Bronchoscopic management of prolonged air leak
Introduction
Broncho-pleural fistula (BPF) is an atypical communication between the tracheobronchial tree and the alveolar/pleural space, with prolonged air leak (PAL). BPF is frequent and related to significant morbidity, prolonged length of hospital stay, and mortality (1). Patients with underlying respiratory comorbidities or in poor general condition are at a notably increased risk for a PAL (2). Lobectomies or pneumonectomies, though, are not the only origin of this challenging complication. Simple procedures or even lung diseases without any interventions could develop a BPF. It is well-known that BPF could increase morbidity and mortality. High morbidity could be due to a prolonged length of hospital stay, atelectasis, community-acquired pneumonia, and thromboembolic event. Nevertheless, in about 10%, more than five days of an air leak is considered a PAL (1).
In 1897, Gustav Killian performed the first rigid bronchoscopy. Subsequently, bronchoscopy has experienced a diagnostic and therapeutic development. The innovative developments augmented in 1966 with the introduction by Shigeto Ikeda of flexible bronchoscopy (3). Several endoscopic techniques have beforehand been reported for the treatment of PAL, including lead shots, installation of ethanol, fibrin glue, antibiotics, or albumin-glutaraldehyde tissue adhesive. Unfortunately, the installation of these substances is frequently associated with irreversible obstruction of selected airways, marked foreign body reaction, or both (2). One of the new development in therapeutic bronchoscopy is the placement of endobronchial valves (3). We review the management of PAL developed after a pulmonary resection managed with the endobronchial approaches.
Definition of PAL
The discovery of bubbles in the water seal chamber indicates the presence of an air leak. This is common during the first two days after surgery but could persist in few patients. The severity of air leak is characteristically classified according to the respiratory cycle phase where the bubbles appear. Air leak increases along the following range: air escape during forced exhalation manoeuvre (a cough), quiet exhalation (spontaneous breathing), inspiration (positive pressure breathing), and both (inhalation and exhalation). Digital flow meters in drainage systems could quantify the leak and are widely available. An air leak is prolonged if it persists after 5 days (3,4).
Quantification of air leaks
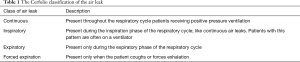
The volume of air bubbling through a water seal chamber is not easy to quantify. Any chest drainage system go back in the nineteenth century to Gotthard Bülau who first used drainage with a tube draining fluid and air underwater to preserve the negative pressure of the pleural cavity. Assumed the trouble of quantitative measurement, qualitative assessment of air leaks could be tried by discriminating active leaks (bronchiolo-alveolar districts) from passive leaks (reduced lung compliance). The strategy of suction applied to chest drainages varies among institutions and surgeons. Electronic chest drainage systems offer a possible exit strategy for this impasse. They achieve a quantitative calculation of air leaks not only at a given moment but over a defined period (3,4). There are multiple ways to evaluate the volume of air leaks and most are simple and based on observing the water seal chamber. Most common in clinical use is a simple description, such as mild, moderate, or severe. This method lacks standardisation and validation among observers (5). The digital and continuous air leak measurement provides consistent evidence for assessment of the surgeons and forthright clinical decisions leading to reduce the hospital length of stay. Diverse systems are accessible nowadays, which nonstop calculation of the air leaks or the air loss (6). An alternative method is the Cerfolio classification system that is also based on observation, but is less subjective, is validated, and is reproducible among observers. In this classification, there are four categories based on the timing of the air leak in the respiratory cycle (Table 1), coupled with the grading or sizing of the air leak as measured by an air leak meter (7).
Full table
Bronchoscopic management of PAL
Amplatzer devices
Amplatzer devices are well-known for the heart septal defect closure. Made of Nitinol mesh with a polyester cloth, this combination offers early coverage and formerly encourages the growth of the tissue over the device. Two devices have been employed in BPF management with a thin central diaphragm or with a disc on each termination. The fitting dimension is contingent on the size of the stump and length of the BPF to treat. For placement, a guidewire is passed through the flexible bronchoscope channel, and the BPF followed by a sheath. Subsequent, the Amplatzer devices and its distal disc are forward through the BPF and positioned by pulling back. The second disc is formerly carried to the proximal side of the BPF (4).
Watanabe spigots
Watanabe reported silicone-made bronchial fillers to treat intractable pneumothorax and BPF. It was described that the air leak in the majority of patients was reduced or stopped with these implants. Nevertheless, only 57% of these patients were liberated from their chest tubes. Also, no systematic long-term follow-up studies have been described (2).
Endobronchial valves
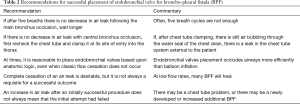
The placement of the endobronchial valves can be achieved merely with a flexible bronchoscope, under conscious sedation and local anaesthesia. The choice is a function of several factors as the available resources and the experience (Table 2). The endobronchial valves in the management of PAL have potential hazards, such as the migration of the valve inside the bronchial tree (3). Treatment of PAL with one-way endobronchial valves is feasible, safe, and resulted in successful treatment and reduction of air leakage flow in the majority of patients. The air is not entering the pleural space, thus enabling the lung to possibly re-expand and heal spontaneously. In contrast to other blocking devices, however, valves allow for expiration and clearance of bronchial secretions, therefore reducing the risk of post-obstructive pneumonia. In the United States, the use of one-way valves is restricted to air leakage after lung resection. On the contrary, valves have received European Conformity certification and can be used for the treatment of air leak without specific restrictions in 2006 (2). A typical approach to endobronchial valves in the BPF management has been defined: endobronchial valves placement should be indicated in BPF after five days in spite of proper management. The lung/lobe/segment through where the leak occurs should be localised with bronchoscopy and balloon occlusion. An endobronchial balloon is inflated in the ipsilateral main bronchus while a decrease in the rate of air leak through the water chamber of a water seal chest drain should be observed, for five breathing cycles. The sequence is then repeated advancing the balloon distally, isolating lobar first and segmental airways subsequently. The balloon occlusion could guide other endobronchial valves placements until the stop of PAL through the BPF (8). Potential endobronchial valves advantages include potentially decreased hospitalisation and pleural drainage days. However, non-pulmonary resection air leaks constitute a somewhat diverse population, and it remains unclear who benefits the most from interventions like endobronchial valves (9,10). The cost of endobronchial valves can be justified in selected patients, especially if used earlier when one can avoid the costs of a more extended hospital stay. Direct cost comparisons with other treatments are needed to understand the cost-effectiveness in comparison to other alternatives better. Further studies are ongoing to understand the role of endobronchial valves therapy and how to appropriately select the correct patient population to treat (11). Randomized controlled trials are ongoing to find out the perfect patients and timing of the valve placement, understanding their effect on patient quality of life and satisfaction, as well as their cost-effectiveness (12).
Full table
Conclusions
PAL is a challenging complication and is accounted for noteworthy morbidity. Endobronchial valves placement is comparatively non-invasive when the surgery is the only alternative. Given the cost of a protracted length of hospital stays and the morbidity of unsettled BPF, the placement of endobronchial valves may be cost-effective. Endobronchial valve is a novel device for the PAL management with minimal morbidity if related to surgical repairs. While it is suggested that surgical treatment should be undertaken when possible, endobronchial valves should be recommended as a therapeutic choice in high-risk patients. Placement techniques remain operator and patient friendly and allow the procedure to be performed with relative ease. By the current data, prospectively conducted, randomised, controlled clinical trials are needed where valve treatment is compared with other bronchoscopic techniques, surgical procedures, or both.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Akgül AG, Özbay S, Mehmetoğlu SS, et al. Simple and economical management of a prolonged air leak. J Bronchology Interv Pulmonol 2013;20:355-6. [Crossref] [PubMed]
- Firlinger I, Stubenberger E, Müller MR, et al. Endoscopic one-way valve implantation in patients with prolonged air leak and the use of digital air leak monitoring. Ann Thorac Surg 2013;95:1243-9. [Crossref] [PubMed]
- El-Sameed Y, Waness A, Al Shamsi I, et al. Endobronchial valves in the management of broncho-pleural and alveolo-pleural fistulae. Lung 2012;190:347-51. [Crossref] [PubMed]
- Keshishyan S, Revelo AE, Epelbaum O. Bronchoscopic management of prolonged air leak. J Thorac Dis 2017;9:S1034-46. [Crossref] [PubMed]
- Wood DE, Cerfolio RJ, Gonzalez X, et al. Bronchoscopic management of prolonged air leak. Clin Chest Med 2010;31:127-33. Table of Contents. [Crossref] [PubMed]
- Mueller MR, Marzluf BA. The anticipation and management of air leaks and residual spaces post lung resection. J Thorac Dis 2014;6:271-84. [PubMed]
- Cerfolio RJ, Bass CS, Pask AH, et al. Predictors and treatment of persistent air leaks. Ann Thorac Surg 2002;73:1727-30; discussion 1730-1.
- Gaspard D, Bartter T, Boujaoude Z, et al. Endobronchial valves for bronchopleural fistula: pitfalls and principles. Ther Adv Respir Dis 2017;11:3-8. [Crossref] [PubMed]
- Gilbert CR, Casal RF, Lee HJ, et al. Use of one-way intrabronchial valves in air leak management after tube thoracostomy drainage. Ann Thorac Surg 2016;101:1891-6. [Crossref] [PubMed]
- Mahajan AK, Khandhar SJ. Bronchoscopic valves for prolonged air leak: current status and technique. J Thorac Dis 2017;9:S110-5. [Crossref] [PubMed]
- Podgaetz E, Zamora F, Gibson H, et al. Intrabronchial Valve Treatment for Prolonged Air Leak: Can We Justify the Cost? Can Respir J 2016;2016. [Crossref] [PubMed]
- Podgaetz E, Andrade RS, Zamora F, et al. Endobronchial treatment of bronchopleural fistulas by using intrabronchial valve system: a case series. Semin Thorac Cardiovasc Surg 2015;27:218-22. [Crossref] [PubMed]


