Latest development of liquid biopsy
Introduction
Biopsy is obtaining tissue samples from a lesion for detecting a pathological process. Traditionally, biopsy could be classified as needle biopsy, incisional and excisional biopsy. Taking tissue biopsy is thus generally an invasive procedure. Aspiration cytology is a less invasive procedure to obtain cytology samples from the pathological lesion. With the advance of personalized cancer therapy, samples obtained from the cancer tissues are many a times not only used for diagnostic purposes, but also for detecting predictive biomarkers. Thus, there is increasing demand to obtain adequate sample for detection of the ever expanding repertoire of biomarkers. Furthermore, when patients develop resistance to targeting therapy, obtaining additional cancer samples, preferably from the resistance clone, is critical to delineate the resistance mechanism in guiding appropriate treatment. However, obtaining tissue or cytology sample may often require invasive procedures or may be practically impossible.
The advance in liquid biopsy allows an alternative and attractive non-invasive procedure to obtain biomaterials from cancers for diagnosis. Liquid biopsy would be defined as obtaining circulating cancer cells, tumor-derived cell free DNA (cfDNA) or other compounds in body fluids. The body fluids not only include peripheral blood, but also others, like urine, cerebrospinal fluid, or effusion fluids. However, it is most commonly refer to peripheral blood, and the current review is focused and limited to this scope.
Although the application of liquid biopsy into clinical use in cancer patients is relatively recent, the concept of its utility in cancer diagnosis has been there for many years. Elevated DNA levels were detected by radioimmunoassay in cancer patients in 1977 (1). A 1983 study determined that elevated DNA levels coupled with high circulating carcinoembryonic antigen (CEA) may be useful to diagnose gastrointestinal tract cancer (2). In this review, we discuss the current understanding and latest advances of this diagnostic method.
Traditional biopsy is limited by the amount of the tissue that can be sampled, which in turn is limited by the size of instrument used and the areas of sampling that can be achieved. Counterintuitively, a fine needle aspiration biopsy may be able to yield more diagnostic materials than a thick bore core needle because the fine needle can enter the suspicious mass in different angles, such that more parts of the lesion can be sampled. Apart from the invasiveness of these procedures, intra-tumoral heterogeneity is always a potential issue on the accuracy of a tissue biopsy (3-6). Any parts of the tumor can in theory shed materials into the bloodstream, be they nucleic acid, protein, secretory vesicles (such as exosomes), or tumor cells (Table 1). Thus, it is suggested that liquid biopsy may provide an even more representative sampling of the biomaterials from cancer (30).

Full table
Liquid biopsy in detecting tumor-derived circulating cfDNA—diagnostic potential
It was hypothesized that circulating cell-free DNA (cfDNA) is produced by tumor cell apoptosis or necrosis (31). The concept of detecting tumor-derived DNA in peripheral blood is not entirely new. For examples, the detection of circulating gene promotor methylation in serum of gastric and colorectal cancer patients has been reported (9,10). In addition, tumor-associated virus could also be a useful biomarker for cancer detection. For example, detecting circulating Epstein-Barr virus (EBV) DNA in blood has been established as a tumor marker for nasopharyngeal carcinoma (NPC) (11). In the context of lung cancer, similar to NPC, high level of circulating EBV DNA could be detected in lymphoepithelial-like carcinoma of lung, a rare lung cancer subtype (12,13). These suggest that tracing the circulating cell-free viral DNA may be useful in cancer screening and detecting cancer recurrence.
With the advances of cancer targeting therapy, the current interest is focusing on detecting critical gene mutations, be they driver mutation, resistance mutation or mutations that may be potentially actionable. While liquid biopsy has an advantage of being safe and easy to collect, the level of tumor-derived DNA is usually very low. In this regard, the major hurdle in liquid biopsy lies not in sampling but in the sample analysis. To differentiate circulating tumor DNA from DNA derived from normal cells, sensitive methods are required to detect cancer-specific genetic aberrations (Table 2).
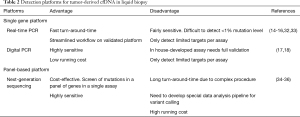
Full table
Allele-specific PCR [also known as amplification refractory mutation system (ARMS)], digital PCR or quantitative PCR are examples (37). These methods require the mutations to be well characterized, so that allele-specific primers (as in ARMS) or probes (as in digital PCR) can be designed specifically for the mutation at the specific locus. There were several attempts to detect mutations in cfDNA on various cancer types, such as KRAS (e.g., G12V, G12C, G12V, G13D) and BRAF (V600E) in colon cancer (23,38-40), or PIK3CA (E545K, H1047R, H1047L) in breast cancer (14). However, most of the developments were research-based and extensive validation was needed before putting them into clinical use. The first FDA approval on cfDNA-based liquid biopsy only occurred relatively recently, in June 2016 (32). This allele-specific PCR test was developed by Roche (Cobas cfEGFR Test) for detection of 42 EGFR mutations in peripheral blood for non-small cell lung cancer (NSCLC). EGFR mutation is the first actionable mutation discovered in NSCLC, in particular adenocarcinoma (ADC) that can be targeted by small molecule inhibitors. The prevalence of EGFR mutation varies among ethical and geographic group and being much higher in Asian population, it accounts for up to 40% to 60% in Lung ADC in Asian countries (33). Comparing to tissue genotyping result, the specificity for this blood EGFR test ranges from 82% to 96%, and the sensitivity ranges from 60.7% to 76% (15,16). However, the sensitivity in detecting T790M is lower (15,16). The reason for this lower sensitivity in detecting T790M mutation is not entirely clear. However, it may be attributed to that only a subpopulation of cancer cells harbors this resistance mutation (41).
To improve the sensitivity of detecting tumor-derived DNA in blood, digital PCR platform has been investigated. It could be chip-based or droplet based. The specificity for EGFR L858R and 19del mutation detection is up to 100% while the sensitivity ranges from 74% to 82%, depending of the mutation types (17). The sensitivity in detecting T790M is improved in this platform with a 77% sensitivity (17).
Apart from EGFR mutation, liquid biopsy for BRAF mutation is also under active investigations. This is particularly relevant to lung cancer as BRAF inhibitors are available for treatment and have been approved for treating metastatic non-small cell lung cancer with V600E mutation (42). BRAF mutation detection in the peripheral blood can be achieved by digital PCR (18).
With the advances of personalized molecular targeting therapy, one could anticipate more actionable gene mutations to become potential candidates for liquid biopsy detection. Thus, a gene panel testing becomes an attractive approach. A number of next-generation sequencing based gene panels are currently available for tissue samples (34-36). Such gene panel approach is also applicable in the setting of liquid biopsy (19). However, the sensitivity is still relatively low.
Liquid biopsy in detecting tumor-derived circulating cfDNA—disease monitoring and detecting recurrence
When a mutation can be characterized for the primary cancer, the detection of such a specific mutation for a particular patient may be utilized as disease monitoring or detecting recurrence. This personalized medicine approach of cancer patient follow-up is exemplified by several studies (24-26,37). Diehl et al. reported that detection of APC, KRAS, PIK3CA, and TP53 mutation in cfDNA in post-operative plasma in colorectal cancer patients who had undergone surgery was highly predictive of recurrence (24). According to Garcia-Murillas et al.’s study, for breast cancer patients, using mutation-specific digital PCR in tracking mutation in follow-up blood samples was useful in predicting early relapse (25).
Liquid biopsy in detecting tumor-derived circulating cfDNA—implication in cancer screening
Recently, a cancer screening algorithm was developed to detect eight common cancer types, by using a panel of 16 genes, such as EGFR, APC, KRAS, and TP53 (43). After an initial round of gene amplification, the samples were subjected to parallel sequencing with next generation sequencing platforms. Together with proteomics information, the algorithm was able to detect cancer with 69–98% sensitivity, with very low false negativity (7/812 subjects). The authors reasoned that the performance and the relatively low cost were major advantages of this strategy. Understandably, the relative small number of genes being tested and the overlapping spectrum of mutations that can occur in different tumors made it difficult to ascertain the causative cancer type. The authors resolved this issue by calculating the probability of each cancer type that the patient may have, by taking into account of the mutation type, patient age and sex, and other serological markers such as CEA. Although intriguing, the corollary of this strategy is that apart from molecular testing, clinical information and patient demographics are still indispensable in arriving a possible correct diagnosis.
For cancer screening, one concern is that being increasing in sensitivity, screening assays may eventually pick up mutant DNA which are derived from pre-invasive lesion, benign or indolent tumor, which may not manifest or affect an individual within his/her life span. Detecting these lesions can result in unnecessary anxiety or series of investigations for an individual. Therefore, as a screening test, it will require stringent evaluation.
Recent guidelines for the role of testing cfDNA in lung cancer patients
The College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology published a guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors (TKIs) (30). It recommends that physicians may use plasma cfDNA methods to identify EGFR mutations in lung adenocarcinoma patients when insufficient tissue is obtained. It also supports the use of plasma for EGFR T790M mutation test in lung adenocarcinoma patients with progression or secondary clinical resistance to EGFR-targeted TKIs. When the testing of EGFR mutation in plasma is negative, testing the tumor sample is recommended. However, there is currently insufficient evidence to support the use of liquid biopsy for the diagnosis of primary lung adenocarcinoma by the identification of EGFR or other mutations.
Thus, the practical usefulness of EGFR mutation detection in liquid biopsy is “rule in” targetable mutations when tissue sample is limited or hard to obtain. When tissue biopsy materials are insufficient for molecular testing, cfDNA-based tests for patient selection for targeting therapy are possible (20,21,30). Furthermore, when biopsy tissue is inadequate or not available, detection of resistance mutation T790M in liquid biopsy may allow the consideration of using third generation TKI (22).
Liquid biopsy is not limited to cfDNA
miRNA
Detecting other circulating tumor-derived nuclear acid is also under investigations. For example, elevated levels of several microRNAs have been described in different cancers (27,28). However, the clinical unity of these approaches remains to be further evaluated.
Extracellular vesicles
Although it was discussed at length that cfDNA is a promising tumor marker for liquid biopsy, more candidates are emerging, such as extracellular vesicles (EV) which are secreted by tumor cells into the bloodstream (44-46). These membrane bound substances can be technically challenging to detect, but recent research has indicated that their detection may be simplified by using antibody-based assays, such as CD147 and CD9 for colorectal cancer (29).
Circulating tumor cells (CTCs)
It has long been discovered that intact tumor cells were shed into the blood-stream by the main tumor bulk (47). These cells can be isolated by means of density gradient centrifugation, size centrifugation, fluorescence-assisted cell sorting, or antibody-conjugated microfluidic devices, etc. (48). The detection of the amount of CTCs has been shown to have prognostic value in patients with metastatic breast cancer (7). Based on the clinical finding, Cellsearch CTC test (Menarini Silicon Biosystems, San Diego, CA, USA) has been approved by FDA for monitoring metastatic breast cancer (8). However, the techniques of isolating CTCs are still cumbersome and not easily adapted in most laboratories. Thus, its clinical utility will require further investigations and verification.
Limitations and challenges in liquid biopsy
While promising, limitations in liquid biopsy do exist. Apart from the sensitivity issues, there are other technical challenges. For example, gene translocations are particularly difficult to detect. The fragment length of cfDNA in blood can be quite short to span translocation breakpoints and make detecting gene translocations difficult (49,50). Detecting gene copy number variation in cfDNA is limited to high copy number amplification (51). For NSCLC patients with EGFR mutation who developed acquired resistance to the first or second generation TKIs, T790M mutation accounts for only about half of the resistance mechanisms. Other resistance mechanism, like small cell transformation (52) may not be readily detectable from liquid biopsy.
Emerging immunotherapeutic options such as immune checkpoint blockade may require tissue assessment of PD-L1 expression for patient selection (53). This could be beyond the capability of liquid biopsy at the present moment. Further investigations in the assessment of PD-L1 RNA expression, protein expression in CTC or estimation of tumor mutation burden in liquid biopsy may shed light on predicting the response of cancer patients to immunotherapies.
Conclusions
Knowledge on tumor biology and treatment advance constantly shape our diagnostic approach in cancer patients. There is increasing demand for detecting various biomarkers in tumor samples. Coupled with the technological breakthrough, it is now feasible to detect circulating tumor-derived cfDNA, tumor-derived compounds or cancer cells in peripheral blood. It opens the possibility of non-invasive, safe and easily repeatable testing platform in detecting cancer. It may serve as an attractive alternative approach in aiding diagnosis, disease monitoring, recurrence and detection of resistance mechanism in guiding clinical management. However, there are still limitations and challenges ahead. Further investigation, technological advancement, and clinical validation are mandatory to explore the clinical utility of liquid biopsy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Leon SA, Shapiro B, Sklaroff D, et al. Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res 1977;37:646-50. [PubMed]
- Shapiro B, Chakrabarty M, Cohn EM, et al. Determination of circulating DNA levels in patients with benign or malignant gastrointestinal disease. Cancer 1983;51:2116-20. [Crossref] [PubMed]
- Bedard PL, Hansen AR, Ratain MJ, et al. Tumour heterogeneity in the clinic. Nature 2013;501:355-64. [Crossref] [PubMed]
- Ye P, Zhang M, Fan S, et al. Intra-tumoral heterogeneity of HER2, FGFR2, cMET and ATM in gastric cancer: optimizing personalized healthcare through innovative pathological and statistical analysis. PloS one 2015;10:e0143207. [Crossref] [PubMed]
- Hoffman LM, DeWire M, Ryall S, et al. Spatial genomic heterogeneity in diffuse intrinsic pontine and midline high-grade glioma: implications for diagnostic biopsy and targeted therapeutics. Acta Neuropathol Commun 2016;4:1. [Crossref] [PubMed]
- Hiley CT, Le Quesne J, Santis G, et al. Challenges in molecular testing in non-small-cell lung cancer patients with advanced disease. Lancet 2016;388:1002-11. [Crossref] [PubMed]
- Cristofanilli M, Budd GT, Ellis MJ, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 2004;351:781-91. [Crossref] [PubMed]
- Hayes DF, Cristofanilli M, Budd GT, et al. Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin Cancer Res 2006;12:4218-24. [Crossref] [PubMed]
- Lee TL, Leung WK, Chan MW, et al. Detection of gene promoter hypermethylation in the tumor and serum of patients with gastric carcinoma. Clin Cancer Res 2002;8:1761-6. [PubMed]
- Leung WK, To KF, Man EP, et al. Quantitative detection of promoter hypermethylation in multiple genes in the serum of patients with colorectal cancer. Am J Gastroenterol 2005;100:2274-9. [Crossref] [PubMed]
- Chan KCA, Woo JKS, King A, et al. Analysis of Plasma Epstein-Barr Virus DNA to Screen for Nasopharyngeal Cancer. N Engl J Med 2017;377:513-22. [Crossref] [PubMed]
- Ngan RK, Yip TT, Cheng WW, et al. Circulating Epstein-Barr virus DNA in serum of patients with lymphoepithelioma-like carcinoma of the lung: a potential surrogate marker for monitoring disease. Clin Cancer Res 2002;8:986-94. [PubMed]
- Xie M, Wu X, Wang F, et al. Clinical significance of plasma Epstein-Barr Virus DNA in pulmonary lymphoepithelioma-like carcinoma (LELC) patients. J Thorac Oncol. 2018;13:218-27. [Crossref] [PubMed]
- Higgins MJ, Jelovac D, Barnathan E, et al. Detection of tumor PIK3CA status in metastatic breast cancer using peripheral blood. Clin Cancer Res 2012;18:3462-9. [Crossref] [PubMed]
- Mok T, Wu YL, Lee JS, et al. Detection of EGFR-activating mutations from plasma DNA as a potent predictor of survival outcomes in FASTACT 2: A randomized phase III study on intercalated combination of erlotinib (E) and chemotherapy (C). J Clin Oncol 2013:31:abstr 8021.
- Weber B, Meldgaard P, Hager H, et al. Detection of EGFR mutations in plasma and biopsies from non-small cell lung cancer patients by allele-specific PCR assays. BMC Cancer 2014;14:294. [Crossref] [PubMed]
- Sacher AG, Paweletz C, Dahlberg SE, et al. Prospective validation of rapid plasma genotyping for the detection of EGFR and KRAS mutations in advanced lung cancer. JAMA Oncol 2016;2:1014-22. [Crossref] [PubMed]
- Sanmamed MF, Fernández-Landázuri S, Rodríguez C, et al. Quantitative cell-free circulating BRAFV600E mutation analysis by use of droplet digital PCR in the follow-up of patients with melanoma being treated with BRAF inhibitors. Clin Chem 2015;61:297-304. [Crossref] [PubMed]
- Schwaederle M, Husain H, Fanta PT, et al. Use of liquid biopsies in clinical oncology: pilot experience in 168 patients. Clin Cancer Res 2016;22:5497-505. [Crossref] [PubMed]
- Mok T, Wu YL, Lee JS, et al. Detection and dynamic changes of EGFR mutations from circulating tumor DNA as a predictor of survival outcomes in NSCLC patients treated with first-line intercalated erlotinib and chemotherapy. Clin Cancer Res 2015;21:3196-203. [Crossref] [PubMed]
- Douillard JY, Ostoros G, Cobo M, et al. Gefitinib treatment in EGFR mutated caucasian NSCLC: circulating-free tumor DNA as a surrogate for determination of EGFR status. J Thorac Oncol 2014;9:1345-53. [Crossref] [PubMed]
- Oxnard GR, Thress KS, Alden RS, et al. Association between plasma genotyping and outcomes of treatment with osimertinib (AZD9291) in advanced non–small-cell lung cancer. J Clin Oncol 2016;34:3375-82. [Crossref] [PubMed]
- Spindler KL, Pallisgaard N, Vogelius I, et al. Quantitative cell free DNA, KRAS and BRAF mutations in plasma from patients with metastatic colorectal cancer during treatment with cetuximab and irinotecan. Clin Cancer Res 2012;18:1177-85. [Crossref] [PubMed]
- Diehl F, Schmidt K, Choti MA, et al. Circulating mutant DNA to assess tumor dynamics. Nat Med 2008;14:985-90. [Crossref] [PubMed]
- Garcia-Murillas I, Schiavon G, Weigelt B, et al. Mutation tracking in circulating tumor DNA predicts relapse in early breast cancer. Sci Transl Med 2015;7:302ra133. [Crossref] [PubMed]
- Dawson SJ, Tsui DW, Murtaza M, et al. Analysis of circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med 2013;368:1199-209. [Crossref] [PubMed]
- Madhavan B, Yue S, Galli U, et al. Combined evaluation of a panel of protein and miRNA serum-exosome biomarkers for pancreatic cancer diagnosis increases sensitivity and specificity. Int J Cancer 2015;136:2616-27. [Crossref] [PubMed]
- Zhu C, Ren C, Han J, et al. A five-microRNA panel in plasma was identified as potential biomarker for early detection of gastric cancer. Br J Cancer 2014;110:2291-9. [Crossref] [PubMed]
- Yoshioka Y, Kosaka N, Konishi Y, et al. Ultra-sensitive liquid biopsy of circulating extracellular vesicles using ExoScreen. Nat Commun 2014;5:3591. [Crossref] [PubMed]
- Lindeman NI, Cagle PT, Aisner DL, et al. Updated molecular testing guideline for the selection of lung cancer patients for treatment with targeted tyrosine kinase inhibitors: Guideline from the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J Thorac Oncol 2018;13:323-58. [Crossref] [PubMed]
- Jahr S, Hentze H, Englisch S, et al. DNA fragments in the blood plasma of cancer patients: quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer res 2001;61:1659-65. [PubMed]
- Krishnamurthy N, Spencer E, Torkamani A, et al. Liquid biopsies for cancer: coming to a patient near you. J Clin Med 2017;6. [Crossref] [PubMed]
- Yeung SF, Tong JHM, Law PPW, et al. Profiling of Oncogenic Driver Events in Lung Adenocarcinoma Revealed MET Mutation as Independent Prognostic Factor. J Thorac Oncol 2015;10:1292-300. [Crossref] [PubMed]
- Blumenthal GM, Pazdur R. Approvals in 2017: gene therapies and site-agnostic indications. Nat Rev Clin Oncol 2018;15:127-8. [Crossref] [PubMed]
- Yu T, Morrison C, Gold E, et al. Retrospective Analysis of NSCLC Testing in Low Tumor Content Samples: Single-Gene Tests, NGS, & the Oncomine™ Dx Target Test. J Thorac Oncol 2017;12:S1845. [Crossref]
- Santini FC. RET rearrangements in non–small cell lung cancer and implications for the future of precision drug development. Expert Rev Precis Med Drug Dev 2018;3:63-7. [Crossref]
- Crowley E, Di Nicolantonio F, Loupakis F, et al. A. Liquid biopsy: monitoring cancer-genetics in the blood. Nat Rev Clin Oncol 2013;10:472-84. [Crossref] [PubMed]
- Frattini M, Gallino G, Signoroni S, et al. Quantitative and qualitative characterization of plasma DNA identifies primary and recurrent colorectal cancer. Cancer lett 2008;263:170-81. [Crossref] [PubMed]
- Margonis GA, Kim Y, Spolverato G, et al. Association between specific mutations in KRAS codon 12 and colorectal liver metastasis. JAMA surg 2015;150:722-9. [Crossref] [PubMed]
- Spindler KL, Pallisgaard N, Andersen RF, et al. Circulating free DNA as biomarker and source for mutation detection in metastatic colorectal cancer. PloS one 2015;10:e0108247. [Crossref] [PubMed]
- IASLC Atlas of EGFR Testing in Lung Cancer. Available online: https://www.iaslc.org/publications/iaslc-atlas-egfr-testing-lung-cancer
- Planchard D, Besse B, Groen HJ, et al. Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol 2016;17:984-93. [Crossref] [PubMed]
- Cohen JD, Li L, Wang Y, et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 2018;359:926-30. [Crossref] [PubMed]
- Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol 2013;200:373-83. [Crossref] [PubMed]
- György B, Szabó TG, Pásztói M, et al. Membrane vesicles, current state-of-the-art: emerging role of extracellular vesicles. Cell Mol Life Sci 2011;68:2667-88. [Crossref] [PubMed]
- EL Andaloussi S, Mäger I, Breakefield XO, et al. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov 2013;12:347-57. [Crossref] [PubMed]
- Ashworth T. A case of cancer in which cells similar to those in the tumours were seen in the blood after death. Aust Med J 1869;14:146.
- Alix-Panabières C, Pantel K. Circulating tumor cells: liquid biopsy of cancer. Clin Chem 2013;59:110-8. [Crossref] [PubMed]
- Underhill HR, Kitzman JO, Hellwig S, et al. Fragment length of circulating tumor DNA. PLoS Genet 2016;12:e1006162. [Crossref] [PubMed]
- Bettegowda C, Sausen M, Leary RJ, et al. Detection of circulating tumor DNA in early-and late-stage human malignancies. Sci Transl Med 2014;6:224ra24. [Crossref] [PubMed]
- Chan KC, Jiang P, Chan CW, et al. Noninvasive detection of cancer-associated genome-wide hypomethylation and copy number aberrations by plasma DNA bisulfite sequencing. Proc Natl Acad Sci U S A 2013;110:18761-8. [Crossref] [PubMed]
- Oser MG, Niederst MJ, Sequist LV, et al. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol 2015;16:e165-e172. [Crossref] [PubMed]
- Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. [Crossref] [PubMed]


