Pulmonary torsion after open esophagectomy for esophageal cancer: a case report and review
Introduction
Pulmonary torsion (PT) is an extremely uncommon event (1-4). Although PT is known to occur only rarely after lung resection, we now know that it can also occur after other thoracic procedures such as cardiac, esophageal, and chest trauma surgery and, spontaneously, after chest trauma itself (3-11). A delay in diagnosis and/or an improper treatment strategy can lead to serious complications (3,4,10-15). In this report, we describe a case of PT, discuss what we learned about methods of early diagnosis and appropriate treatment strategies from our experience, and review the literature.
Case presentation
A 77-year-old man with hypertension and a history of surgery for tongue cancer but no significant history of cardiovascular or pulmonary disease was diagnosed as having squamous cell carcinoma of the esophagus (cT1aN0M0-cStage IA, UICC classification 7th ed.). A thoracoscopic esophagectomy with three-field lymph node dissection was performed. A single-lumen endotracheal tube with a bronchial blocker was used for one-lung ventilation. During the operation, a bridging vein between the azygos vein and hemiazygos vein was damaged near the diaphragm, and conversion to open esophagectomy was required to control the bleeding, after which the tumor resection was finally completed. The anesthesiologist noted obstruction of the right upper lobe bronchus and stenosis of the bronchus intermedius by bronchoscopy, but after discussion with the surgeons, these were judged to be caused only by compression of the lungs (Figure 1).

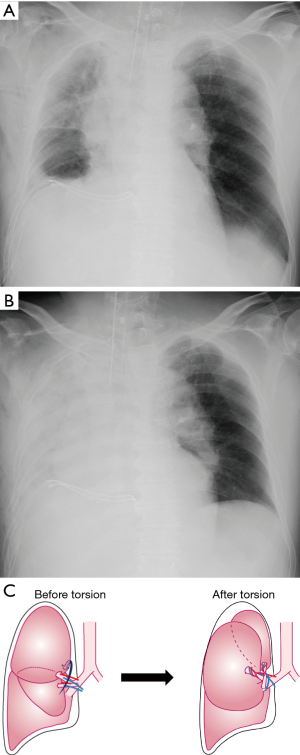
The initial portable chest x-ray film obtained just after the operation showed decreased clarity of the right upper and middle fields (Figure 2A), but arterial blood gases were normal with a partial arterial oxygen tension to fractional inspired oxygen ratio (PaO2/FIO2 ratio) of 400.
The patient was admitted to the surgical intensive care unit with stable vital signs. On the morning of the first postoperative day, the chest radiograph revealed complete opacification of the right hemithorax (Figure 2B). The PaO2/FIO2 ratio had dropped to less than 200. A blood test showed only a slight rise in inflammatory findings. A computed tomography (CT) scan of the chest revealed noticeably swollen right upper and middle lobes with diffuse consolidation, a tapered severe stenosis of the proximal right pulmonary artery, obliteration of the right upper bronchus and first branch of the right pulmonary artery, and narrowing of the right lower bronchus and basal pulmonary artery. We diagnosed right upper and middle lobar torsion. The patient underwent emergent rethoracotomy that night (about 16 hours after the open esophagectomy). Before starting surgery, the patient was placed on extracorporeal membrane oxygenation due to the deterioration of his respiratory status. When the chest was opened, the right upper and middle lobes were tense and dark red in color. These lobes were so swollen that we could not immediately grasp the details of how they were twisted. First, we divided the superior pulmonary vein in the pericardium to avoid the systemic release of toxic substances produced in the ischemic lung and thrombus in the superior pulmonary vein. Then, we relieved the torsion manually. The lobes were twisted by 180° in a counter-clockwise direction around the normal length of the bronchovascular pedicle (Figure 1, Figure 2C). An incomplete interlobar fissure was seen between the right upper lobe and middle lobe. Thus, we resected the right upper and middle lobes (Figure 1). Pathological examination revealed extensive hemorrhagic infarction of the affected lobes.
Postoperatively, the patient suffered pneumonia, acute respiratory distress syndrome, pneumothorax, cerebral infarction, empyema, deep vein thrombosis, and renal failure, but he ultimately recovered and was transferred to the ward three months after surgery.
Discussion
It is very important for thoracic surgeons to acquire profound knowledge about PT because it occurs abruptly and can lead to catastrophic complications if managed improperly. Once PT occurs in a high-risk patient, it is easy to imagine that the patient could enter a malignant cycle resulting in death.
We performed a literature search using PubMed and ICHUSHI, which offers information on medical studies in Japan for the past 110 years. The search terms were “pulmonary torsion OR lung torsion”. Of the 143 research papers and two abstracts (in proceedings) found from 1968 to 2017, 27 were rejected because they were insufficiently informative for us to allow the determination of individual patient data for various reasons. However, even though some of the research papers and abstracts did not have data for all items, we did not omit them from the analysis. The remaining 114 research papers, two abstracts, and our case were analyzed.
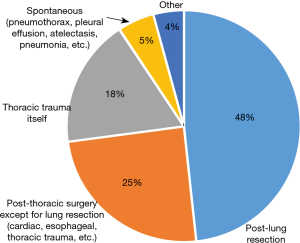
The etiology of PT is shown in Figure 3. Even after the consideration of publication bias (8,15), PT might occur in various situations, notably after other thoracic surgeries except for lung resection. The breakdown of the reasons for other thoracic surgery in 29 other cases (esophageal cancer in seven, other esophageal disease in six, thoracic trauma in six, congenital heart diseases in two, aortic dissection in two, mediastinal tumor in two, pneumothorax in two and lung transplantation in two patients) indicates that PT may occur in any thoracic surgery (3-11,17,18). It may be easily caused by operative procedures such as pushing on the collapsed lungs to improve the surgical view, transection of the inferior pulmonary ligament, and even more easily in conditions in which there are anatomical long pedicles or the absence of a parenchymal bridge between contiguous lobes (6,19,20). We think that the reason for the PT in our case was panic by the surgeons when the unexpected bleeding occurred, which resulted in them pushing on the collapsed lungs with great force. Anatomically, there is no long pedicle but incomplete lobulation between the right upper lobe and middle lobe.
Early diagnosis is very important because it strongly affects the subsequent surgical procedure and the postoperative course (3,4,10-15). In fact, however, it is often difficult to diagnose PT early. As shown in Table 1, only four patients underwent rethoracotomy immediately after surgery. We guess that one reason is that the vital signs and respiratory status in the early period of PT were usually stable, and the symptoms were usually minor and the abnormal laboratory data nonspecific (4,21-24). Another reason is that it takes some time for an obvious abnormality of the chest X-ray film to appear because air trapped in the twisted lobes can remain for a while (13,25-27). Actually, in many reported cases and our case, the timing of rethoracotomy was usually after the morning of postoperative day 1 at the earliest because further examinations to diagnose PT were triggered by progressive abnormalities seen on the chest X-ray films.

Full table
Now, what should be done to diagnose PT as early as possible to preserve and leave the affected lungs in good condition? We think that two cases give us the clues (23,28).
In one case, the patient underwent exploratory rethoracotomy before leaving the operating room (OR) because an abnormal airway pressure and abnormal bronchoscopic findings were pointed out during the operation. In the other case, the patient underwent exploratory rethoracotomy before leaving the OR because of an abnormal shadow on the portable chest X-ray film obtained at the end of surgery. In both cases, the patients experienced a good clinical course after detorsion. Furthermore, we experienced another patient with PT in whom an abnormality was found on the portable chest X-ray image just after surgery, and thoracoscopic detorsion was performed before extubation.
These cases teach us that there are several ways to discover PT in the OR. One is by carefully examining the portable chest X-ray film obtained just after surgery. Judging from the fact that some abnormality on the immediate post-operative chest X-ray film could be found in about 25% of the reported cases (Table 1), we are certain that abnormalities can be detected with higher probability if the image is examined with a suspicious eye. At present, although it is difficult to show the typical abnormalities that can be seen on portable chest X-ray films, from the report by Felson (29) and our own experience, an abnormal shadow adjacent to the hilum and in the paratracheal area of the lung field, or an abnormal vascular shadow in the residual lung, and/or mild decreased permeability of the lung field may be early findings of PT.
Second, intraoperative bronchoscopy is also a very useful tool when PT is suspected. Even if we cannot find complete torsional obstruction, any abnormality such as stenosis or mild torsion would be grounds enough for considering rethoracotomy (12-15,28).
Third, communication between the anesthesiologist and surgeons is also important. In one of 3 model cases in which detorsion was performed before the patient left the OR, the surgeon listened closely to the information about the bronchoscopic findings or changes in the respirator parameters provided by the anesthesiologist (28,30).
The treatment of PT basically comprises three types: resection of the twisted lobes, detorsion, and conservative management. Conservative treatment is effective only in cases in which the degree of torsion is mild, for example ≤90°, but it is rare and exceptional for a patient to recover with conservative treatment alone (18,31,32). In theory, the ideal treatment is detorsion, but in many of the reviewed papers, resection of the twisted lobes was selected because early diagnosis is very difficult, and the condition of the affected lobe was already poor at the time of rethoracotomy (Table 1). The merit of detorsion is that it preserves the functional lobes, which is very important in patients with severe comorbidities including decreased pulmonary function. However, there are some risks. One is the inflow of inflammatory mediators, necrotic tissue, and a pulmonary vein clot into the systemic circulation and respiratory tract following release of the torsion, which could potentially provoke a systemic inflammatory response resulting in multiorgan failure, cerebral infarction, and death (4,7,14,17,20,22). Another is that it can leave a shrunken and nonfunctional lung, which carries the risk of being a source of infections in over the long run (21,33-35). On the other hand, resection of the twisted lobes reduces the probability and severity of a systemic inflammatory response or cerebral infarction. As a result, it can also prevent other fatal complications that might occur subsequent to those events.
Theoretically, we should first consider detorsion, and if this is not possible, we should proceed with resection. However, in fact, it is not easy to judge the pathological condition of the twisted lobes by inspection and palpation during surgery, except in the case of obvious necrosis. In other words, it can be difficult to distinguish congestion from hemorrhagic infarction and early necrosis, which includes the destruction of the alveolar architecture, unless a wedge resection for biopsy is performed. Therefore, to minimize risk, resection of the twisted lung should be the first-line choice if it is unclear that the detorsion will go well.The main points of the operative procedure for PT are as follows. First, the pulmonary vein should be divided in the pericardium before the lobe is untwisted to avoid the inflow of inflammatory mediators, necrotic tissue, and a pulmonary vein clot into the left atrium (3,12,26,36-38). To perform this procedure safely and quickly, a large posterolateral thoracotomy is also required because the affected lobes can be intensely swollen. Second, to prevent a large amount of bloody secretions from flowing into the unaffected lobes after detorsion, we ask the anesthesiologist to use a double-lumen endotracheal tube and to aspirate the airway frequently (18,21,24,39-41). Third, we carefully check whether the remaining lobes are in their normal positions when the anesthesiologist re-inflates the collapsed lungs before chest closure. If we are still unsure, because of a complete pulmonary fissure and/or free long pedicle, fixation of the remaining lobes should be done.In summary, thoracic surgeons should realize that although infrequent, PT is one of the possible complications after any kind of thoracic surgery, and the outcomes are usually unsatisfactory. To diagnose PT early enough to preserve functional lobes, the postoperative portable chest X-ray film, intraoperative bronchoscopy, and close communication with the anesthesiologist are important. Resection of the twisted lobes should be selected if the surgeon is not sure that the twisted lobes are viable.
Acknowledgements
We thank all of the members of the Department of Thoracic Surgery, Surgery and Anesthesiology of Kitasato University School of Medicine for helping in the management of this patient.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: This case report was approved by the Kitasato University Medical Ethics Committee (B16-235).
References
- Cable DG, Deschamps C, Allen MS, et al. Lobar torsion after pulmonary resection: presentation and outcome. J Thorac Cardiovasc Surg 2001;122:1091-3. [Crossref] [PubMed]
- Demir A, Akin H, Olcmen A, et al. Lobar torsion after pulmonary resection; report of two cases. Ann Thorac Cardiovasc Surg 2006;12:63-5. [PubMed]
- Banki F, Velmahos GC. Partial pulmonary torsion after thoracotomy without pulmonary resection. J Trauma 2005;59:478-81. [Crossref] [PubMed]
- Larsson S, Lepore V, Dernevik L, et al. Torsion of a lung lobe: diagnosis and treatment. Thorac Cardiovasc Surg 1988;36:281-3. [Crossref] [PubMed]
- Ohde Y, Nakagawa K, Okumura T, et al. Spontaneous pulmonary torsion secondary to pseudo-Meigs' syndrome. Interact Cardiovasc Thorac Surg 2005;4:59-60. [PubMed]
- Alberti D, Borsellino A, Migliazza L, et al. Pulmonary torsion after cardiac surgery in two infants: review of pediatric literature. J Pediatr Surg 2004;39:1719-23. [Crossref] [PubMed]
- Oliveira C, Zamakhshary M, Abdallah MR, et al. Lung torsion after tracheoesophageal fistula repair: a case report and review of literature. J Pediatr Surg 2007;42:E5-9. [Crossref] [PubMed]
- Schamaun M. Postoperative pulmonary torsion: report of a case and survey of the literature including spontaneous and posttraumatic lesions. Thorac Cardiovasc Surg 1994;42:116-21. [Crossref] [PubMed]
- Schena S, Veeramachaneni NK, Bhalla S, et al. Partial lobar torsion secondary to traumatic hemothorax. J Thorac Cardiovasc Surg 2008;135:208-9. [Crossref] [PubMed]
- Chan MC, Scott JM, Mercer CD, et al. Intraoperative whole-lung torsion producing pulmonary venous infarction. Ann Thorac Surg 1994;57:1330-1. [Crossref] [PubMed]
- Felmine V, Zuleika M. Lobar torsion following thoraco-abdominal oesophagogastrectomy. Anaesthesia 2009;64:1130-3. [Crossref] [PubMed]
- Yamane M, Sano Y, Nagahiro I, et al. Lobar torsion after pulmonary resection for lung cancer. Kyobu Geka 2005;58:1153-7. [PubMed]
- Apostolakis E, Koletsis EN, Panagopoulos N, et al. Fatal stroke after completion pneumonectomy for torsion of left upper lobe following left lower lobectomy. J Cardiothorac Surg 2006;1:25. [Crossref] [PubMed]
- Pairolero PC, Linos DA. Complications associated with covering the bronchial stump with pleura. J Thorac Cardiovasc Surg 1980;79:453-5. [PubMed]
- Hendriks J, Van Schil P, De Backer W, et al. Massive cerebral infarction after completion pneumonectomy for pulmonary torsion. Thorax 1994;49:1274-5. [Crossref] [PubMed]
- Shiomi K, Yamashita K, Arai M, et al. The bronchoscopic findings and surgical technique of pulmonary torsion. Asvide 2018;5:596. Available online: http://www.asvide.com/article/view/25642
- Grazia TJ, Hodges TN, Cleveland JC Jr, et al. Lobar torsion complicating bilateral lung transplantation. J Heart Lung Transplant 2003;22:102-6. [Crossref] [PubMed]
- Gilkeson RC, Lange P, Kirby TJ. Lung torsion after lung transplantation: evaluation with helical CT. AJR Am J Roentgenol 2000;174:1341-3. [Crossref] [PubMed]
- Wagner RB, Nesbitt JC. Pulmonary torsion and gangrene. Chest Surg Clin North Am 1992;2:839-52.
- Haruki S, Nishikage T, Nakajima Y, et al. Torsion of right upper pulmonary lobe diagnosed after thoracoscopic esophagectomy: a case report. J Jpn Soc Endosc Surg 2009;14:693-7.
- Reyna R, Jung JY, Salas R, et al. Postoperative torsion of a lobe of the lung. Case report. Mo Med 1978;75:447-50. [PubMed]
- Oddi MA, Traugott RC, Will RJ, et al. Unrecognized intraoperative torsion of the lung. Surgery 1981;89:390-3. [PubMed]
- Shirakusa T, Motonaga R, Takada S, et al. Lung lobe torsion following lobectomy. Am Surg 1990;56:639-42. [PubMed]
- Kucich VA, Villareal JR, Schwartz DB. Left upper lobe torsion following lower lobe resection: Early recognition of a rare complication. Chest 1989;95:1146-7. [Crossref] [PubMed]
- Weisbrod GL. Left upper lobe torsion following left lingulectomy. Can Assoc Radiol J 1987;38:296-8. [PubMed]
- Eguchi T, Kato K, Shiina T, et al. Pulmonary torsion of the lingula following a segmentectomy of the left upper division. Gen Thorac Cardiovasc Surg 2008;56:505-8. [Crossref] [PubMed]
- Inagaki M, Fuziwara A, Yuasa H, et al. Case of torsion of the middle lobe after right upper lobectomy. J Jpn Soc Respir Endosc 1991;13:626-31.
- Ogasawara T, Nakai K, Hirota K, et al. Pulmonary torsion diagnosed and successfully treated during a surgery for esophageal cancer; a case report. J Jpn Soc Clin Anesth 2013;33:303.
- Felson B. Lung torsion: radiographic findings in nine cases. Radiology 1987;162:631-8. [Crossref] [PubMed]
- Goskowicz R, Harrell JH, Roth DM. Intraoperative diagnosis of torsion of the left lung after repair of a disruption of the descending thoracic aorta. Anesthesiology 1997;87:164-6. [Crossref] [PubMed]
- Hirata N, Monden Y, Iioka S, et al. Torsion of the right middle and lower lobes after right upper lobectomy: a case report. Nihon Kyobu Geka Gakkai Zasshi 1985;33:521-5. [PubMed]
- Takahashi E, Matsushima Y, Nakamura H. Pulmonary torsion following left upper lobectomy-recovery without thoracotomy; a case report. Jpn J Chest Surg 1993;7:103-8. [Crossref]
- Fu JJ, Chen CL, Wu JY. Lung torsion: survival of a patient whose hemorrhagic infarcted lung remained in situ after detorsion. J Thorac Cardiovasc Surg 1990;99:1112-4. [PubMed]
- Yang EM, Song ES. Lung torsion after tracheoesophageal fistula repair in an infant. Korean J Pediatr 2013;56:186-90. [Crossref] [PubMed]
- Koziarkiewicz M, Taczalska A, Piaseczna-Piotrowska A. Pulmonary torsion as an atypical complication of congenital esophageal atresia repair-a case report and review of literature. European J Pediatr Surg Rep 2014;2:43-45. [Crossref] [PubMed]
- Kanemitsu S, Tanaka K, Suzuki H, et al. Pulmonary torsion following right upper lobectomy. Ann Thorac Cardiovasc Surg 2006;12:417-9. [PubMed]
- Hasegawa S, Suda T, Kitamura Y, et al. A case of lobar torsion after left upper lung lobectomy. Jpn J Chest Surg 2008;22:829-32. [Crossref]
- Sakamoto K, Tamagawa S, Okita M, et al. Torsion of the middle lobe after right upper lobectomy of the lung; report of a case and the review of the Japanese literatures. Kyobu Geka 2003;56:251-4. [PubMed]
- Velmahos GC, Franhouse J, Ciccolo M. Pulmonary torsion of the right upper lobe after middle lobectomy for a stab wound to the chest. J Trauma 1998;44:920-2. [Crossref] [PubMed]
- Uchida Y, Ando S, Kida A, et al. Case of lung torsion after esophagectomy. Masui 2011;60:1321-5. [PubMed]
- Sakai M, Kurimori K, Saeki Y, et al. Video-assisted thoracoscopic conservative repair of postoperative lobar torsion. Ann Thorac Surg 2014;98:e119-21. [Crossref] [PubMed]