Air leak pattern shown by digital chest drainage system predict prolonged air leakage after pulmonary resection for patients with lung cancer
Introduction
One of the most common causes of complications and protracted hospital stay after pulmonary resection is prolonged air leakage (1,2), thus management of a pulmonary air leak is an important clinical issue for thoracic surgeons (3). Air leak incidence is dependent on several factors, such as the surgical procedures employed and patient physiological characteristics, with such leakage considered to be prolonged when persisting for more than 5 days (4). A prolonged air leak often leads to increased complications, including longer drainage time, infection, and empyema, resulting in an increased period of hospitalization (5).
Digital pleural drainage systems utilize electronic sensors to measure and record air leakage from chest tubes, by which they can provide a graphical display of air leak trend over time (6). The ThopazTM chest drainage system (Medela, Switzerland) is a portable suction unit that features scientific digital flow recordings (7). The machine is equipped with digital display to provide objective data in real time as well as a 24-hour graph of air flow, which provides data for timely and objective decisions, including chest tube removal. In addition, clinicians can review air leak data transferred to a personal computer (PC) by a universal serial bus (USB) connection.
In the present study, we reviewed air leak data provided by a Thopaz device from patients who underwent pulmonary resection for lung malignancy and used that digital chest drainage system. From our findings, we divided the various postoperative air leak patterns into 4 groups; none, intermittent, decrease, and variable, and evaluated the correlation of those patterns with prolonged air leakage after surgery. The purpose of this study was to evaluate if the postoperative air leak patterns could predict prolonged air leakage after surgery.
Methods
Patients
Five hundred twenty-two patients underwent a pulmonary resection procedure for lung cancer between 2011 and 2015 at Osaka University Hospital. The Thopaz system was used after surgery in patients with pulmonary resection. Patients who underwent a pneumonectomy or wedge resection were excluded from the analysis. Patients who had severe adhesion or pulmonary emphysema were also excluded from the analysis because those patients basically required 2 chest drainage tubes for postoperative massive air leak or pleural effusion, thus the accurate analysis of air leak flow and trend was impossible. For the present study, data from Thopaz use in 299 patients who underwent a lobectomy or segmentectomy was saved and analyzed retrospectively. This study was approved by the Institutional Review Board of Osaka University Hospital (ID10026-3) and written informed consent was obtained from all patients.
Operation procedure
The surgical procedures were performed using a muscle sparing anterolateral thoracotomy (Open) or 3 port thoracoscopic surgery (TS) method. Mechanical staplers were used to develop incomplete fissures and to close the bronchus. Before chest closure, an air leak test was performed under a pressure loading of 25 cmH2O. As no leakage was detected, no coverage of the margin of the dissected or stapled lung tissue was performed, while small air leaks in other patients were managed by suturing. When alveolar air leakage occurred from the superficial pulmonary parenchyma, it was managed with fibrin glue in combination with an absorbable mesh sheet [Neoveil absorbable polyglycolic acid (PGA) felt, Gunze, Osaka, Japan]. In cases with alveolar air leakage occurring from a location deep in the pulmonary parenchyma, subcutaneous fat pads about 2×2 cm in size were harvested from the thoracotomy and placed on the damaged lung tissue with fibrin glue in combination with 2 or 3 mattress sutures (8). At the end of the operation, 1 chest tube, size 24 F (BLAKE® Silicone Drains, Ethicon, Inc., Somerville, NJ, USA), was placed, then suction of 10 cmH2O was applied by use of the Thopaz device. In each case, the drain was inserted through an insertion point on the 7th intercostal middle axillary line. For patients with lower lobectomy, the drain was basically inserted into the dorsal region and ascended to the apical portion of the lung and descended into the ventral region. For patients with upper or lobectomy, the drain was inserted into the ventral region and ascended to the apical portion of the lung and descended into the dorsal region. In this period, we performed reoperation to control an air leak when the amount of leakage was more than 1,000 mL/min immediately after surgery.
Postoperative management
The tube was removed when air flow was less than a continuous 20 mL/minute within the past 24 hours after confirming complete re-expansion of the residual lung (9). If the air leak persisted until postoperative day 7 and the residual lung was fully expanded, chemical pleurodesis with 5 KE of OK-432 (Pecibanil®: Chugai Pharmaceutical Co. Ltd., Tokyo, Japan) or supplementation with factor XIII (Fibrogammin®: CSL Behring, Tokyo, Japan) were considered. If a significant air leak at more than 500 mL/minute with increased subcutaneous emphysema or residual air spaces persists in a patient despite conservative measures, surgical revision was considered. For patients with prolonged air leak, these postoperative chest tube management procedures were agreed upon and used by all 5 members of our department.
Data collection
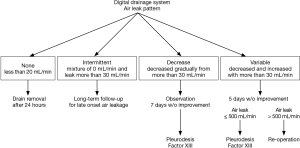
Air flow data were transferred to a PC by USB and analyzed. As shown in Figure 1, we divided the postoperative air leak patterns into 4 groups, as follows: none, air leakage ≤20 mL/minute; intermittent, air leakage varied between 0 and >20 mL/minute; decreased, air leakage at >20 mL/minute then gradually decreased; and variable, air leakage showed variable decrease and increase >20 mL/minute and not ≤20 mL/minute within 4 days after surgery. In this study, prolonged air leak was defined as an air leak lasting for more than 5 days (4). Variables were compared among the groups using a Chi-square test and Krusukal-Wallis test with JMP Pro (version 12.2.0).

Results
In the present patients who underwent a pulmonary resection, the incidence of prolonged air leak was 10% (30/299). The postoperative air leak pattern was none in 217 (73%), intermittent in 21 (7%), decrease in 40 (13%), and variable in 21 (7%). Patient characteristics after dividing into those groups are shown in Table 1. Age, preoperative respiratory function, and operation procedures were similar among them. Male patients showed to be classified more often into the decrease or variable group. Furthermore, operation time was significantly longer in patients of variable group. There was no correlation of air leak pattern with histology type or staging of lung cancer. The incidence of prolonged air leak in each group was 0.5% (1/217) in the none group, 24% (5/21) in the intermittent group, 20% (8/40) in the decrease group, and 76% (16/21) in the variable group.

Full table
Figure 2 shows the differences in terms of air leakage immediately after surgery in the operating room, air leak duration, and chest tube duration among the 4 groups. The amount of leakage immediately after surgery was highest in the variable group, while those classified as intermittent or variable group showed longer durations of prolonged air leakage and chest tube placement.

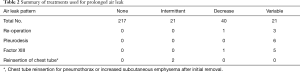
A summary of methods for treatment of postoperative air leakage in the present patients is shown in Table 2. Those with a prolonged leak were treated by reoperation, chemical pleurodesis, and factor XIII supplementation. The frequency of postoperative treatment was greater in the variable group as compared to the others. In addition, we found that procedures for reinsertion of the chest tube for pneumothorax or increased subcutaneous emphysema after chest tube removal were confined to the intermittent group. No other major pulmonary complications were noted and no postoperative mortalities occurred in the present cohort. Late onset (>30 days) alveolopleural fistula was seen in 1 patient in the none and 2 in the intermittent group, each of whom underwent reinsertion of the chest tube or a reoperation to provide drainage.
Full table
Discussion
The duration of chest drainage following a pulmonary resection procedure is mainly dependent on the presence of air leakage and/or pleural effusion (1). Several risk factor of prolonged air leak have been identified, including age, gender, body mass index, presence of pleural adhesions, lobectomy or segmentectomy, and surgical sites (4,10,11). Patients with prolonged air leak have higher incidence of postoperative complications, stayed longer in the hospital after surgery, and pay higher medical costs (3,4). Thus, an air leak that continues for more than 5 days should be treated. To develop a treatment strategy for patients with postoperative air leakage, we reviewed various air leak patterns in patients who underwent a pulmonary resection procedure for lung cancer with use of a digital pleural drainage system. Patients in the variable group had a greater amount of air leakage immediately after surgery, and the durations of air leak and chest drainage tube placement were longer as compared to the none and decrease group. Those patients often required invasive treatment, such as surgery or pleurodesis, for prolonged air leakage. If a significant air leak with increased subcutaneous emphysema or residual air spaces, reoperation should be considered. In order to minimize the risk of pleural space infection or partial obstruction, this decision should be made as early as possible within a few days (12). In the variable air leak pattern group, interventional treatment was typically performed approximately 5 days after the initial operation. Thus, when a variable air leak pattern continues, chemical pleurodesis or surgical repair should be considered, and performed within 5 days after surgery when considered necessary. Our findings also revealed that patients with air leakage greater than 500 mL/minute immediately after surgery developed a prolonged air leak and were classified as part of the variable group. Thus, those patients may require treatment for air leakage during the early postoperative period.
Although the mean amount of air leakage in the intermittent group was not extremely elevated, the durations of air leak and chest drainage tube were longer as compared to the none and decreased groups, while some also underwent invasive treatment for prolonged air leakage. Two patients in the intermittent group underwent reinsertion of the chest tube for pneumothorax or increased subcutaneous emphysema after chest tube removal. Furthermore, another 2 in that group suffered from late onset air leakage and were readmitted for drainage or a reoperation. Such patients should be carefully followed for several months after surgery. Notably, our findings showed that the intermittent air leak pattern was not easily detected with a conventional drainage system, but rather with use of the Thopaz digital drainage system which can provide objective data in real time as well as a 24-hour graph of air flow.
On the other hand, air leakage showed a gradual decrease and was diminished within several days in the decrease group and the postoperative course of those patients was largely uneventful. Some underwent interventional treatment such as pleurodesis and factor XIII supplementation, which immediately reduced the air leak. A lower postoperative level of factor XIII activity is one of the causes of an air leak, with exogenous factor XIII concentrate shown to be an effective and safe non-invasive treatment (13). In our experience, supplementation with factor XIII is effective for a minor air leak that appears after surgery, thus we consider it to be suitable for patients categorized as decrease in our classification. We also think that these patients do not always require surgical repair. Our present results indicate that air leakage rate measured after a lung resection can show the air leak pattern, which is useful for predicting the durations of air leakage and chest tube drainage, as well as the postoperative course.
The mechanism of prolonged air leakage remains unclear. In the present classification, the decrease pattern likely indicates a normal healing process of lung parenchyma defects and residual lung expansion, while the variable pattern indicates active and massive air leakage due to the presence of several lung parenchyma defects. Furthermore, the intermittent pattern is likely associated with drainage failure due to the position of the drain tube. The location of the chest tube depends on what is being drained. We usually use the Blake drain for chest drainage of air as well as pleural fluid after pulmonary resection instead of using two drains. Although the postoperative course was uneventful for almost patients, drainage is not adequate for a few patients probably due to the position of the Blake drain tube. Such failure after a pulmonary resection procedure may result in inadequate air space and pleural effusion, thus preventing lung expansion and wound healing. Thus, these factors may be related to late onset air leakage in patients with the intermittent classification.
Digital pleural drainage systems have been reported to help reduce the durations of chest tube drainage and hospitalization as compared with conventional systems (14), which is likely related to the more accurate pressure regulation in the pleural cavity provided by the technological advantages of these systems (6,15). Another reason is that the present patients who underwent digital drainage evaluation experienced chest drain removal 1 day earlier as compared to those treated with a traditional system, because a chest tube clamping test was not necessary. Such clamping is often needed for patients with a traditional system to rule out the presence of small air leaks that are difficult to detect (5,16). In our cohort, chest tubes were removed when the amount of continuous air leakage was less than 20 mL/minute. None of our patients, excluding the intermittent group, suffered from pneumothorax after chest drain removal, indicating that the air leak quantification performed with a digital drainage system shows an accurate trend of air leakage based on recordings obtained over several hours, thus enabling effective decision making in regard to drain removal (7). Furthermore, use of a digital device makes possible earlier patient mobilization as well as improved postoperative physiotherapy results, reducing the risk of secretion retention and pneumonia (1).
Our study has some limitations. The occurrence of air leakage is dependent on the operation procedures employed. Therefore, the ability to predict air leak duration is important for considering treatment for a prolonged air leak after operative findings are known, such as results of an intraoperative water seal test and the repair method used for lung parenchyma defect.
Conclusions
We found that air leak pattern following a pulmonary resection can predict the durations of air leakage and chest tube drainage, which is helpful for producing an air leak management algorithm (Figure 3). In addition, our results suggest potential advantages of a digital drainage system, including continuous monitoring and recording capabilities, which can provide information to determine the air leak pattern in patients undergoing a pulmonary resection procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of Osaka University Hospital (ID10026-3) and written informed consent was obtained from all patients.
References
- Filosso PL, Nigra VA, Lanza G, et al. Digital versus traditional air leak evaluation after elective pulmonary resection: a prospective and comparative mono-institutional study. J Thorac Dis 2015;7:1719-24. [PubMed]
- Burt BM, Shrager JB. Prevention and management of postoperative air leaks. Ann Cardiothorac Surg 2014;3:216-8. [PubMed]
- Brunelli A, Cassivi SD, Halgren L. Risk factors for prolonged air leak after pulmonary resection. Thorac Surg Clin 2010;20:359-64. [Crossref] [PubMed]
- Zhao K, Mei J, Xia C, et al. Prolonged air leak after video-assisted thoracic surgery lung cancer resection: risk factors and its effect on postoperative clinical recovery. J Thorac Dis 2017;9:1219-25. [Crossref] [PubMed]
- Anegg U, Rychlik R, Smolle-Juttner F. Do the benefits of shorter hospital stay associated with the use of fleece-bound sealing outweigh the cost of the materials? Interact Cardiovasc Thorac Surg 2008;7:292-6; discussion 26. [Crossref] [PubMed]
- Gilbert S, McGuire AL, Maghera S, et al. Randomized trial of digital versus analog pleural drainage in patients with or without a pulmonary air leak after lung resection. J Thorac Cardiovasc Surg 2015;150:1243-9. [Crossref] [PubMed]
- Rathinam S, Bradley A, Cantlin T, et al. Thopaz Portable Suction Systems in Thoracic Surgery: an end user assessment and feedback in a tertiary unit. J Cardiothorac Surg 2011;6:59. [Crossref] [PubMed]
- Shintani Y, Inoue M, Funaki S, et al. Clinical usefulness of free subcutaneous fat pad for reduction of intraoperative air leakage during thoracoscopic pulmonary resection in lung cancer cases. Surg Endosc 2015;29:2910-3. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. The benefits of continuous and digital air leak assessment after elective pulmonary resection: a prospective study. Ann Thorac Surg 2008;86:396-401. [Crossref] [PubMed]
- Okereke I, Murthy SC, Alster JM, et al. Characterization and importance of air leak after lobectomy. Ann Thorac Surg 2005;79:1167-73. [Crossref] [PubMed]
- Rivera C, Bernard A, Falcoz PE, et al. Characterization and prediction of prolonged air leak after pulmonary resection: a nationwide study setting up the index of prolonged air leak. Ann Thorac Surg 2011;92:1062-8; discussion 8. [Crossref] [PubMed]
- Mueller MR, Marzluf BA. The anticipation and management of air leaks and residual spaces post lung resection. J Thorac Dis 2014;6:271-84. [PubMed]
- Inoue H, Nishiyama N, Mizuguchi S, et al. Clinical value of exogenous factor XIII for prolonged air leak following pulmonary lobectomy: a case control study. BMC Surg 2014;14:109. [Crossref] [PubMed]
- Pompili C, Detterbeck F, Papagiannopoulos K, et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg 2014;98:490-6; discussion 6-7. [Crossref] [PubMed]
- Miller DL, Helms GA, Mayfield WR. Digital Drainage System Reduces Hospitalization After Video-Assisted Thoracoscopic Surgery Lung Resection. Ann Thorac Surg 2016;102:955-61. [Crossref] [PubMed]
- Varela G, Jimenez MF, Novoa NM, et al. Postoperative chest tube management: measuring air leak using an electronic device decreases variability in the clinical practice. Eur J Cardiothorac Surg 2009;35:28-31. [Crossref] [PubMed]


