Reduced complexity of uniportal video-assisted thoracoscopic left upper sleeve lobectomy
Introduction
In recent years improvements in thoracoscopic instrumentation and technology including high definition cameras and miniaturized energy devices have led to uniportal video-assisted thoracoscopic (VATS) lobectomy becoming more common (1). However, uniportal VATS sleeve lobectomy (SL) is more difficult, and the competence threshold for performing such surgery is high, so only a small number of expert VATS surgeons have mastered it (2). Furthermore, the left upper SL is usually more complicated due to the presence of the aortic arch, the bigger size of the pulmonary artery and absence of the intermediate bronchus (3). In this article, we describe improvements to bronchial exposure and simplification of the anastomosis technique with existing equipment which reduces the complexity of uniportal VATS left upper SL.
Operative techniques
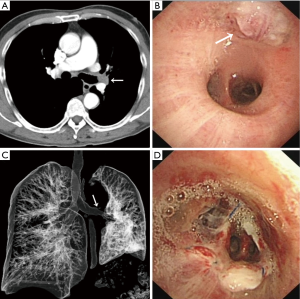
A 64-year-old male smoker without significant comorbidities was found to have a left upper lobe (LUL) lesion during incidental computed tomography (CT) screening. The scan revealed consolidation of the LUL with no hilar or mediastinal lymphadenopathy (Figure 1). Flexible bronchoscopy showed a solid tumor obstructing the origin of the LUL bronchus (Figure 1B), the left main bronchus and left lower bronchus being grossly normal. A biopsy revealed a squamous cell carcinoma. After excluding distant metastasis, the patient was referred for surgery. A minimally invasive LUL sleeve lobectomy using a uniportal approach was proposed on December 28th 2017.
An anterior incision, approximately 4 cm long, was created over the 5th intercostal space. The surgical procedure can be summarized in four steps:
Performing lymph node dissection
Lymphadenectomy was firstly performed on nodes in groups 5 and 6 in order to assist in the exposure of the left upper pulmonary vein and pulmonary artery, followed by paratracheal and subcarinal lymphadenectomy, to achieve bronchial exposure. Because release maneuvers of the pulmonary ligament needed to be performed in advance, lymphadenectomy of groups 8 and 9 nodes was performed simultaneously.
Lobectomy process
Because of incomplete interlobar fissure, the left upper pulmonary vein was firstly dissected, followed by the pulmonary artery, which was technically challenging due to inflammation in the tissues in addition to the presence of lymph nodes that obstructed the planes of dissection. Preliminary suspension of the pulmonary artery was performed to expose the left second carina and surrounding tissue (Figure 2), then the proximal and distal bronchi were separated sufficiently distant from the tumor. The left main bronchus was divided first, followed by the left lower bronchus. After dissecting the lingular artery, the fissure was resolved and the LUL was removed using an endobag.
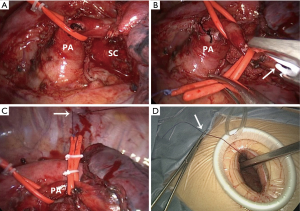
Pulmonary artery suspension devices
To fully prepare the site prior to creation of the anastomosis, another device was used for suspending the pulmonary artery (see Figure 3) to expose both bronchial extremities, as follows: Firstly, a section of catheter connected to silk suture was used to surround the left pulmonary artery with the help of hem-o-lok ligation clips (Figure 2B). The silk suture was attached to the parietal pleura to form a pulley-like device to lift the left pulmonary artery (Figure 2C). Finally the end of the silk suture was fed out through the incision and fixed externally (Figure 2D). The tension of the suspension devices could be adjusted as required before fixation of the silk suture.

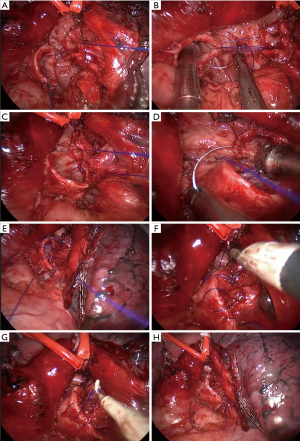
The anastomosis process
After frozen-section examination confirmed negative margins, a simplified method of suture-tensionless continuous suture (see Figure 4) was used, which only required the tying of one final knot (known as a one-knot suture). We used 3-0 prolene suture material which facilitated smoothing the suture and tightening it before tying. An end-to-end anastomosis was performed starting with a posterior stitch in the cartilaginous-membranous junction with no knots (Figure 5A). A continuous suture was initiated in the membranous portion from posterior to anterior (Figure 5B,C) followed by another continuous suture (using the same suture) from posterior to anterior for the cartilaginous part (Figure 5D,E) then tied with the running suture of the membranous part. The suture required tightening at multiple sites using a coagulation hook (Figure 5F,G) before a knot pusher was used to tie the knot outwards (Figure 5H).

After confirmation of the absence of an air leak using underwater insufflation, the incision was closed with a double-embedding stitching method (6) (see Figure 6). A 24-F chest tube was placed in the posterior end of the incision before it was closed. Blood loss was 120 mL and duration of surgery was 305 minutes.
Postoperative recovery was uneventful. The 24F chest tube was removed after 3 days. Postoperative chest CT showed effective lung expansion 5 days postoperatively (Figure 1C) and bronchoscopy demonstrated that the anastomosis had been created expertly (Figure 1D). The patient was discharged after 11 days. Pathological analysis showed keratinizing squamous cell carcinoma with involvement of only one parabronchial lymph node.
Comments
Since the first thoracoscopic sleeve lobectomy was performed by Santambrogio and colleagues (8), this surgery is no longer a contraindication for thoracoscopy. With the development of uniportal thoracoscopic instrumentation and technology, a few instances of uniportal thoracoscopic sleeve lobectomy have been reported (9-17). A small number of reports are due to the difficulty of surgical field exposure and the anastomosis process. In particular, we found only ten cases (including five cases of double sleeve lobectomy) of left side uniportal VATS sleeve lobectomy in these reports (10,11,13,15,16).
Regarding the experience threshold for uniportal VATS sleeve lobectomy, some authors suggest at least 200 uniportal VATS lobectomies and 20 open sleeve procedures should be performed before attempting a uniportal thoracoscopic sleeve resection (2,10,18). These requirements deter most thoracic surgeons from attempting such surgery. We hypothesized that improvements, such as ideal exposure or appropriate anastomosis, could simplify the procedure, and a surgeon with some experience in uniportal VATS lobectomy (perhaps more than 50 cases) would be able to perform the procedure. The author (L Huang), 35 years old, that had performed about 50 uniportal VATS lobectomies and 2 open sleeve procedures previously, safely performed left upper sleeve lobectomy through uniportal VATS. We identified three aspects that improved probability of success: performing lymph node dissection firstly, installing pulmonary artery suspension devices and using a one-knot suture.
Some surgeons suggest that complete lymph node dissection should be performed prior to initiating the anastomosis (10), in order to expose the brochus and prevent injury or disruption to the anastomotic stoma (19). We further advocate completion of lymph node dissection prior to dividing the bronchus to increase accuracy of the cutting positions.
Excellent exposure in this case was achieved primarily using left pulmonary artery suspension devices. This method greatly reduced interference from the pulmonary artery during creation of the anastomosis. The process is simple and fast. No additional instruments are required except for one catheter, several sutures and hem-o-lok ligation clips. One alternative technique involved lifting the trunk of the left pulmonary artery by threading a 1–0 silk suture through the posterior chest wall with a crochet needle in multiportal VATS (20).
Bronchial sleeve anastomosis can be performed with an interrupted or continuous suture. Placing interrupted sutures using a VATS approach is more complex and time-consuming than using a running suture (2). Current methods of deploying a running suture require two-point interrupted suturing (anterior and posterior wall, also called a two-knot anastomosis) (2,21). The simplified method described here is a tensionless continuous suture (one-knot suture), without the need to tie a knot until completion of the suture process. There are three benefits of one-knot suture: a reduction in the number of knots; easy examination of the required stitch distance which assists in avoiding air leaks; and, most importantly, needle angle can be adjusted by moving the bronchial stumps (Figure 5B,D), so uniportal thoracoscopic anastomosis can be achieved with general VATS suture skills. The main criticism may be that there is a possibility of retraction without fixing the two bronchial stumps in addition to suture loosening. For the former problem, we achieved good exposure of the stumps after lymphadenectomy and suspension of the pulmonary artery. For the latter, we achieved sufficient suture tension by tightening the suture at multiple sites and confirming the absence of air leaks using underwater insufflation. Andrade and colleagues (9) also suggest placing low-tension sutures, avoiding devascularization of the bronchial stumps and aligning the anastomosis.
In conclusion, we believe our case indicate that suspension of the pulmonary artery and a tensionless continuous suture can simplify uniportal VATS left upper sleeve lobectomy which lowers the threshold of experience for surgeons.
Acknowledgements
Funding: This work was supported by grants from Education Department of Zhejiang Province (Y201534184), National Natural Science Foundation of China (81572800, PW) and the Natural Science Foundation of Zhejiang Province (LY15H160041, PW).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: The authors have given written informed consent for publication from this patient.
References
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resectionsdagger. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Uniportal video-assisted thoracoscopic bronchoplastic and carinal sleeve procedures. J Thorac Dis 2016;8:S210-22. [PubMed]
- Huang L, Wu P, Zhao L, et al. Demonstrating suspending the pulmonary artery. Asvide 2018;5:578. Available online: http://www.asvide.com/article/view/25550
- Huang L, Wu P, Zhao L, et al. Demonstrating suture-tensionless continuous suture. Asvide 2018;5:579. Available online: http://www.asvide.com/article/view/25553
- Huang L, Zhao L, Li W, et al. Improved closure technique for uniportal video-assisted thoracic surgery: double-embedding stitching method. Ann Thorac Surg 2017;104:1760-1. [Crossref] [PubMed]
- Huang L, Wu P, Zhao L, et al. Demonstrating a double-embedding stitching method and the process of pulling out the chest tube. Asvide 2018;5:580. Available online: http://www.asvide.com/article/view/25555
- Santambrogio L, Cioffi U, De Simone M, et al. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest 2002;121:635-6. [Crossref] [PubMed]
- Andrade H, Joubert P, Vieira A, et al. Single-port right upper lobe sleeve lobectomy for a typical carcinoid tumour. Interact Cardiovasc Thorac Surg 2017;24:315-6. [PubMed]
- Yang Y, Guerrero WG, Algitmi I, et al. Complex uniportal video-assisted thoracoscopic sleeve lobectomy during live surgery broadcasting. J Thorac Dis 2016;8:1345-8. [Crossref] [PubMed]
- Lyscov A, Obukhova T, Ryabova V, et al. Double-sleeve and carinal resections using the uniportal VATS technique: a single centre experience. J Thorac Dis 2016;8:S235-41. [PubMed]
- Gonzalez-Rivas D, Marin JC, Granados JP, et al. Uniportal video-assisted thoracoscopic right upper sleeve lobectomy and tracheoplasty in a 10-year-old patient. J Thorac Dis 2016;8:E966-9. [Crossref] [PubMed]
- Chen H, Xu G, Zheng B, et al. Initial experience of single-port video-assisted thoracoscopic surgery sleeve lobectomy and systematic mediastinal lymphadenectomy for non-small-cell lung cancer. J Thorac Dis 2016;8:2196-202. [Crossref] [PubMed]
- Guido W, Gonzalez-Rivas D, Duang L, et al. Uniportal video-assisted thoracoscopic right upper sleeve lobectomy. J Vis Surg 2015;1:10. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Left lower sleeve lobectomy by uniportal video-assisted thoracoscopic approach. Interact Cardiovasc Thorac Surg 2014;18:237-9. [Crossref] [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- Agasthian T. Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg 2013;44:616-23. [Crossref] [PubMed]
- Xu G, Zheng W, Guo Z, et al. Complete video-assisted thoracoscopic surgery upper left bronchial sleeve lobectomy. J Thorac Dis 2013;5 Suppl 3:S298-300. [PubMed]
- Chen H, Huang L, Xu G, et al. Modified bronchial anastomosis in video-assisted thoracoscopic sleeve lobectomy: a report of 32 cases. J Thorac Dis 2016;8:2233-40. [Crossref] [PubMed]