Cervical triangulating stapled anastomosis: technique and initial experience
Introduction
Despite the technical advances in gastric conduit formation or anastomotic methods, the anastomotic complications following the surgical resection of esophageal cancer (EC) have continued to perplex thoracic surgeons (1-6).
Triangulating stapled (TS) anastomosis for GEA has been shown to be associated with lower incidence of anastomotic complications (7-10). However, there was only one previous report comparing the results of TS with circular stapled (CS) anastomoses, and partially due to the limited number of patients, the incidence of anastomotic leak of both TS and CS was undesirable (TS, 2/8, 25.0% vs. CS, 1/12, 8.3%) (7).
In this report, we describe our surgical technique of TSA in the cervical part and examine its efficacy in compared with circular staplings.
Patients and methods
Patients
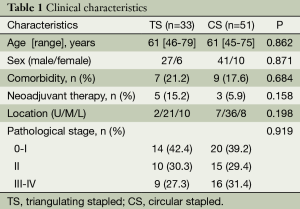
From January 2013 to November 2013, a total of 84 EC patients underwent minimally invasive esophagectomy (MIE) at Zhongshan Hospital of Fudan University were included in this retrospective study. The study was approved by the hospital ethics committee, and a waiver for individual patient consent for this retrospective study was also obtained from the ethics committee. All patients were diagnosed as EC by endoscopic biopsy. Physical examination, standard laboratory tests, electrocardiogram, and lung function test were performed in all patients. Preoperative staging was determined by enhanced thoracic and abdominal CT. According to the clinical findings, T1-3N0M0 EC patients were selected as candidates for MIE. The clinic characteristics of patients were shown in Table 1.
Full table
Surgical techniques
All operations were three-stage MIE, which was described in previous publications (11,12). The operation was performed by the same surgeon (L.T). A 3.0 cm wide gastric tube formed by linear staplers (TLC75, Ethicon Endosurgery, Cincinatti, OH, USA) was used for alimentary reconstruction. GEA was performed by cervical end to side CS anastomosis until July 2013 or a more proximal anastomosis which was difficult for TS (CS group, n=51) and by the cervical TSA after August 2013 (TS group, n=33).
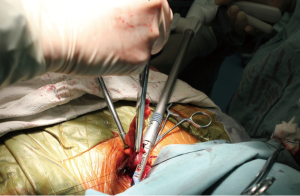
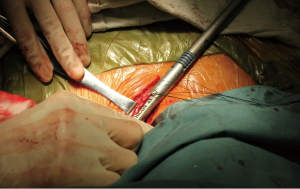
For the cervical TS, our surgical technique was basically similar to previous reports (7-9), in which an end-to-end GEA was performed using three linear staplers (Figures 1-4). The formed gastric tube was pulled up to the left neck through posterior mediastinal route. After two-thirds of the superior end of gastric tube was cut off by tissue scissor, three suspension sutures through the whole layer were added to secure the first anastomosis which was applied to posterior wall of the remnant esophagus and the gastric tube in an inverted fashion (Figure 1). Then these sutures were pulled up and completely removed with a linear stapler (ATB 45, Ethicon Endosurgery, Cincinatti, OH, USA). After two-thirds of the superior end of gastric tube was cut off by tissue scissor, three suspension sutures through the whole layer were added to secure the first anastomosis which was applied to posterior wall of the remnant esophagus and the gastric tube in an inverted fashion. Then these sutures were pulled up and completely removed with a linear stapler (ATB 45, Ethicon Endosurgery, Cincinatti, OH, USA). The second and the third anastomosis were performed in the same manner using the second and third linear staples; however, these were done in an everted instead of in an inverted fashion. At last, interrupted sutures of the serosa were performed between the anastomosis which was covered with the attached omenta. Then the triangulating shaped end-to-end anastomosis was completed between the remnant esophagus and the gastric tube in the cervical region. A closed suction drain was placed in the anastomotic region.
Statistical analysis
Differences between the TS and CS were assessed using the Wilcoxon rank sum test for continuous variables, the chi-square or Fisher exact tests for categorical variables. For all calculations, a P value of <0.05 was considered to be significant. Statistical computations were all performed by SPSS software, version 19.0 (SPSS, Inc, Chicago, IL, USA).
Results
In this study, eighty-four patients were enrolled, including 68 men (81%) and 16 women (19%). The median age was 61 years (range, 45-79 years). Sixteen patients presented with significant comorbidity and eight patients received neoadjuvant therapy. There were no significant differences in clinical characteristics between two groups (Table 1).
None of the procedures were converted to thoracotomy. Postoperative pathology reported that all cases were squamous cell carcinoma. The overall incidence of postoperative complications was significantly lower in TS than that in CS (15.2% vs. 35.3%, P=0.043). There was no significant difference in length of hospital stay, and mortality rate between two groups (Table 2).
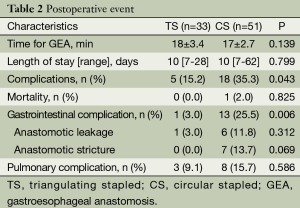
Full table
No difference was found for the mean time of GEA. In TS, there was only one minor leakage, which healed after 16 days of drainage. Of the six cases of leakage in the CS group, five (83.3%) were minor or moderate, and resolved after inserted drainage from a cervical drain However, One of these six patients in CS died of severe anastomotic leak during the perioperative period. Anastomotic leakage tended to occur less frequently in TS than in CS, although the difference was not significant (3.0% vs. 11.8%, P=0.312).
Patients who suffered swallowing dysfunction following the operation would receive endoscopic examination, and the stenosis was defined to the cases when endoscopic dilation at the anastomotic portion was required. Post-operative stenosis was found in 0.0% and 13.7% for the TS and CS anastomosis, respectively (Table 2).
Discussion
In this study, modified TS anastomosis was introduced to the gastroesophageal anastomosis (GEA) during MIE, and it was found to be superior to CS anastomosis in the incidence of postoperative complications. The overall gastrointestinal complication was significantly lower in TS following the surgery, which suggested TSA as a safe and effective alternative for GEA.
The gastric tube is the most commonly used conduit for the GEA. The major complications after GEA, including anastomotic leakage and anastomotic stricture, are frequently encountered, which would prolong patients’ hospital stay, compromise quality of life, and even be life-threatening (1,2,13,14). However, previous studies, either on gastric formation or anastomotic methods, were based on improvements of blood supply in the reconstruction of gastric conduits and the outcome was less promising (2,4-6).
There are encouraging results of TS anastomosis in both colo-colonic (15,16) and GEA (8,9). Theoretically, this end to end anastomosis preserves the integrity of vascular network of the gastric wall, which provides more blood supply to the anastomotic site. Furthermore, it allows reserving longer gastric tube and bringing less tension to the anastomotic site and it would be ideal for the passage of food. Finally, our modification that only two-thirds of the proximal gastric conduit was cut open for the GEA, which may ease the procedure of the first stapling for the anastomosis, and it would be convenient for further adjustment before the first linear stapler was fired. As in our study, anastomotic leak in TS had the tendency of reduction compared with CS.
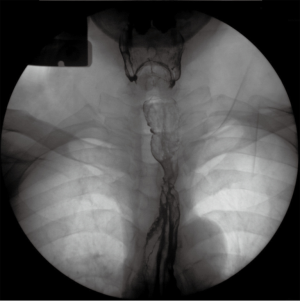
Conventionally, anastomotic stenosis after CS anastomosis occurs in 12.3-20% (17,18), which remains considerable concerns for this technique. The cause may include that all the layers of alimentary tract are punched out, which led to unexpected exposure to the inner lumen of the alimentary tract for the muscular layer (7). It is easily understood that this would increase the incidence of stenosis. For TSA, however, only one third of the anastomotic site is inverted, which theoretically may greatly eliminate the adverse effect caused by CS anastomosis. As a result, there was no anastomotic stenosis in TS (Figure 5), compared with 13.7% in CS (Table 2).
Additionally, other series reported reducing the time to perform GEA by using the TSA (7). Since this was our initial experience, the recorded time for GEA had no significant difference between two groups.
However, the limitations of our study include its nonrandomized retrospective study design and its lack of exploration of the long-term effects of TSA, especially on quality of life analysis. To minimize technical bias, all operations were performed under the guidance of one single experienced surgeon. We chose to include patients only in whom the esophageal bed was used as the route for the conduit pull-up, since the retrosternal route has been reported to be longer in length than the posterior route (19).
In conclusion, the TSA is a safely and effectively alternative method for cervical GEA. Further randomized controlled trails are needed to confirm this conclusion.
Conclusions
TSA is a safe and effective alternative for GEA, which would probably lower the incidence of leakage and stenosis following MIE. Further studies based on larger volumes are required to confirm these findings.
Acknowledgements
I would like to extend my deepest gratitude to my mentor, Dr. Lijie Tan, an honest, selfless and visionary scholar, who has instructed me how to conduct a good research, as well as what makes a good doctor.
Disclosure: The authors declare no conflict of interest.
References
- Kassis ES, Kosinski AS, Ross P Jr, et al. Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 2013;96:1919-26. [PubMed]
- Markar SR, Arya S, Karthikesalingam A, et al. Technical factors that affect anastomotic integrity following esophagectomy: systematic review and meta-analysis. Ann Surg Oncol 2013;20:4274-81. [PubMed]
- Kim RH, Takabe K. Methods of esophagogastric anastomoses following esophagectomy for cancer: A systematic review. J Surg Oncol 2010;101:527-33. [PubMed]
- Diana M, Hübner M, Vuilleumier H, et al. Redistribution of gastric blood flow by embolization of gastric arteries before esophagectomy. Ann Thorac Surg 2011;91:1546-51. [PubMed]
- Okushiba S, Kawarada Y, Shichinohe T, et al. Esophageal delta-shaped anastomosis: a new method of stapled anastomosis for the cervical esophagus and digestive tract. Surg Today 2005;35:341-4. [PubMed]
- Veeramootoo D, Shore AC, Wajed SA. Randomized controlled trial of laparoscopic gastric ischemic conditioning prior to minimally invasive esophagectomy, the LOGIC trial. Surg Endosc 2012;26:1822-9. [PubMed]
- Furukawa Y, Hanyu N, Hirai K, et al. Usefulness of automatic triangular anastomosis for esophageal cancer surgery using a linear stapler (TA-30). Ann Thorac Cardiovasc Surg 2005;11:80-6. [PubMed]
- Toh Y, Sakaguchi Y, Ikeda O, et al. The triangulating stapling technique for cervical esophagogastric anastomosis after esophagectomy. Surg Today 2009;39:201-6. [PubMed]
- Noshiro H, Urata M, Ikeda O, et al. Triangulating stapling technique for esophagogastrostomy after minimally invasive esophagectomy. Surgery 2013;154:604-10. [PubMed]
- Takemura M, Yoshida K, Fujiwara Y. Modified triangulating stapling technique for esophagogastrostomy after esophagectomy for esophageal cancer. Surg Endosc 2013;27:1249-53. [PubMed]
- Feng M, Shen Y, Wang H, et al. Thoracolaparoscopic esophagectomy: is the prone position a safe alternative to the decubitus position? J Am Coll Surg 2012;214:838-44. [PubMed]
- Shen Y, Zhang Y, Tan L, et al. Extensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single center. J Gastrointest Surg 2012;16:715-21. [PubMed]
- Sarela AI, Tolan DJ, Harris K, et al. Anastomotic leakage after esophagectomy for cancer: a mortality-free experience. J Am Coll Surg 2008;206:516-23. [PubMed]
- Kassis ES, Kosinski AS, Ross P Jr, et al. Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 2013;96:1919-26. [PubMed]
- Venkatesh KS, Morrison N, Larson DM, et al. Triangulating stapling technique: an alternative approach to colorectal anastomosis. Dis Colon Rectum 1993;36:73-6. [PubMed]
- Fukunaga Y, Higashino M, Tanimura S, et al. Triangulating stapling technique for reconstruction after colectomy. Hepatogastroenterology 2007;54:414-7. [PubMed]
- Xu QR, Wang KN, Wang WP, et al. Linear stapled esophagogastrostomy is more effective than hand-sewn or circular stapler in prevention of anastomotic stricture: a comparative clinical study. J Gastrointest Surg 2011;15:915-21. [PubMed]
- Petrin G, Ruol A, Battaglia G, et al. Anastomotic stenoses occurring after circular stapling in esophageal cancer surgery. Surg Endosc 2000;14:670-4. [PubMed]
- Hu H, Ye T, Tan D, et al. Is anterior mediastinum route a shorter choice for esophageal reconstruction? A comparative anatomic study. Eur J Cardiothorac Surg 2011;40:1466-9. [PubMed]