History of lung volume reduction procedures
Introduction
The abnormal expansion of the lungs has been recognized as a main finding in emphysema since the report of autoptic observations by Laennec in his famous treatise on chest diseases at the beginning of XIX century (1). He described the increased volume and the failure of the emphysematous lungs to collapse at the opening of pleural cavities.
In the XX century advances in respiratory physiology better identified mechanical properties of healthy and pathological respiratory system. The increase in functional residual capacity (FRC) due to loss of elastic recoil of lung parenchyma has been termed static pulmonary hyperinflation; it poses the diaphragm in a state of mechanical disadvantage. Dynamic hyperinflation refers to the rise in end-expiratory lung volume at rest or during exercise as a consequence of air flow limitation that prevents the respiratory system from attaining static equilibrium before the next inspiratory effort. The resulting intrinsic alveolar positive end-expiratory pressure (PEEP) imposes an elastic inspiratory threshold on respiratory muscles that greatly increases the work of breathing. These physiological derangements are closely related to dyspnea and quality of life (QOL) in patients with emphysema (2).
Inhaled bronchodilators, currently the drugs of choice in chronic obstructive pulmonary disease (COPD), can attenuate dynamic hyperinflation improving dyspnea and exercise tolerance (3). However, many emphysematous patients do not obtain a consistent clinical benefit with pharmacological therapy and/or pulmonary rehabilitation.
Aim of this review is to report the historical evidence regarding the development and dissemination of both surgical and endoscopic lung volume reduction (LVR) procedures.
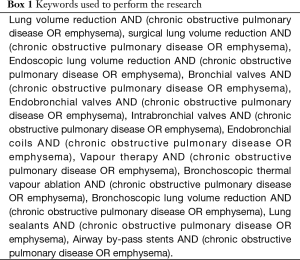
A search of relevant medical literature was conducted in Medline/PubMed including observational and interventional studies from 1961 through January 2018. Keywords used to perform the research are reported in Box 1. Studies targeting children and editorials, narrative, and conference abstracts have been excluded.
Full table
Surgical LVR
In the 1950s the American surgeon and anatomist Otto Brantigan [1904–1981] first introduced a surgical approach in patients with emphysema. He speculated that the mechanical properties of the respiratory system could be improved by removing the most functionally useless portions of lung parenchyma. In 1961, he published a case series on 56 patients who underwent unilateral (n=42) or bilateral (n=14) operations (4). LVR was obtained by resection and/or folding of most hyperinflated lung tissue. The physiological benefit of intervention was not clearly established; however, he reported clinical improvement in 75% of treated patients and a consistent increase in vital capacity (VC). Brantigan’s conjecture was not welcomed in medical community and raised criticism because of high operative mortality (about 16%) and the apparent paradox of removal of lung tissue in a destructive disease as emphysema. Given these considerations, LVR surgery was put aside until the reappraisal by J. Cooper in the early 1990s. Cooper had gained experience in lung transplantation and noticed an impressive and fast reduction of chest volume in patients transplanted for end-stage emphysema. He speculated that in patients with emphysema, especially centrilobular and upper-lobe predominant, removal of functionless hyper-inflated zones could downsize the chest and ameliorate ventilatory mechanics and gas exchanges.
In 1997 Cooper reported the results of a series of 100 consecutive cases, mean age 61 years and mean forced expiratory volume in 1st second (FEV1) 0.69 L (24% of predicted), who experienced at 6-month follow-up a mean increase of 400 mL in FEV1 and 600 mL in forced VC (FVC) and a reduction in residual volume (RV) of about 2 L (5). Exercise tolerance improved and many patients did not further require oxygen therapy (33% of cases required oxygen supplementation 6 months after surgical intervention vs. 90% before surgical intervention). The surgical procedure was done through a median sternotomy and bilateral volume reduction. In the vast majority of cases the upper lobes were the target of tissue removal. Post-operative stay was on average 14 days and the 1-year all-causes mortality was 5% (5).
In the same decade the initial reports by Cooper stimulated other thoracic surgeons to perform LVR surgery in thousands of patients as a palliative treatment for advanced emphysema and several uncontrolled case series reported functional improvement after bilateral LVR surgery. In the following years small randomized controlled trials (RCTs) shed light on the possible role of LVR surgery in the clinical management of emphysematous patients (6).
In 1999, Criner et al. published the results of a prospective RCT comparing pulmonary rehabilitation followed by bilateral LVR surgery to pulmonary rehabilitation alone in advanced emphysema (6). The authors screened 200 patients and LVR surgery was performed in 32 cases, with an overall mortality rate of 9.4% (3 out of 32). High Resolution Computerized Tomography (HRCT) and perfusion lung scan were used to target the more compromised lung tissue; 20% to 40% of lung volume was removed on each side via median sternotomy and stapling resection. At 3-month post-operative evaluation, surgical patients showed significant improvement in FEV1, FVC, total lung capacity (TLC), RV, gas exchange and QOL compared with post-rehabilitation values in patients randomized to the rehabilitation alone group (6).
Geddes et al. in 2000 evaluated 174 patients, after optimization of medical therapy and a rehabilitation program, 24 were randomized to continue standard medical therapy and 24 to bilateral LVR surgery via median sternotomy or thoracoscopy (7). Similarly to the study by Criner, the portions of lung tissue to be removed were identified on HRCT and visually during intervention. After 6 months the authors reported a significant improvement in FEV1, shuttle walk distance and QOL favoring surgical patients, while the impact on mortality was uncertain (7).
Goldstein et al. in 2003 studied the effect of LVR surgery focusing on disease-specific QOL (8). Of 328 screened subjects with severe heterogeneous emphysema, 55 were randomized after pulmonary rehabilitation (28 in the surgery group vs. 27 in the control group). Preoperative evaluation included HRCT and ventilation-perfusion (V/Q) lung scan; the surgical procedure, differently from the studies by Geddes and Criner, was done in most cases by video-assisted thoracic surgery (VATS) removing 20% to 30% of lung volume. Surgical patients had a significant benefit in disease-specific QOL that was sustained at 12 months (8). Similarly to Goldstein et al., a Swedish trial started in 1996 by Hillerdal et al. had, as primary end point, patients’ health status (9). After an initial 6-week physical training program, the authors randomized 106 patients with diffuse but heterogeneous emphysema to either LVR surgery with continued training for 3 months (53 cases) or to continued training alone for 1 year (53 cases). Bilateral LVR surgery by median sternotomy was the preferred procedure. The results published in 2005 showed a significant improvement in health status in the LVR group, however the surgical procedure was associated with a higher mortality risk (7 vs. 2 deaths) (9).
In spite of some initially promising results, many questions remained unanswered. To evaluate the effects on mortality, the magnitude and durability of benefits, and criteria for the selection of patients, a large RCT, the National Emphysema Treatment Trial (NETT), was designed and published in 2003 (10). Overall mortality and maximal exercise capacity were the primary endpoints. The study enrolled 1,218 patients and, after 24 months, exercise capacity had improved by more than 10 W in 15% of patients in the surgery group, as compared with 3% of patients in the medical-therapy group (P<0.001). A survival advantage was seen only in patients with upper-lobe predominant emphysema and low exercise capacity (40 W in men, 25 W in women). As main conclusion the authors observed that patients with non-upper-lobe emphysema and high base-line exercise capacity were poor candidates for LVR surgery, because of increased mortality and negligible functional gain. The overall 90-day mortality was 7.9% in the surgical group vs. 1.3% in the medical care group (P<0.001). A high risk for postoperative death (28.6%) had been observed at an interim analysis in 70 patients with FEV1 <20% predicted and either homogeneous emphysema or DLCO <20% predicted (10).
Following the NETT trial, in order to reduce morbidity and mortality associated with LVR surgery, some centers adopted VATS and unilateral procedure; other groups proposed a non-resectional folding of less functional lung tissue to reduce the risk of prolonged air leaks (11).
In 2016, the authors of a Cochrane review concluded that LVR surgery may lead to better health status and lung function outcomes in patients with severe upper lobe-predominant emphysema and low exercise capacity, however the authors recognized that the procedure is not without risks, being associated with risks of early mortality and adverse events (12).
At present several centers worldwide offer LVR surgery. However, many patients are ineligible for medical reasons or decline surgical interventions because of its invasiveness and the risk of operative death.
Endoscopic LVR
The history of LVR surgery has taught us that selected emphysematous patients can benefit from a remodeling intervention that aims at restoration of chest geometry. To overcome the operative risks linked to LVR surgery, several endobronchial procedures have been invented to obtain similar results with a more convenient risk/benefit ratio.
Bronchial valves (BV)
One-way BV have been designed for placement by a flexible bronchoscope in the segmental or sub-segmental bronchi of a pulmonary lobe to obtain a lobar atelectasis. Two valve models have been marketed in 2000’s (Zephyr® EBV, Emphasys Medical, now Pulmonx; IBV®, Spiration, now Olympus).
Valve therapy is a reversible blocking procedure, hence lobar exclusion is not always attainable because of collateral ventilation through incomplete fissures or due to anatomical/technical issues.
Several uncontrolled case series reported encouraging outcomes.
Endobronchial valves (EBV)
Different RCTs on the use of EBV have been designed and conducted in the last decade (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf). The first RCT published in 2010 was the multicenter VENT study, carried out in the USA to evaluate the efficacy and safety of endoscopic treatment with Zephyr® valves compared to medical care in 321 patients with advanced heterogeneous emphysema (220 EBV vs. 101 control) (13). Co-primary efficacy endpoints were percentage change in FEV1 and 6-minute walking test (6MWT) at 6 months. Secondary efficacy end points were: changes in QOL as measured on the St. George’s Respiratory Questionnaire (SGRQ), incremental cycle exercise capacity, dyspnea as measured on the modified Medical Research Council (mMRC) scale, and daily oxygen use.
Endobronchial LVR procedures led to a significant improvement in FEV1, 6MWT and QOL although the magnitude of results was modest (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf). A clinically meaningful change in functional primary endpoints and symptoms was linked to inter-lobar heterogeneity of emphysema and complete fissure as evaluated by HRCT. Hemoptysis and COPD exacerbations were more frequently observed in the EBV group during the follow-up after valve implantation (13). The VENT study had a smaller European subgroup of patients, whose results were reported separately in 2012 (14). When comparing the 111 participants assigned to the EBV group to the 70 controls, the European cohort showed similar results to the twin study performed in the US, with the exception of a border line result in FEV1 (P=0.067). Good safety results were confirmed since serious complications did not differ between groups. Completeness of fissure and lobar exclusion were confirmed as predictors of higher changes while heterogeneity of emphysema was not a critical factor (14).
The VENT study was followed by two smaller European single-centre RCTs: the BeLieVeR-HIFi performed in the UK and the STELVIO study performed in the Netherlands, both published in 2015 (15,16) (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf). Both studies included patients with a target lobe with intact inter-lobar fissures on chest CT, and the BeLieVeR-HIFi also required the presence of heterogeneous emphysema. Collateral ventilation was assessed in all patients with Chartis® system (Pulmonx). In the BeLieVeR-HIFi patients were randomized to placement of Zephyr® EBV valves plus medical therapy vs. sham bronchoscopy plus medical therapy, while in the STELVIO study the control group was not subjected to sham bronchoscopy. Both studies reported similar outcomes in regards to pulmonary function tests and exercise capacity when compared to the VENT study (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf). Serious adverse events occurred more frequently in the EBV group, in particular, two deaths (8% of patients in the EBV group) occurred in the BeLieVeR-HIFi and one (3% of patients in the EBV group) in the STELVIO study, both in patients treated with bronchoscopic lung volume reduction (BLVR) (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf).
BeLieVeR-HIFi and STELVIO set the stage for completed or ongoing multicenter RCTs.
The IMPACT study, published in 2016, tested Zephyr® EBV in patients with homogeneous emphysema without collateral ventilation as assessed by Chartis® system (17). The study showed positive results in pulmonary function tests, 6MWT and QOL (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf). However, 11 cases of procedure-related pneumothoraces were reported.
Another recent multicenter RCT, the TRANSFORM trial, evaluated the efficacy and safety of Zephyr® EBV in 97 patients (65 cases in the EBV group vs. 32 in the standard of care group) with heterogeneous emphysema and absence of collateral ventilation (18). EBV treatment resulted in clinically and statistically significant benefits in lung function, dyspnea, exercise tolerance, and quality of life, with an acceptable safety profile, in accordance with the results of the previously cited studies (online: http://jtd.amegroups.com/public/system/jtd/supp-jtd.2018.04.165-1.pdf).
Other trials have completed recruitment or are currently ongoing. A recent Cochrane review concluded that EBV was associated with FEV1 and SGQR improvement compared to standard of care; however, patients’ selection was recognized to play a fundamental role, since absence of collateral ventilation was associated with superior clinically significant improvements in health outcomes (19). In regards to adverse events, there were no significant differences in mortality between intervention and control groups, nevertheless other side effects, particularly pneumothoraces, were more common in the EBV group (19).
Intrabronchial valves (IBV)
A multicentre, blinded, sham-controlled study published in 2012 assessed the efficacy and safety of IBV using a bilateral upper lobe treatment approach without the goal of lobar atelectasis (20). Thirty-seven patients underwent bronchoscopy and IBV valve placement, while 36 were randomized to control group. Primary endpoint was a ≥4-point improvement in SGRQ and a lobar volume shift as measured by quantitative CT. At 3 months only a minority of treated subjects attained the endpoint (24%) vs none in the control group (P=0.002). Eberhard and colleagues compared complete lobar unilateral vs. partial bilateral treatment with IBV in 22 patients, 11 in each arm. End points were change in pulmonary function tests, 6MWD, mMRC dyspnea score and QOL as measured by SGRQ. Unilateral treatment was significantly superior in all measurements at 30 days (21). In the IBV study [2014], 277 subjects from 36 centers were enrolled in a randomized, sham-controlled, double-blind trial (22). Valves were placed bilaterally, partially occluding the bronchi of the target lobe. The primary endpoint was a significant improvement in disease-related QOL as assessed with SGRQ and changes in lobar lung volumes. Treated patients did not achieve clinically meaningful results.
Overall the available evidence shows that BV may have a role in the multimodality treatment of a subset of patients with advanced emphysema who are symptomatic on maximal pharmacological therapy and are engaged in rehabilitation programs. Lobar atelectasis is a precondition to achieve a clinically meaningful outcome. The advantage of BV is reversibility, since they can be easily removed or replaced.
Endobronchial coils
The coils are metallic devices made of memory-shape nitinol (a metal alloy of nickel and titanium in roughly equal percentage) measuring 100–150 mm in length. They are placed in a straightened form through the working channel of a flexible bronchoscope; when deployed they recover the coiled shape compressing lung parenchyma. Because of its mechanism of action, collateral ventilation is not a concern. Usually 8 to 10 coils are placed per lobe in 2 bilateral lobes in 2 steps 1 to 3 months apart, under visual and fluoroscopic control. Following small feasibility studies, three RCTs have been done to evaluate efficacy and safety of this modality of treatment.
The RESET trial [2013] evaluated coils in 47 patients from three UK centers (23 active treatment vs. 24 usual care) defining between-group difference in SGRQ at 3 months as the primary endpoint (23). Patients were included irrespectively of distribution of emphysema. The coil-treated group had a difference in change from baseline of –8.6 points on SGRQ compared with the control group (P=0.04); 57% of the coil-treated patients improved at least 8 points, compared with 13% of the patients in the control group (P=0.01). An increase in 6MWD ≥26 m was registered in 74% of patients in the LVR group compared to 17% in the usual care group (P<0.0003). Adverse events did not occur more frequently in coil-treated participants (23).
The REVOLENS study (RéductionVolumique Endobronchique par Spirales), published in 2016, investigated endobronchial coil therapy vs. usual care in 100 emphysematous patients from 10 French centers (24). The primary endpoint was between-group difference in the proportion of patients improving by at least 54 m on the 6MWD at 6 months after treatment. The primary endpoint was reached by 18 patients (36%) in the coil group and 9 patients (18%) in the usual care group (P=0.03). The difference on SGRQ was −13.4 points at 6 months and −10.6 points at 12 months (P<0.001 for both). Within 12 months, 4 deaths occurred in the coil group and 3 in the usual care group. Furthermore, given the high costs associated with LVR strategies for severe emphysema, the investigators conducted a cost-effectiveness analysis, reporting higher short term costs in the intervention group (mean 1-year per-patient cost in the intervention group was $53,821 vs. $5,912 in the control group, with a difference between groups of $47,908, P<0.001).
The RENEW trial [2016] evaluated the efficacy and safety of coils in 315 patients coming from 21 North American and 5 European centers (157 usual care vs. 158 coils treatment) (25). Each patient underwent 2 sequential procedures 4 months apart. The primary efficacy endpoint was the difference in absolute change from baseline in 6MWT at 12 months [minimal clinically important difference (MCID), 25 m]. Between-group difference in 6MWD was 14.6 m (P=0.02). Improvement of at least 25 m occurred in 40% of patients in the coil group vs 26.9% in the usual care group (P=0.01). A statistically significant change was observed in FEV1 and SGRQ, each favoring the coil group. The authors also performed a primary safety analysis including major complications, such as death, hemoptysis, pneumothorax requiring extended chest tube drainage, respiratory failure requiring mechanical ventilation, and lower respiratory tract infections. These major complications (potentially life-threatening or fatal events) occurred in 34.8% of coil participants vs. 19.1% of usual care (P=0.002). This statistically significant difference was mainly driven by increased incidence in lower respiratory tract infections in the coils group compared to control group (18.7% vs. 4.5%; P<0.001). Furthermore, there were 2 cases of hemoptysis requiring intervention in the coil group. However, no differences in other major complications, including death, complicated pneumothorax and severe respiratory failure, were observed between groups.
A Cochrane review analyzing the three cited studies and comprising 461 participants agreed upon the fact that treatment with endobronchial coils compared to usual care led to a significant improvement in mean difference in FEV1 and SGRQ, but not in exercise capacity, evaluated through 6MWT (19). Furthermore, in spite of not having significant differences in regards to mortality, adverse events were significantly more common in patients treated with coils, particularly lower respiratory tract infections, including COPD exacerbations and pneumonia, and pneumothoraces (19). The available evidence suggests that a subgroup of carefully selected emphysematous patients, such as those with more severe static hyperinflation, might benefit from this volume-reducing treatment.
Vapour therapy
Bronchoscopic thermal vapour ablation (BTVA) refers to delivery of thermal energy to diseased lung tissue using heated water vapour in order to achieve an inflammatory and scarring reaction.
In an uncontrolled study Snell et al. [2012] reported a significant improvement in FEV1, RV, SGRQ, 6MWD and mMRC at 6 months post-treatment in 44 patients from Europe and USA (26).
The multicenter RCT STEP-UP (Sequential Staged Treatment of Emphysema with Upper Lobe Predominance), published in 2016, evaluated selective sequential treatment of the more diseased upper lobe segments with BTVA in 70 patients with severe, upper lobe-predominant emphysema from 13 European and 3 Australian centers (27). Forty-six patients were allocated to treatment group and 24 to the control group. Between groups changes in FEV1 and SGRQ score at 6 months were the primary endpoints and both were reached in the treatment group (FEV1 +14.7%, P<0.0001; SGRQ –9.7 points, P=0.0021). These improvements in FEV1 and QOL were retained at 12-month follow-up (28). However, BTVA patients experienced more COPD exacerbations and a death possibly related to treatment (27).
At present the role of BTVA is unclear given the available evidence about efficacy, safety and durability of results. Potentially it offers the unique opportunity to treat sequentially only the targeted segments sparing the more preserved ones in case of marked intra-lobar heterogeneity.
Lung sealants
AeriSeal® is a polymeric foam developed to be delivered via a catheter introduced in the working channel of a flexible bronchoscope. It aims at reducing hyperinflation by irreversibly occluding small airways and collateral bronchial branches in the target pulmonary zone, producing absorptive atelectasis and scarring. Hence collateral ventilation would not invalidate the results of the procedure.
Following preliminary pilot studies, the AeriSeal System for Hyperinflation Reduction in Emphysema (ASPIRE) RCT was launched in 2012 to evaluate AeriSeal® treatment in patients with advanced upper-lobe emphysema (29). It was prematurely terminated for financing reasons after 95 of the 300 planned patients had been randomized. The planned primary efficacy end-point was mean percentage change in post-bronchodilator FEV1 from baseline to 12 months. Secondary efficacy end-points included proportion of patients achieving an increase in FEV1 ≥100 mL and 12%, changes in mMRC dyspnea score, disease-specific QOL assessed through SGRQ, and changes in 6MWD and upper lobe volume (measured by quantitative CT scan) at 12 months. The available results could be analyzed only at 3 and 6 months and favored the treatment group. On the other hand 44% of treated patients had major complications requiring hospitalization and 2 possibly procedure-related deaths occurred (29). For these reasons AeriSeal® is not currently marketed for clinical use.
Airway by-pass stents
Airway bypass aims at pulmonary deflation by creating transbronchial passages that are supported with paclitaxel-eluting stents.
The Exhale Airway Stents for Emphysema (EASE) trial was a multicenter randomized, double-blind, sham-controlled study that enrolled 315 emphysematous patients with severe hyperinflation (airway bypass group 208 cases vs. control group 107 cases) (30). Co-primary efficacy endpoints were: 12% or greater improvement in FVC and 1 point or greater decrease in the mMRC dyspnoea score at 6 months from baseline. These outcome measures were not accomplished.
Current evidence for BLVR
Up to now, as suggested by a Cochrane review published in 2017, the strongest evidence in regards to short-term improvements in disease status, including lung function and QOL, has been in support of EBV and endobronchial coils (19). Improvements in lung function and QOL were also found for vapour ablation and AeriSeal®, but the quality of that evidence is limited as the study on vapour ablation was small and the RCT on AeriSeal® was terminated early. Neither airway bypass stents nor partial bilateral placement of IBV seemed to lead to significant changes in health outcomes, although unilateral placement of IBV did lead to better health outcomes as assessed by a small study (20). Studies that found improvements in health outcomes also found higher rates of potential complications as a result of the procedures themselves. However, the available studies, although not conclusive, did not provide evidence for a higher risk of death after BLVR procedures (19).
Current clinical practice
Based on current body of evidence LVR may be considered for symptomatic emphysematous patients with significant hyperinflation, who have stopped smoking, take a state-of-art drug therapy, and are engaged in a rehabilitation program (31).
In 2017, an expert panel published recommendations for clinical use of EBV (31).
On the basis of current knowledge EBV should be addressed to clinically stable emphysematous patients with a RV >175% of predicted, FEV1 between 15% and 50% of predicted, no evidence of significant coexistent pulmonary disease on CT scan and a distance walked at 6MWD >100 m. The target lobe is identified on HRCT multiplanar reconstructions; in cases with homogeneous emphysema perfusion lung scan may be of value. The absence of collateral ventilation should be verified by Chartis system unless quantitative CT shows >95% completeness of interlobar fissure. PaCO2 >60 mmHg or PaO2 <45 mmHg are suggested as exclusion criteria. The absence of lobar atelectasis at 1 month should prompt a re-evaluation and removal or repositioning of the valves (31).
Coils-treatment may be offered to patients who are not candidate to BV due to collateral ventilation. The possible role and indications of BTVA and AeriSeal® should be further studied. Surgical treatment may still be considered for patients with a predominantly paraseptal emphysema (32).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- René-Théophile-Marie-Hyacinthe Laennec. De l'auscultation médiate ou traité du diagnostic des maladies des puomons et du coeur fondé principalment sur ce nouveau moyen d'exploration. Paris: Brosson & Chaudé, 1819.
- Zhao L, Peng L, Wu B, et al. Effects of dynamic hyperinflation on exercise capacity and quality of life in stable COPD patients. Clin Respir J 2016;10:579-88. [Crossref] [PubMed]
- Rossi A, Aisanov Z, Avdeev S, et al. Mechanisms, assessment and therapeutic implications of lung hyperinflation in COPD. Respir Med 2015;109:785-802. [Crossref] [PubMed]
- Brantigan OC, Kress MB, Mueller EA. The surgical approach to pulmonary emphysema. Diseases of the Chest 1961;5:485-99. [Crossref]
- Cooper JD. The History of Surgical Procedures for Emphysema. Ann Thorac Surg 1997;63:312-9. [Crossref] [PubMed]
- Criner GJ, Cordova FC, Furukawa S, et al. Prospective Randomized Trial Comparing Bilateral Lung Volume Reduction Surgery to Pulmonary Rehabilitation in Severe Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 1999;160:2018-27. [Crossref] [PubMed]
- Geddes D, Davies M, Koyama H, et al. Effect of lung-volume-reduction surgery in patients with severe emphysema. N Engl J Med 2000;343:239-45. [Crossref] [PubMed]
- Goldstein RS, Todd TR, Guyatt G, et al. Influence of lung volume reduction surgery (LVRS) on health related quality of life in patients with chronic obstructive pulmonary disease. Thorax 2003;58:405-10. [Crossref] [PubMed]
- Hillerdal G, Löfdahl CG, Ström K, et al. Comparison of lung volume reduction surgery and physical training on health status and physiologic outcomes. Chest 2005;128:3489-99. [Crossref] [PubMed]
- Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume–reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059-73. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Mineo TC. Comparative results of non-resectional lung volume reduction performed by awake or non-awake anesthesia. Eur J Cardiothorac Surg 2011;39:e51-8. [Crossref] [PubMed]
- van Agteren JE, Carson KV, Tiong LU, et al. Lung volume reduction surgery for diffuse emphysema. Cochrane Database Syst Rev 2016;10. [PubMed]
- Sciurba FC, Ernst A, Herth FJ, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med 2010;363:1233-44. [Crossref] [PubMed]
- Herth FJ, Noppen M, Valipour A, et al. Efficacy predictors of lung volume reduction with Zephyr valves in a European cohort. Eur Respir J 2012;39:1334-42. [Crossref] [PubMed]
- Davey C, Zoumot Z, Jordan S, et al. Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomised controlled trial. Lancet 2015;386:1066-73. [Crossref] [PubMed]
- Klooster K, ten Hacken NH, Hartman JE, et al. Endobronchial Valves for Emphysema without Interlobar Collateral Ventilation. N Engl J Med 2015;373:2325-35. [Crossref] [PubMed]
- Valipour A, Slebos DJ, Herth F, et al. Endobronchial Valve Therapy in Patients with Homogeneous Emphysema. Results from the IMPACT Study. Am J Respir Crit Care Med 2016;194:1073-82. [Crossref] [PubMed]
- Kemp SV, Slebos DJ, Kirk A, et al. A Multicenter Randomized Controlled Trial of Zephyr Endobronchial Valve Treatment in Heterogeneous Emphysema (TRANSFORM). Am J Respir Crit Care Med 2017;196:1535-43. [Crossref] [PubMed]
- van Agteren JE, Hnin K, Grosser D, et al. Bronchoscopic lung volume reduction procedures for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017;2. [PubMed]
- Ninane V, Geltner C, Bezzi M, et al. Multicentre European study for the treatment of advanced emphysema with bronchial valves. Eur Respir J 2012;39:1319-25. [Crossref] [PubMed]
- Eberhardt R, Gompelmann D, Schuhmann M, et al. Complete unilateral vs partial bilateral endoscopic lung volume reduction in patients with bilateral lung emphysema. Chest 2012;142:900-8. [Crossref] [PubMed]
- Wood DE, Nader DA, Springmeyer SC, et al. The IBV Valve trial: a multicenter, randomized, double-blind trial of endobronchial therapy for severe emphysema. J Bronchology Interv Pulmonol 2014;21:288-97. [Crossref] [PubMed]
- Shah PL, Zoumot Z, Singh S, et al. Endobronchial coils for the treatment of severe emphysema with hyperinflation (RESET): a randomised controlled trial. Lancet Respir Med 2013;1:233-40. [Crossref] [PubMed]
- Deslée G, Mal H, Dutau H, et al. Lung Volume Reduction Coil Treatment vs Usual Care in Patients With Severe Emphysema: The REVOLENS Randomized Clinical Trial. JAMA 2016;315:175-84. [Crossref] [PubMed]
- Sciurba FC, Criner GJ, Strange C, et al. Effect of Endobronchial Coils vs Usual Care on Exercise Tolerance in Patients With Severe Emphysema: The RENEW Randomized Clinical Trial. JAMA 2016;315:2178-89. [Crossref] [PubMed]
- Snell G, Herth FJ, Hopkins P, et al. Bronchoscopic thermal vapour ablation therapy in the management of heterogeneous emphysema. Eur Respir J 2012;39:1326-33. [Crossref] [PubMed]
- Herth FJ, Valipour A, Shah PL, et al. Segmental volume reduction using thermal vapour ablation in patients with severe emphysema: 6-month results of the multicentre, parallel-group, open-label, randomised controlled STEP-UP trial. Lancet Respir Med 2016;4:185-93. [Crossref] [PubMed]
- Shah PL, Gompelmann D, Valipour A, et al. Thermal vapour ablation to reduce segmental volume in patients with severe emphysema: STEP-UP 12 month results. Lancet Respir Med 2016;4:e44-5. [Crossref] [PubMed]
- Come CE, Kramer MR, Dransfield MT, et al. A randomised trial of lung sealant versus medical therapy for advanced emphysema. Eur Respir J 2015;46:651-62. [Crossref] [PubMed]
- Shah PL, Slebos DJ, Cardoso PF, et al. Bronchoscopic lung-volume reduction with Exhale airway stents for emphysema (EASE trial): randomised, sham-controlled, multicentre trial. Lancet 2011;378:997-1005. [Crossref] [PubMed]
- Slebos DJ, Shah PL, Herth FJ, et al. Endobronchial Valves for Endoscopic Lung Volume Reduction: Best Practice Recommendations from Expert Panel on Endoscopic Lung Volume Reduction. Respiration 2017;93:138-50. [Crossref] [PubMed]
- Shah PL, Herth FJ, van Geffen WH, et al. Lung volume reduction for emphysema. Lancet Respir Med 2017;5:147-56. [Crossref] [PubMed]


