bliwise DL, Colrain IM, Swan GE, et al. Incident sleep disordered breathing in old age. J Gerontol A Biol Sci Med Sci 2010;65:997-1003. [Crossref] [PubMed]
- Romero-Corral A, Caples SM, Lopez-Jimenez F, et al. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 2010;137:711-9. [Crossref] [PubMed]
- Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med 2002;162:893-900. [Crossref] [PubMed]
- Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011;306:613-9. [PubMed]
- Chang WP, Liu ME, Chang WC, et al. Sleep apnea and the risk of dementia: a population-based 5-year follow-up study in Taiwan. PloS One 2013;8:e78655. [Crossref] [PubMed]
- Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation 2010;122:352-60. [Crossref] [PubMed]
- Lavie P, Lavie L. Unexpected survival advantage in elderly people with moderate sleep apnoea. J Sleep Res 2009;18:397-403. [Crossref] [PubMed]
- Ancoli-Israel S, Kripke DF, Klauber MR, et al. Morbidity, mortality and sleep-disordered breathing in community dwelling elderly. Sleep 1996;19:277-82. [Crossref] [PubMed]
- Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 2009;6:e1000132. [Crossref] [PubMed]
- Martínez-García MA, Campos-Rodríguez F, Catalán-Serra P, et al. Cardiovascular mortality in obstructive sleep apnea in the elderly: role of long-term continuous positive airway pressure treatment: a prospective observational study. Am J Respir Crit Care Med 2012;186:909-16. [Crossref] [PubMed]
- Martínez-García MÁ, Chiner E, Hernández L, et al. Obstructive sleep apnoea in the elderly: role of continuous positive airway pressure treatment. Eur Respir J 2015;46:142-51. [Crossref] [PubMed]
- McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Respir Med 2014;2:804-12. [Crossref] [PubMed]
- Monneret D, Barthélémy JC, Hupin D, et al. Serum lipid profile, sleep-disordered breathing and blood pressure in the elderly: a 10-year follow-up of the PROOF-SYNAPSE cohort. Sleep Med 2017;39:14-22. [Crossref] [PubMed]
- Haas DC, Foster GL, Nieto FJ, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation 2005;111:614-21. [Crossref] [PubMed]
- Guillot M, Sforza E, Achour-Crawford E, et al. Association between severe obstructive sleep apnea and incident arterial hypertension in the older people population. Sleep Med 2013;14:838-42. [Crossref] [PubMed]
- Bratton DJ, Gaisl T, Wons AM, et al. CPAP vs Mandibular Advancement Devices and Blood Pressure in Patients With Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. JAMA 2015;314:2280-93. [Crossref] [PubMed]
- Gottlieb DJ, Punjabi NM, Mehra R, et al. CPAP versus oxygen in obstructive sleep apnea. N Engl J Med 2014;370:2276-85. [Crossref] [PubMed]
- Muxfeldt ES, Margallo V, Costa LM, et al. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: a randomized controlled trial. Hypertension 2015;65:736-42. [Crossref] [PubMed]
- Newman AB, Nieto FJ, Guidry U, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol 2001;154:50-9. [Crossref] [PubMed]
- Bratton DJ, Stradling JR, Barbé F, et al. Effect of CPAP on blood pressure in patients with minimally symptomatic obstructive sleep apnoea: a meta-analysis using individual patient data from four randomised controlled trials. Thorax 2014;69:1128-35. [Crossref] [PubMed]


