Using twitch tracheal airway pressure, negative inhale forced pressure, and Medical Research Council score to guide weaning from mechanical ventilation
Introduction
Mechanical ventilation (MV) in critically ill patients is associated with increased mortality (1) and medical cost (2). Both issues exacerbate as MV is prolonged, especially due to ventilator-associated pneumonia and ventilator-induced diaphragm dysfunction (3). Thus, predicting the success of weaning from MV is an important and universal issue in critically ill patients.
Diaphragmatic dysfunction leads to a higher rate of weaning failure and prolonged MV time (4). Negative inspiratory force (NIF) is widely used clinically for the noninvasive and rapid assessment of the strength of the entire inspiratory muscle, including the diaphragm (5). However, NIF is easily influenced by subjective factors such as the patient’s perception and cooperation. At present, peripheral muscle strength is mostly evaluated using the Medical Research Council (MRC) scale (6-8).
In 1985, the assessment of diaphragmatic function was often based on twitch transdiaphragmatic pressure (TwPdi) obtained by phrenic nerve stimulation. Similowski et al. (9) proposed utilizing cervical magnetic stimulation to obtain the TwPdi and evaluate diaphragmatic contractility without pain or adverse effects. In 2001, Mills et al. (10) showed that twitch tracheal tube pressure during magnetic stimulation of the phrenic nerves could be used as an indicator of diaphragm strength in the intensive care unit (ICU).
Our previous study (11) showed that twitch tracheal airway pressure (TwPtr) and TwPdi correlated well, but TwPtr can better assess diaphragm function. Especially with the self-designed T-type solenoid unidirectional connection, diaphragm function could be evaluated non-invasively. We hypothesized that TwPtr was a better predictor for weaning compared to NIF and MRC score.
The present prospective study evaluated TwPtr relative to NIF or MRC score, for predicting success of weaning from MV.
Methods
According to our pilot study for a preliminary experiment (unpublished), the sensitivity was 0.889 (P1), the specificity was 1 (P2), the allowable error (δ) was 0.1, and the inspection level (α) was 0.05; µ0.05 was 1.96 (2-sided test). According to the formula n1 = (µα/ δ)2 × P1 (1−P1) and n2 = (µα/ δ)2 × P2 (1−P2) (12), the sample size should be 38.
All the patients, or their guardians, were aware of the purpose of this study and provided signed informed consent. The Scientific Research Project Review Ethics Committee of Guangzhou Medical University First Affiliated Hospital approved this prospective study (Ethics Batch Number 2017 No. 35).
The enrolled patients were admitted to the ICU of First Affiliated Hospital of Guangzhou Medical University from December 2015 to March 2017, received invasive MV lasting >48 hours, and were entering the spontaneous breathing trial (SBT) stage. The patients were aged >18 years, with stable vital signs and respiratory rate <30 breathes/min. The general demographic and clinical information collected for each patient included name, age, gender, date of admission, date into ICU, diagnosis, weaning time, and Acute Physiology and Chronic Health Evaluation (APACHE II) score.
Patients with any of the following were excluded from this study: thoracic drainage; abdominal hypertension; abdominal infection; pregnancy; in a severe delirium state; with uncontrolled epilepsy; or could not cooperate with the examination. In addition, patients with the following features that contraindicated magnetic stimulation were excluded: heart Pacemaker; implantable cardiac defibrillator; cervical spine injury; or cervical implant device (3).
Patients were considered for weaning under the following conditions: the cause of respiratory failure was relieved or controlled; patient was conscious without sedation or analgesic maintenance; hemoglobin ≥8 mg/L; ventilator pressure support ≤8 cmH2O; positive end-expiratory pressure (PEEP) ≤5 cmH2O; P/F ratio ≥200 mmHg; pH ≥7.25; and fraction of inspired oxygen (FiO2) ≤40%. Weaning failure was defined as the need to re-intubate for invasive ventilation within 48 hours after extubation. Weaning success was defined as no need to re-intubate within 48 hours after extubation.
MRC score and NIF acquirements
The UK MRC 6-level scale (6-8) was used to score peripheral muscle strength, from 0 to 5, with 5 being the strongest. A total score <48 points satisfies the criteria for an initial diagnosis of ICU-acquired weakness (13).
NIF ≤−20 cmH2O is widely accepted as a prognosticator of weaning success. Most types of ventilators are equipped to measure this feature. With the SBT program in the pressure support mode (pressure support ventilation ≤8 cmH2O, PEEP =4–5 cmH2O), patients with smooth breathing and stable vital signs were placed in the half-seat position (a 45° angle between the spine and horizontal). With inspiratory strength maximized and the fastest inhalation, NIF was recorded. Measurements were taken for 5 minutes, and 3 records were acquired. The maximum value was taken.
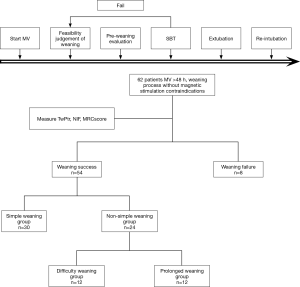
Weaning progressed as in the Figure 1 flowchart. Weaning success was classified as simple, difficult, or prolonged, defined as follows (14). Patients who accomplished simple weaning proceeded from initiation of weaning to successful extubation on the first attempt without difficulty. Difficult weaning was considered the failure of initial weaning, with ≤3 SBTs required or ≤7 days from the first SBT to achieve successful weaning. Prolonged weaning was defined as failure at ≤3 weaning attempts or requiring >7 days of weaning after the first SBT. For purposes of comparison, the patients who experienced difficult or prolonged weaning were considered the non-simple weaning group.
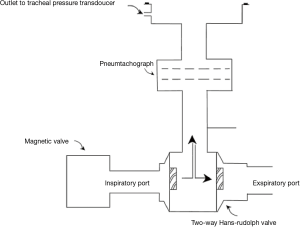
The measurement of TwPtr was performed with a 2-way non-rebreathing automatic trigger device system (Figure 2), with the ventilator connected to the pipeline. Before the magnetic stimulation, the patients were fasted and were observed for gastric juice retention. Parallel suction was utilized to maintain airway patency. Patients were positioned half-sitting (with spine at 45° from horizontal) and the waist belt was loosened to release abdominal pressure.
The TwPtr measurements are shown in Figure 3. At the end of the inspiratory phase, the magnetic valve at the inspiratory terminal was closed (Figure 3, point a). Inspired air was blown out of the system from the unidirectional valve. At this moment, a negative inspiratory pressure was created, which was detected by the pressure sensor (−0.005 cmH2O). A trigger given by the magnetic stimulator synchronization was released to stimulate the phrenic nerve of the body surface projection (Figure 3, point b). The diaphragm constricted, which caused the pressure in the system to change (Figure 3, point c). TwPtr was calculated as the difference in the pressures at points c and b.
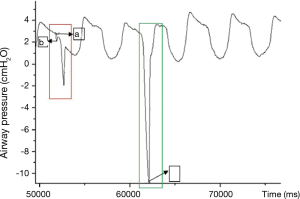
Before magnetic stimulation, a blank control was used to determine the starting point of the magnetic stimulus and the value of the intrapulmonary airway pressure by the patients themselves (shown as a red frame box in Figure 3).
Statistical analysis
Data was identified as with or without normal distribution. All normally distributed data were expressed as mean ± standard deviation (SD). The Mann-Whitney test was used for ranked variables. If normal distribution and variance homogeneity were satisfied, variance analysis was used. If the normal distribution and variance homogeneity were not satisfied, the Kruskal-Wallis H test was used. A multifactor logistic regression model was used to analyze and correct the effects of confounding factors on weaning, and the area under the receiver operating characteristic (ROC) curve (AUC) was calculated. The difference between AUCs was calculated using the methodology of Hanley and McNeil (15). P<0.05 was defined as statistically significant. The SPSS 19.0 software package was used for statistical analyses.
Results
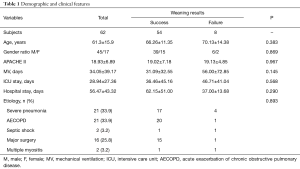
Sixty-two patients (45 men and 17 women, aged 61.3±15.9 years old) were included in the present study (Table 1). The overall mean APACHE II score was 19. All the patients were able to complete the entire experiment and no discomfort or other side effects were observed.
Full table
There were no significant differences at baseline between the successful weaning and failed weaning groups with regard to the following: age; gender; MV time; ICU stay; hospital stay, and MV etiology (Table 1).
The optimal thresholds obtained via ROC curve analysis for weaning success were: TwPtr, −8.75 cmH2O; NIF, −20 cmH2O; and MRC score, 48 (Table 2). The ROC analysis indicated differences in the sensitivity, specificity, and AUC of these parameters. By the AUCs, the MRC score was significantly less able to determine the success rate of weaning than TwPtr combined with NIF.
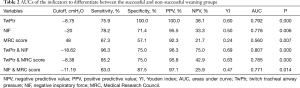
Full table
Compared with the non-simple weaning group (that is, including difficult and prolonged weaning), the patients in the simple weaning group were significantly younger, with a lower APACHE II score, and the durations of MV, and ICU and hospital stay were shorter (Table 3). The simple and non-simple groups were similar in etiology. The multivariate logistic regression analysis showed that age was an independent risk factor (P=0.002) to predict weaning failure. In the weaning success group, after correction for age, the cutoff points to differentiate the simple weaning from non-simple weaning groups were determined by AUCs for the various indicators (Table 4).
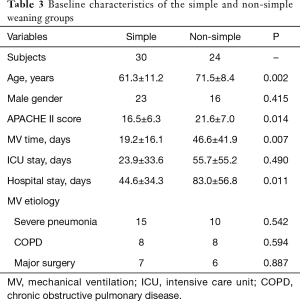
Full table
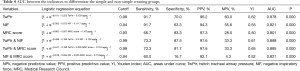
Full table
The MRC score of the simple weaning group was significantly higher than that of the failed weaning group (Table 5). The TwPtr of the simple weaning group was significantly higher than that of the non-simple weaning groups. The NIF of the simple weaning group was significantly higher than that of the prolonged and failed weaning groups.
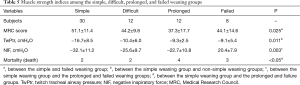
Full table
Discussion
This prospective study determined the relative values of TwPtr, NIF, and MRC score for predicting success of weaning patients of MV. Primarily, we found that the mean age of patients in the non-simple weaning group was significantly higher than that of the simple weaning group. Furthermore, TwPtr was superior to either NIF or MRC score for differentiating patients in the simple weaning group from those patients who experienced difficult, prolonged, or failed weaning. Finally, combining TwPtr and NIF was better for predicting weaning success than the MRC score alone.
As life expectancies in China have increased, the average age of patients admitted to the ICU has become higher. Our study showed that the mean age of patients who experienced non-simple weaning was significantly higher than that of patients who accomplished simple weaning. This is in accordance with a recent prospective 1-day prevalence study performed at 55 ICUs in Mainland China (16), in which the study population comprised 302 adult patients receiving invasive MV. The study determined that being older than 74 years (odds ratio 2.78; 95% CI: 1.05–7.40) was a high-risk factor for weaning failure. These findings suggest that weaning should be considered with great caution in elderly patients.
Diaphragm dysfunction is associated with higher ICU and hospital mortality, and is a major determining factor in weaning failure (17). Using an automatic trigger system to monitor TwPtr is helpful for evaluating diaphragm function; readings of TwPtr are highly reproducible and effective (18). Our present study also showed that TwPtr was useful for differentiating patients who could accomplish simple weaning from those in the non-simple weaning group. Similarly, Dres et al. (19) showed that in ICU patients, low twitch pressure was independently associated with weaning failure, the MRC score was not, and the mortality rate of patients who required extended weaning was higher than that of the simple weaning group. It has also been shown that the TwPtr of patients in the ICU who survive (−7.3 cmH2O) was significantly lower than that of non-survivors (−9.7) (16). Esteban et al. (1) showed that the rate of mortality was positively associated with MV time, even in patients who experienced successful evacuation.
NIF is putatively not as accurate as TwPdi in predicting weaning outcome, because NIF requires subjective coordination and is also affected by lung volume status (20). In the present study, we set the NIF to −20 cmH2O as the threshold for extubation, with a lower specificity (71.4%) and a higher sensitivity (78.2%), which is similar to previous studies (21). NIF measurements are volitional tests that require patient’s cooperation and are affected by lung capacity status (22). These measurements may be difficult in the ICU, where respiratory muscle strength may be underestimated because of the effects of sedation. Therefore, an NIF of less than −20 cmH2O may be considered to include a certain amount of respiratory muscle reserve, while an NIF greater than −20 cmH2O should be combined with other parameters to predict weaning outcome.
Limb weakness is also prevalent in the ICU (morbidity 34%) in patients with long-term disease (23,24). The MRC score mainly reflects peripheral muscle strength. An MRC score <48 points satisfies the criteria for an initial diagnosis of ICU-acquired weakness (13).
Although the diaphragm and peripheral muscles are of the same skeletal muscle and have the same cell access, the damages that result from MV or bed rest are very different. Indeed, the MRC score found in our study had low specificity (57.1%) and sensitivity (67.3%), which suggests that it was not an indicator of extubation success.
The utilization of non-invasive ventilation is a component of modern weaning strategies that has less weaning failure and an improved outcome. This is especially true for patients who are likely to experience difficult weaning. The present study included a high number of patients with infections, in which weaning was considered only after stabilization and improvement of the underlying disease.
The present study is limited in that using phrenic nerve stimulation to measure diaphragm function may be contraindicated, and there is no gold standard for determining diaphragm dysfunction. We also cannot absolutely rule out that incomplete (or overstimulation) of phrenic nerve fibers may have contributed to low (or high) twitch pressure in some cases, since no references regarding range are available. We did not conduct a follow-up study of mortality. A multi-center study is needed.
Conclusions
In summary, for patients on MV in the ICU entering the SBT stage, TwPtr had higher sensitivity and specificity than did the NIF or MRC score for differentiating patients who underwent simple and non-simple weaning. TwPtr combined with NIF or other combinations could be used to predict weaning success better than MRC score alone. A further comprehensive assessment will require a larger sample size and evaluations of muscle endurance and other indicators.
Acknowledgements
Funding: This research was supported by National Natural Science Foundation of China (81490534).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Scientific Research Project Review Ethics Committee of Guangzhou Medical University First Affiliated Hospital (ethics batch number 2017 No. 35) and written informed consent was obtained from all patients.
References
- Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002;287:345-55. [Crossref] [PubMed]
- Cooper LM, Linde-Zwirble WT. Medicare intensive care unit use: analysis of incidence, cost, and payment. Crit Care Med 2004;32:2247-53. [Crossref] [PubMed]
- Grosu HB, Lee YI, Lee J, et al. Diaphragm muscle thinning in patients who are mechanically ventilated. Chest 2012;142:1455-60. [Crossref] [PubMed]
- Kim WY, Suh HJ, Hong SB, et al. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 2011;39:2627-30. [Crossref] [PubMed]
- Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445-50. [Crossref] [PubMed]
- Fan E, Cheek F, Chlan L, et al. An official American Thoracic Society Clinical Practice guideline: the diagnosis of intensive care unit acquired weakness in adults. Am J Respir Crit Care Med 2014;190:1437-46. [Crossref] [PubMed]
- De Jonghe B, Sharshar T, Lefaucheur JP, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 2002;288:2859-67. [Crossref] [PubMed]
- Kleyweg RP, van der Meché FG, Schmitz PI. Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle Nerve 1991;14:1103-9. [Crossref] [PubMed]
- Similowski T, Fleury B, Launois S, et al. Cervical magnetic stimulation: a new painless method for bilateral phrenic nerve stimulation in conscious humans. J Appl Physiol 1989;67:1311-8. [Crossref] [PubMed]
- Mills GH, Ponte J, Hamnegard CH, et al. Tracheal tube pressure change during magnetic stimulation of the phrenic nerves as an indicator of diaphragm strength on the intensive care unit. Br J Anaesth 2001;87:876-84. [Crossref] [PubMed]
- Huang YQ. Clinical epidemiology. Beijing: People’s Health Press, 2002:98-119.
- Hua DM, Lin ZM, Ou YE, et al. Use of a two-way non-rebreathing valve to simplify the measurement of twitch mouth pressure using an inspiratory pressure trigger and the establishment of an optimal trigger threshold for healthy subjects and COPD patients. Respir Physiol Neurobiol 2014;201:47-54. [Crossref] [PubMed]
- Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med 2014;370:1626-35. [Crossref] [PubMed]
- Boles JM, Bion J, Connors A, et al. Weaning from mechanical ventilation. Eur Respir J 2007;29:1033-56. [Crossref] [PubMed]
- Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 1983;148:839-43. [Crossref] [PubMed]
- Li J, Zhan QY, Wang C. Survey of Prolonged Mechanical Ventilation in Intensive Care Units in Mainland China. Respir Care 2016;61:1224-31. [Crossref] [PubMed]
- Supinski GS, Callahan LA. Diaphragm weakness in mechanically ventilated critically ill patients. Crit Care 2013;17:R120. [Crossref] [PubMed]
- Demoule A, Jung B, Prodanovic H, et al. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact-a prospective study. Am J Respir Crit Care Med 2013;188:213-9. [Crossref] [PubMed]
- Dres M, Dube BP, Mayaux J, et al. Coexistence and Impact of Limb Muscle and Diaphragm Weakness at Time of Liberation from Mechanical Ventilation in Medical Intensive Care Unit Patients. Am J Respir Crit Care Med 2017;195:57-66. [Crossref] [PubMed]
- Nemer SN, Barbas CS, Caldeira JB, et al. Evaluation of maximal inspiratory pressure, tracheal airway occlusion pressure, and its ratio in the weaning outcome. J Crit Care 2009;24:441-6. [Crossref] [PubMed]
- Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445-50. [Crossref] [PubMed]
- Fiz J, Gallego M, Izquierdo J, et al. Variation in maximum inspiratory and expiratory pressure after application of inspiratory loads in patients with COPD. Chest 1990;97:618-20. [Crossref] [PubMed]
- Sharshar T, Bastuji-Garin S, Stevens RD, et al. Presence and severity of intensive care unitacquired paresis at time of awakening are associated with increased intensive care unit and hospital mortality. Crit Care Med 2009;37:3047-53. [Crossref] [PubMed]
- Schmidt GA, Girard TD, Kress JP, et al. Official Executive Summary of an American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically ill Adults. Am J Respir Crit Care Med 2017;195:115-9. [Crossref] [PubMed]