A comparison between laryngeal mask airway and endotracheal intubation for anaesthesia in adult patients undergoing NUSS procedure
Introduction
With stable growth of the chest skeleton in adults (age >16), placing an internal support frame in the thoracic cavity of patients with pectus excavatum (PE) may not have an effect on its later development. Furthermore, the procedure applied at this relatively mature age might be beneficial for re-shaping the chest. As a result, the video-assisted thoracic surgery (VATS)-NUSS procedure has been widely applied as a standard procedure for treating adult patients with PE, and abundant clinical cases have demonstrated its successful effects (1,2). In traditional opinions, airway management with endotracheal intubation (ETT) for general anaesthesia is necessary for the NUSS procedure. Either one or dual-lung ventilation can be applied. For dual-lung ventilation, artificial pneumothorax is applied to expose the operating field by the surgeon with CO2 perfused into the pleural cavity (3,4). However, due to an abnormal thoracic cavity, patients with PE usually suffer some severe complications before surgery, such as repeated respiratory system infection and further pulmonary dysfunction. In addition, the ETT procedure may also increase the incidence of or aggravate these complications (5,6). To avoid the occurrence of complications induced by ETT, some surgeons are seeking an alternative method and trying to apply laryngeal mask airway (LMA) for airway management in VATS for treating spontaneous pneumothorax. These attempts were successful and preliminarily showed the promising prospect of the application of LMA for airway management in the area of minimally invasive thoracic surgery (7). However, we need to be concerned that this conclusion was only from a small number of clinical cases, and the study lacked a prospective and comprehensive comparison with ETT; thus, the feasibility and safety of LMA still needs to be further confirmed. To provide strong clinical evidence and to further evaluate the feasibility and safety of LMA application in the VATS-NUSS procedure, it is necessary for us to design a randomized control study in which the effects of LMA and traditional ETT are compared.
Methods
Trial design
This project was designed as a prospective, randomized controlled study and has been approved by the Human Ethics Committee of Guangdong General Hospital (Guangzhou, China). We used statistical software (IBM SPSS Statistics v22.0, IBM, Armonk, USA) to produce a computer-generating code for each enrolled patient and then designed the grouping by using the simple random sampling method. Enrolled patients were randomly distributed to the LMA and ETT groups, and then the data were collected until the total sample number was 60 and the sample in each group reached 30. The grouping information was stored as code and kept by a third party person who was later responsible for data analysis.
Patient recruitment
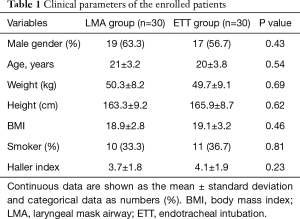
Written informed consent was obtained after the patients had been informed about the investigational nature of the study, the potential risks, and the predictable outcomes. Eligible patients aged 17 to 24 with a medical record in the hospital between 01 Sep 2016 and 01 Mar 2017 were recruited. The eligibility criteria included the following: patients (age >16) diagnosed with PE by chest radiographic manifestations or computed tomography and those who were willing to be treated by VATS-NUSS. Exclusion criteria: (I) patients with a preoperative anaesthesia assessment score higher than III (American Society of Anesthesiologists, ASA); (II) patients with severe circulation, liver or kidney dysfunction or those intolerant of surgery; (III) patients with low levels of pulmonary function (FEV1 <60%) or with infection in the respiration tract; (IV) psychiatric patients who needed long-term medication treatment or patients with diseases of the central nervous system; (V) patients with history of anaesthetic allergy; (VI) obese patients whose body mass index (BMI) was higher than 29.9. Then, we selected eligible patients and randomly distributed them into the LMA and ETT groups. The data from the enrolled patients who suffered severe complications during surgery such as arrhythmia, electrolyte disorders or uncontrolled blood loss and needed to convert to open-chest surgery were excluded from our final analysis. Based on “rule of thumb” in statistics and a previously published article (8), at least 30 patients in each group are considered adequate for statistical analysis. We were recruiting patients until the sample size for each group reached our ideal number. The clinical parameters of enrolled patients in the LMA and ETT groups are shown in Table 1.
Full table
Anaesthesia preparation, induction, and maintenance
Preparation: all the patients lay in supine position after being sent to the surgery room. Their vital signs, such as electrocardiogram, pulse oximetry, non-invasive blood pressure, respiratory rate, and electroencephalogram (EEG) intensity, were monitored before the induction of anaesthesia. The vein line was established for rehydration, and scopolamine at 0.005 mg/kg was infused intravenously for 30 min for premedication before anaesthesia induction. The devices for the induction and maintenance of anaesthesia were prepared including fibreoptic bronchoscopy, laryngeal mask and endotracheal tubes.
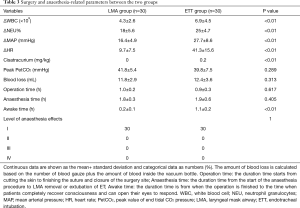
Induction and maintenance: anaesthesia in the LMA group was induced by intravenous injection of 0.05–0.1 mg/kg of midazolam, 2 µg/kg of fentanyl and pump infusion of propofol with a target concentration in the plasma of 1.5–2 µg/mL. The correctly sized laryngeal mask was chosen based on the patients’ weight and placed in the airway by the anaesthesiologist after patients lost consciousness. The cuff was inflated to the maximum volume, and it was confirmed that there was no air leakage. After, the airway device was attached to the anaesthetic circuit. Anaesthesia was maintained by pump infusion of propofol and 0.05~0.1 µg/kg/min of remifentanil, and the depth of anaesthesia was adjusted based on the EEG and circulatory parameters. For the ETT group, intravenous injection of 3–4 µg/kg of fentanyl plus the same dosage of midazolam and propofol as that in the LMA group was administered to induce anaesthesia. Intravenous injection of 0.2 mg/kg cisatracurium was applied to relax the muscles after patients lost consciousness. Then, a single-lumen endotracheal tube was placed by the anaesthesiologist. The patients were continually pump-infused with propofol (target plasma concentration 2–4 µg/mL), remifentanil (0.1~0.2 µg/kg/min) and cisatracurium (2 µg/kg/min). The ventilator mode of synchronized intermittent mandatory ventilation (SIMV) was set for the LMA group. In addition, volume preset ventilation mode (VPV) was set for the ETT patients. As shown in Table 2, the ventilator parameters for both groups were similar. The peak pressure of ventilation in both groups was controlled no higher than 40 cmH2O; the leak pressure for the LMA group was 18 mmHg. The oxygen saturation in patients was maintained higher than 95%, and the depth of anaesthesia was within 50–60.

Full table
Termination: a total of 2 µg/kg fentanyl was added intravenously prior to closure of the chest cavity in both groups. In the ETT group, the muscle relaxant stopped pumping at the same time; 0.03 mg/kg neostigmine plus 0.01 mg/kg atropine were applied intravenously to antagonize the effect of the muscle relaxant. All the patients were sent to the recovery room after surgery.
Criteria for extubation: patients could respond by opening their eyes; spontaneous respiratory rate was regular and 14–20/min; breath sounds in both lungs were normal; oxygen saturation was higher than 95%. All the patients were checked for hoarseness and pharynx discomfort after they recovered consciousness.
Surgical procedure
The details of the VATS-NUSS procedure we used have been described previously (9). First, after induction of anaesthesia, the patients were positioned supine on the right side of the table with both arms abducted approximately 70° from the chest wall. This position not only allowed good access to the lower chest wall and did not cause brachial plexus injury but also ensured free movement of the thoracoscope; Second, the right end of the Nuss bar had a longer shape than the left end for bar stabilization. Third, a 5-mm trocar was inserted through the same incision sites on the right side to maximize visualization. Fourth, to improve visualization, CO2 was insufflated through the trocar, and the pressure was maintained from 3 to 5 mmHg to keep the lungs out of the operative field. Fifth, when creating the retrosternal tunnel with an introducer, the thoracic entry and exit sites were placed close to the sternum to prevent disruption of the intercostal muscles. Sixth, after the retrosternal tunnel had been created, the introducer was pushed through the left incision and lifted in an anterior direction to pull the sternum and anterior chest wall out of their depressed position. Then, the malformed ribs were pressed forcefully several times to shape them. Next, after a 28-Fr transparent chest drain was fitted to the tip of the introducer and withdrawn from the right incision, the left end of the shaped Nuss bar was fitted to the right end of the drain hollow. Again, the drain was withdrawn from the left incision and guided the Nuss bar across the critical retrosternal tunnel carefully under thoracoscopic guidance. The bar was rotated through 180° with the sternum being pushed upward, and the PE was completely corrected. Seventh, one stabilizer was placed on the right side as close as possible to the thoracic entry sites to avoid rotation. Additionally, the bar and the stabilizer were secured on the muscles with polyester sutures (7.0 metric, ETHICON, INC 2007, MB66.P33). Eighth, at the end of the procedure, a 12-Fr urethral catheter was placed through the right incision site (and the left incision site if left pneumothorax occurred) before the incisions were closed to evacuate the pneumothorax by expanding the lungs with positive pressure ventilation. Ninth, if two bars were needed, the surgical procedure for the second bar was approximately the same as above, with a few differences: the left end of the Nuss bar was longer than the right end, and the stabilizer was placed on the left side because it was difficult to place the two stabilizers on one side.
Postoperative care
The patients were required to remain in a supine position. Both oral and pump-infusing nonsteroidal analgesics were administered as routine. A chest roentgenogram was performed the next morning after surgery to evaluate the effect of the procedure. The patients recovered their intake of food and water based on their requirements. All the postoperative complications were recorded.
Data collection and statistical analysis
All the clinical data were collected from the institutional database, the anaesthesia and surgical notes, and the medical and nursing records. The collected data included: difference in blood cell counts (ΔWBC) and percentage of neutrophil granulocytes (ΔNEU%) between the day before surgery and 1 day after surgery; the variation of haemodynamic parameters during surgery, such as mean arterial pressure (ΔMAP) and heart rate (ΔHR); blood gas analysis during surgery, including arterial blood PH, partial pressure of oxygen in arterial blood (PaO2), partial pressure of carbon dioxide in arterial blood (PaCO2) and peak of end tidal CO2 pressure (PetCO2); Anaesthesia effect score; Surgery and anaesthesia-related parameters, including operation time (the duration time starts from cutting the skin to suture finish and closure of surgery site), anaesthesia time (the duration time from the start of the anaesthesia procedure to LMA removal or extubation of ET), amount of blood loss (based on the number of blood gauze plus the amount of blood inside the vacuum bottle), awake time (the duration time from when the operation is finished to the time when patients completely recover consciousness and can open their eyes to respond), and dosage of muscle relaxant used; postoperative parameters indicating the recovery of patients after surgery. To evaluate and compare the anaesthesia effect between the ETT and LMA groups, we designed the anaesthesia effect score. There are four levels of the anaesthesia effect. Level 1: the anaesthesia effect is satisfying; the patient is resting without any pain, and the haemodynamic level is stable during surgery; the surgery process is going well. Level 2: the anaesthesia effect is still acceptable, but the dosage of analgesic, sedative and muscle relaxant still need further adjustment; haemodynamic fluctuation can be seen during surgery but does not affect the surgery process. Level 3: the anaesthesia effect is not good; the patient is restless, and the haemodynamic fluctuation is unstable during surgery. There is no improvement even if the anaesthetic is adjusted. The surgery is not easily handled. Level 4: the current anaesthesia protocol is not suitable for surgery. Random variables of clinical data were shown as the percentage or mean ± standard deviation. The chi-square test and unpaired t-test were applied to analyse the difference between the LMA and ETT groups. IBM SPSS Statistics v22.0 (IBM, Armonk, USA) was used for the data analysis and to calculate P value. The results were considered significantly different when the P value was less than 0.05.
Results
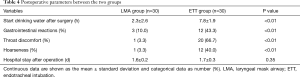
All the selected patients with PE went through the video-assisted thoracoscopic surgery for NUSS procedure (VATS-NUSS) successfully. After randomized grouping, we did not find a significant difference between the LMA and the ETT groups in terms of the physiological parameters and population features of the enrolled patients, such as age, weight, height, and Haller index as well as percentage of male gender and smokers (Table 1), demonstrating that the LMA and ETT groups have similar clinical population characteristics. Overall, no severe surgical complications were observed in any patient; the surgical and anaesthesia procedures in each case achieved satisfying results (Tables 3,4). For the LMA group, all the patients had the laryngeal mask placed properly and successfully. Neither displacement of the laryngeal mask nor conversion to endotracheal incubation occurred during surgery. The patients in the ETT group had endotracheal tubes placed for airway management successfully as well. No respiratory complications, such as airway obstruction or bronchospasm, occurred in any enrolled patients during surgery, ET extubation or LMA removal. Additionally, we did not see postoperative nausea, reflux, or aspiration (Table 4). There was no observed case that required changing the surgical procedure to open the thoracic cavity, and there was no case of death case.
Full table
Full table
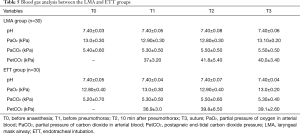
First, compared to the ETT group, the variation in blood cell count and percentage of neutrophil granulocytes (ΔWBC and ΔNEU%) in patients during surgery were much smaller in the LMA group. Additionally, patients in the LMA group showed more stable haemodynamic parameters during surgery, such as HR and MAP, than that in the ETT group (Table 3). Moreover, we found that for patients in the LMA group, routine application of the muscle relaxant was unnecessary, while patients in the ETT group still required administration with a muscle relaxant to ensure satisfying anaesthesia effects (Table 3). During surgery, no significant difference was found between the LMA and ETT group in terms of blood gas analysis, such as arterial PH, arterial partial oxygen and carbon dioxide pressure (PaO2 and PaCO2), and postapneic end-tidal carbon dioxide pressure (PetCO2) at different time points (Table 5). Additionally, the amount of blood loss, anaesthesia and surgical procedure time as well as anaesthesia effect were similar between the two groups (Table 3). Finally, we found that awakening time after surgery was significantly shorter in patients in the LMA group than the ETT group. During in-patient care after surgery, patients in the LMA group recovered their food and water intake much earlier than in the ETT group. Meanwhile, compared to the ETT group, patients in the LMA group had significantly lower incidence of gastrointestinal reactions, throat discomfort and hoarseness. However, there was no obvious difference in days of inpatient care after surgery between the LMA and ETT groups (Table 4).
Full table
Discussion
Thus far, this is the first clinical prospective investigation formally comparing the different methods of airway management between LMA and ETT in general anaesthesia for adult VATS-NUSS procedure in a randomized, controlled and point-to-point method. Some patients with PE in our hospital are already at adult age. However, with the long-term effects of thoracic deformity, most of these patients suffer severe dysfunction of important organs such as those of the cardiopulmonary system. These patients usually come to the hospital with respiratory infections that may multiply, increasing the risk of surgery (10,11). Hence, airway management in general anaesthesia is considered a top priority in patients with PE during surgery. In traditional VATS-NUSS procedures, in order to create enough space to operate, surgeons usually place the intubation tube in one side of the lungs and infuse CO2 inside the thoracic cavity to induce artificial pneumothorax (4). However, utilizing such a method to manage the airway may cause ventilator-associated lung injury (VALI). Additionally, the intubation tube itself may also induce mechanical stretch-associated lung injury and lower respiratory tract infection (12,13). Moreover, ETT may cause several complications, such as airway spasm, vocal cord paralysis and laryngeal edema (14). In addition to ETT, LMA for general anaesthesia is another alternative method of airway management that is safer than epidural anaesthesia. Compared to ETT, LMA shows superiority in certain aspects, which makes it specifically suitable for application in some small thoracic surgeries. There have been clinical cases around the world in which LMA was successfully applied in the VATS procedure for patients with spontaneous pneumothorax or thoracic spine orthopaedics (7,8,15,16). We discovered from clinical practice that LMA possesses multiple advantages for airway management: easy to operate; no laryngoscope required; the whole procedure took only approximately 20 seconds and usually could be accomplished successfully. Hence, if LMA can be applied for the VATS-NUSS procedure instead of traditional ETT, the risk of airway management during surgery would be undoubtedly dramatically decreased. Considering that the time of the VATS-NUSS procedure is as short as 1 h and that it is a well-developed procedure, LMA for airway management is supposed to meet the temporal requirement of VATS-NUSS theoretically. It is worthy for us to compare the different outcomes between LMA and traditional ETT in airway management for VATS-NUSS procedure.
All the enrolled patients went through the VATS-NUSS procedure successfully. No patients needed emergency rescue due to anaesthesia or conversion to ETT procedure during surgery. Additionally, there was no significant difference between the LMA and ETT groups, comparing anaesthesia and surgical time, amount of blood loss, and blood gas analysis, including arterial blood PH, PaO2, PaCO2 and PetCO2 levels. The trend of PetCO2 is clinically meaningful to consider whether the LMA technique should be applied or not. The anaesthetic effect was satisfying in both the LMA and ETT groups. All the results preliminarily demonstrated that LMA in general anaesthesia might be suitable for the standard VATS-NUSS procedure.
In the LMA group, SIMV was selected for ventilation in general anaesthesia, which could effectively prevent hypoxemia via increasing the respiratory rate, even if the tidal volume decreased during artificial pneumothorax. Meanwhile, moderate artificial pneumothorax not only ensures enough operating space for the surgeon but also decreases the activity amplitude of lung lobes that maximally protected lobes’ physical function. The laryngeal mask is placed in the throat and larynx but not into the glottis and trachea; thus, patients are usually more tolerant of LMA because of no stimulation to the epiglottis. Moreover, not muscle relaxant administration but only a small amount of sedatives and analgesics are needed in LMA patients. In contrast to LMA, traditional ETT required deeper anaesthesia to have fully relaxed muscles and satisfactory mouth opening as well as inhibition of reflection in the throat and larynx. We discovered from clinical practice that compared to the ETT group, only a half dose of analgesics was needed to reach the desired effect for the induction of anaesthesia in the LMA group. During maintenance of anaesthesia, blood concentration of sedatives and analgesics in the LMA patients was approximately 50% lower than in the ETT patients. There was a positive correlation between the dosage of anaesthetics used and the awakening time. Therefore, less anaesthetics were used in the LMA group; the patients’ awakening time after anaesthesia was much shorter than the ETT group.
LMA is a non-invasive procedure effectively preventing vocal cord and tracheal mucosa from mechanical injury. As a result, patients in the LMA group suffered less stress responses and postoperative complications. With no effect on cilia activity and with less secretion produced in the tracheal mucosa, LMA was able to dramatically decrease the occurrence of postoperative complications that usually happen in patients with ETT, such as sore throat, laryngeal edema, vocal cord injury and paralysis of the recurrent laryngeal nerve (17). On the other hand, a smaller dosage of anaesthetics may extenuate the side effects and further alleviate the gastrointestinal response as well as prevent the occurrence of reflux and aspiration, which are beneficial for patients to recover their own gastrointestinal function and enables patients to resume eating and drinking as soon as possible.
Overall, we still can discover some differences between these two methods of airway management, considering the pathophysiological impact on patients. First, we found that alternations in haemodynamic parameters, such as the mean arterial pressure and heart rate during surgery (ΔMAP and ΔHR) in the LMA group were much smaller than in the ETT group, indicating that patients suffered less stimulation from the LMA procedure, and their stable haemodynamics were easier to maintain, even if fewer anaesthetics were used. In contrast, ETT and removal of the intubation tube may induce dramatic vibration of blood pressure and heart rate even though patients were already concurrently administered with relatively high dose of sedatives, analgesics and muscle relaxants. Second, the change in ΔWBC and ΔNEU% in the LMA group showed more stability than in the ETT group. We assumed that the aseptic inflammatory response caused by mechanical stimulation from anaesthesia and the surgical procedure may underlie the increase in WBC and NEU% after surgery. Both the LMA and ETT groups showed similarity in terms of operation time and surgical protocol. However, with no impact on patients’ trachea, compared to the ETT group, the LMA group showed obviously less inflammatory responses after surgery and a shorter stress response time. Meanwhile, patients in the LMA group resumed eating and drinking earlier so that they could easily recover stable haemodynamics. In summary, compared to traditional ETT, LMA interfered less in the physiological environment of the respiratory system and enabled patients to recover sooner after surgery.
LMA showed promising advantages in clinical practice; it is a non-invasive procedure that is easy to operate and has good compliance from patients. However, some problems also cannot be ignored. First, the location of the laryngeal mask might change during surgery, which could induce airway leaking or a sudden increase in airway pressure. In this case, we need to adjust the patient’s head or inflatable volume in cuff to correct the location of the laryngeal mask. Without any improvement, conversion to ETT would be necessary. Second, since LMA increases the risks of reflux and aspiration, patients are required to be strictly fasted before surgery. Narrow airway and severe infection in the upper respiratory tract should be considered contraindications for LMA. Finally, sputum could not be sucked out from the airway once LMA was applied, so secretions from the airway should be kept in a limited amount during the whole procedure. Otherwise, the bronchus might be blocked, and immediate conversion to ETT would be needed for sucking the sputum. Thus far, the future application of LMA for thoracic surgery is still being explored, and its indications still need to be carefully considered. We may first attempt to apply this novel ventilation in some small thoracic surgeries, such as hand sweat syndrome, minimally invasive PE orthopaedic, spontaneous pneumothorax and wedge resection for marginal pulmonary nodules. Then, we would be able to accumulate more and more experience in airway management, anaesthesia and surgery. Once there are enough evidence-based clinical cases, we can go further and attempt to apply LMA in larger surgeries such as operations for lung cancer.
Conclusions
In summary, LMA may be a promising method for airway management alternatives to traditional ETT. Much less anaesthetics and stimulation were used on patients with LMA, which further increases the stability of the anaesthetic effect and improves patient recovery after surgery. Abundant clinical evidence demonstrates that LMA could be feasible and safe as ventilation for general anaesthesia in the VATS-NUSS procedure. On the premise of strictly controlling its indicators, LMA may be a better choice for airway management in the adult VATS-NUSS procedure.
Acknowledgements
Funding: This study was funded by Guangdong Natural Science Foundation (grant number S2013010011516).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Human Ethics Committee of Guangdong General Hospital (Guangzhou, China) of No. 2015285H. Written informed consent was obtained from the patients after they had been informed about the investigational nature of the study, the differences between LMA and ETT, the possibility that conversion to an ETT may be necessary during the procedure, and the foreseeable outcomes.
References
- Nuss D, Kelly RE, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Nuss D, Kelly RE. The Minimally Invasive Repair of Pectus Excavatum. Oper Tech Thorac Cardiovasc Surg 2014;19:324-47. [Crossref]
- Futagawa K, Suwa I, Okuda T, et al. Anesthetic management for the minimally invasive Nuss procedure in 21 patients with pectus excavatum. J Anesth 2006;20:48-50. [Crossref] [PubMed]
- Mavi J, Moore DL. Anesthesia and analgesia for pectus excavatum surgery. Anesthesiol Clin 2014;32:175-84. [Crossref] [PubMed]
- Koumbourlis AC. Pectus excavatum: pathophysiology and clinical characteristics. Paediatr Respir Rev 2009;10:3-6. [Crossref] [PubMed]
- Griesdale DE, Henderson WR, Green RS. Airway management in critically ill patients. Lung 2011;189:181-92. [Crossref] [PubMed]
- Ambrogi MC, Fanucchi O, Gemignani R, et al. Video-assisted thoracoscopic surgery with spontaneous breathing laryngeal mask anesthesia: preliminary experience. J Thorac Cardiovasc Surg 2012;144:514-5. [Crossref] [PubMed]
- Du X, Mao S, Cui J, et al. Use of laryngeal mask airway for non-endotracheal intubated anesthesia for patients with pectus excavatum undergoing thoracoscopic Nuss procedure. J Thorac Dis 2016;8:2061-7. [Crossref] [PubMed]
- Zhang DK, Tang JM, Ben XS, et al. Surgical correction of 639 pectus excavatum cases via the Nuss procedure. J Thorac Dis 2015;7:1595-605. [PubMed]
- Saleh RS, Finn JP, Fenchel M, et al. Cardiovascular magnetic resonance in patients with pectus excavatum compared with normal controls. J Cardiovasc Magn Reson 2010;12:73. [Crossref] [PubMed]
- Lawson ML, Mellins RB, Paulson JF, et al. Increasing severity of pectus excavatum is associated with reduced pulmonary function. J Pediatr 2011;159:256-61.e2. [Crossref] [PubMed]
- Bouadma L, Wolff M, Lucet JC. Ventilator-associated pneumonia and its prevention. Curr Opin Infect Dis 2012;25:395-404. [Crossref] [PubMed]
- Li Bassi G, Torres A. Ventilator-associated pneumonia: role of positioning. Curr Opin Crit Care 2011;17:57-63. [Crossref] [PubMed]
- Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth 2012;109 Suppl 1:i68-i85. [Crossref] [PubMed]
- Cai K, Wang X, Ye J, et al. Laryngeal mask anesthesia in video-assisted thoracoscopic surgery for pulmonary bulla: comparison with intubation anesthesia. Nan Fang Yi Ke Da Xue Xue Bao 2013;33:756-60. [PubMed]
- Li P, Liang W, Gu H. One-lung ventilation using Proseal laryngeal mask airway and Arndt endobronchial blocker in paediatric scoliosis surgery. Br J Anaesth 2009;103:902-3. [Crossref] [PubMed]
- Taheri A, Hajimohamadi F, Soltanghoraee H, et al. Complications of using laryngeal mask airway during anaesthesia in patients undergoing major ear surgery. Acta Otorhinolaryngol Ital 2009;29:151-5. [PubMed]


