Authors’ reply—multi-organ ultrasonography: a stethoscope for the body
We read with great interest the letter from Sakka et al. (1) commenting our article (2) on comprehensive haemodynamic monitoring in patients with acute respiratory distress syndrome (ARDS) and traumatic brain injury (TBI). We agree with the authors that haemodynamic monitoring has to be implemented in patients with ARDS complicating TBI. However, we must be aware that thermo-dilution methods are influenced by major pitfalls and limitations that can be summarized as follows: (I) their predictive cutoff values are highly variable; (II) they require controlled mechanical ventilation with tidal volumes >8 mL/kg predicted body weight without inspiratory efforts; (III) their reliability may be influenced by any coexisting right heart dysfunction.
In a context where non-invasive monitoring techniques are expanding, the use of bedside multi-organ ultrasonology could represent a step forward in the management of ARDS complicating TBI.
We therefore suggest to implement the use of ultrasound based non-invasive techniques of multimodal monitoring, such as transthoracic echocardiogram, lung ultrasound and trans cranial Doppler as well as the assessment of organ perfusion with renal Doppler resistive index (RDRI) and splenic Doppler resistive index (SDRI) in patients with TBI and severe lung injury (3).
The goal of multimodal brain monitoring is the early detection of secondary brain injury by monitoring changes in physiologic parameters that reflect cell death and injury. These parameters include intracranial pressure, cerebral perfusion pressure, cerebral blood flow, brain tissue oxygenation, cerebral metabolism and electro cortical activity. The information can be obtained from these tools and, when integrated in the clinical practice, could help decision-making and early goal-directed therapy and to prevent secondary brain injury. Transcranial Doppler (TCD) can provide information on mean flow velocities of the main cerebral vessels, namely, middle cerebral artery, anterior cerebral artery, posterior cerebral artery. The mean flow velocity of middle cerebral artery former can be used for the detection of vasospasm and delayed cerebral ischemia in patients with subarachnoid haemorrhage, and trans Doppler pressure, can be indicative of regional cerebral ischemia (4). Indirect estimate of cerebral blood flow can be obtained non-invasively from mean flow velocities in different intra cerebral vessels (3). A comprehensive multi-organ ultrasound assessment (including heart, inferior cava vein, lung, kidneys and spleen) allows evaluating clinical signs of peripheral perfusion and congestion, and may be a guide for early-stage interventions.
Left ventricular outflow tract Doppler flow sampling allows tracking of stroke volume and cardiac output changes. Variations upon passive leg-raising maneuver or fluid challenge are strong predictors of fluid responsiveness, allowing careful fluid titration. Distension and small inspiratory variations of inferior vena cava suggest systemic venous congestion. Conversely, small size and large inspiratory variations suggest severe hypovolemia, whereas pronounced inspiratory size reduction predicts volume responsiveness with high specificity.
Echocardiography permits the evaluation of right ventricular function that may be heavily influenced by ventilator strategies, as suggested by strong negative correlations between right ventricular dysfunction and airway plateau pressure, or positive end-expiratory pressure, or PaCO2 levels, and positive correlation with prone position. For these reasons, a so-called ‘right ventricle protective ventilation approach’ has been recommended in order to identify the best ventilator settings (5).
Lung ultrasound can provide an early diagnostic tool to detect and differentiate ARDS from acute pulmonary edema, by showing B-lines with inhomogeneous and gravity-independent distribution, spared areas, pleural line thickening, and subpleural consolidations. Lung ultrasound can allow a quantification of extravascular lung water and the number of B-lines has shown an excellent correlation, both with the amount of extravascular lung water (EVLW), and the re-aeration scores in response to recruitment maneuvers (6) (Figure 1).
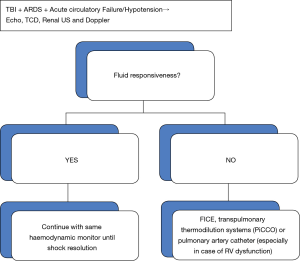
Moreover, readers must be aware that targeting fluid management based on stroke volume changes may not be useful for improving regional perfusion flow to organs, because splanchnic perfusion could increase in response to fluid administration even when stroke volume changes are considered insignificant. In these cases, fluid management should be set case by case according to TCD, RDRI and SDRI, avoiding positive fluid balance is an independent predictor of mortality in critically ill patients. Splanchnic Doppler resistive indexes have been suggested as a potential target to guide resuscitation. In particular, RDRI has been proposed as a marker of tissue oxygenation, because renal vasoconstrictor response has been demonstrated to be modulated not only by a reduction in effective circulating volume but also by mechanisms depending on effective tissue hypoxia as expressed by (mixed venous oxygen saturation) mixed-SvO2 even when arterial oxygenation is normal. RDRI correlates significantly with mixed-SvO2 and cardiac index, independent of the presence of other haemodynamic abnormalities, and is an expression of the adequacy of cardiac index (7).
Pairwise SDRI has been shown to be a marker of adequacy of resuscitation, because it correlates with arterial lactate clearance in selective subgroups of critically ill patients (8).
The precise role of combining ultrasound and transpulmonary thermodilution techniques in clinical practice, albeit currently suggested by guidelines, deserves further multidisciplinary research combining the knowledge, expertise and the common field of interest of intensive care physicians.
In conclusion, we acknowledge the input of the authors to highlight the need for a hemodynamic monitoring in patients with ARDS and TBI; we furthermore propose that conventional invasive methods based on the thermodilution should be always accompanied by a thorough Ultrasound multiorgan assessment, allowing a non-invasive safe and bedside clinical evaluation in the consideration of the US as “a stethoscope for the body”.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sakka SG, Tagami T, Kirov M, et al. Letter to: acute respiratory distress syndrome in traumatic brain injury: how do we manage it? J Thorac Dis 2018;10:E221-3. [Crossref] [PubMed]
- Della Torre V, Badenes R, Corradi F, et al. Acute respiratory distress syndrome in traumatic brain injury: how do we manage it? J Thorac Dis 2017;9:5368-81. [Crossref] [PubMed]
- Harary M, Dolmans RG, Gormley W. Intracranial Pressure Monitoring-Review and Avenues for Development. Sensors (Basel) 2018;18. [Crossref] [PubMed]
- Vora YY, Suarez-Almazor M, Steinke DE, et al. Role of transcranial Doppler monitoring in the diagnosis of cerebral vasospasm after subarachnoid haemorrhage. Neurosurgery 1999;44:1237-47; discussion 1247-8. [PubMed]
- Corradi F, Brusasco C, Pelosi P. Chest ultrasound in acute respiratory distress syndrome. Curr Opin Crit Care 2014;20:98-103. [Crossref] [PubMed]
- Corradi F, Brusasco C, Vezzani A, et al. Computer-Aided Quantitative Ultrasonography for Detection of Pulmonary Edema in Mechanically Ventilated Cardiac Surgery Patients. Chest 2016;150:640-51. [Crossref] [PubMed]
- Corradi F, Brusasco C, Paparo F, et al. Renal Doppler Resistive Index as a Marker of Oxygen Supply and Demand Mismatch in Postoperative Cardiac Surgery Patients. Biomed Res Int 2015;2015. [Crossref] [PubMed]
- Corradi F, Brusasco C, Garlaschi A, et al. Splenic Doppler resistive index for early detection of occult hemorrhagic shock after polytrauma in adult patients. Shock 2012;38:466-73. [Crossref] [PubMed]


