Combined approach using uniportal video-assisted thoracoscopic surgery in left tracheal sleeve pneumonectomy
Introduction
Left tracheal sleeve pneumonectomy is a rare and challenging surgical procedure with high postoperative complication and mortality rates due to limited access to the tracheal carina and mediastinal lymph node levels simultaneously (1,2). Here we report the least invasive single-stage surgical approach using uniportal video-assisted thoracoscopic surgery (VATS) currently successfully applied for a left centrally located bronchogenic carcinoma with tracheal involvement.
Case presentation
A healthy 82-year-old male was referred to a thoracic surgeon after two episodes of left lung acute pneumonia. Chest computed tomography (CT) scan and positron emission tomography-CT scan showed two tumors in the left lung: one in the proximal part of the left main bronchus extending into the lower part of the trachea and the second originating from the left lower lobe bronchus with extraluminal spread (Figure 1A,B) without any lymph node involvement or distant metastases. Bronchoscopy and pathological examination revealed squamous cell carcinomas in the left main bronchus infiltrating lateral wall of the tracheobronchial angle (Figure 1C) and in the orifice of left lower lobe segment VI bronchus. Left main bronchus patency was re-established with electrosurgical resection using a rigid bronchoscope. Lung-function tests demonstrated that the forced expiratory volume in 1 s was 2.27 liters (99.8%) and lung diffusion capacity for carbon monoxide was 82%.

The patient was intubated with a left-sided double lumen endotracheal tube and turned in the left decubitus position for right-sided posterolateral serratus-sparing thoracotomy in the fifth intercostal space. Surgical resection was initiated with mediastinal lymph node dissection of the subcarinal and right paratracheal level. Single-lung ventilation through cross-field intubation of the left main bronchus facilitated excellent exposure for U-shape pericardial release, resection of the two lower tracheal rings along with the right main bronchus transection, creation of anastomosis between the trachea and the right main bronchus using a continuous 3-0 polypropylene suture, and anastomosis reinforcement with a vascularized intercostal muscle flap (Figure 2A). The patient was turned in the right decubitus position and the operation continued on the left side. Subsequently, a 4.5-cm incision was made in the 5th intercostal space. Thirty-degree thoracoscope was inserted and left pulmonary veins and artery were divided by using an endoscopic vascular stapler. Left main bronchus with tumor-involved tracheal segment under the aortic arch was dissected free and the lung was extracted without rib spreading. Surgical resection was completed with multilevel mediastinal lymph node dissection and a chest tube was inserted through the thoracotomy incision (Figure 2B). Total operating time was 295 minutes.
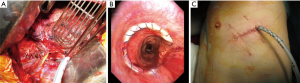
The postoperative period was uneventful. A routine bronchoscopy on the 7th postoperative day showed an intact tracheobronchial anastomosis with good mucosal vascularization (Figure 2C). The histopathological examination of the specimen (Figure 3) confirmed R0 resection. Pathological stages for synchronous primary lung carcinomas were pT4pN0M0, IIIA and pT2bpN0M0, IIA (8th edition of TNM Classification for Lung Cancer). Six months after the operation the patient remained in a good overall condition (ECOG 1) and the follow-up CT scan didn’t show any signs of recurrence.

Discussion
Left tracheal sleeve pneumonectomy is a technically complex procedure, as it requires good surgical exposure for patient safety and complete tumor resection. The historically established surgical approaches have certain degree of disadvantages (1). The use of left thoracotomy is restricted due to the aortic arch placement over the left main bronchus and tracheal carina. Median sternotomy provides better access, but complete mediastinal lymph node dissection is not feasible. Bilateral thoracotomies and clamshell incision cause severe surgical trauma resulting in increased postoperative complication and mortality rates. The implementation of multiport VATS has reduced surgical trauma and offers an adequate exposure for left tracheal sleeve pneumonectomy (3). Recent studies have reported the feasibility, safety and faster recovery of uniport VATS compared to multiport approach in major pulmonary resections (4). Although a feasibility of single port VATS for right tracheal sleeve pneumonectomy has been reported (5), uniportal VATS has never used for left tracheal sleeve pneumonectomy. Our novel single-stage approach incorporating right serratus-sparing thoracotomy and left uniportal VATS is a step further in minimizing invasiveness of the left tracheal sleeve pneumonectomy without compromising patient safety nor oncological principles of complete resection. The VATS pneumonectomy in this case did not significantly differ from a standard one. This case shows that uniportal VATS can be easily used for the benefit of the patient even in the most complex surgical cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Weder W, Inci I. Carinal resection and sleeve pneumonectomy. Thorac Surg Clin 2014;24:77-83. [Crossref] [PubMed]
- Rea F, Marulli G, Schiavon M, et al. Tracheal sleeve pneumonectomy for non small cell lung cancer (NSCLC): short and long-term results in a single institution. Lung Cancer 2008;61:202-8. [Crossref] [PubMed]
- Ai B, Liao Y, Zhang Z, et al. Single-stage bilateral thoracic surgery via a combined VATS and open approach for left central bronchogenic carcinoma with carinal invasion: report of two cases. J Cardiothorac Surg 2015;10:76. [Crossref] [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [PubMed]


