Effects of preventive therapy for latent tuberculosis infection and factors associated with treatment abandonment: a cross-sectional study
Introduction
According to WHO estimation, about 900,000 new TB cases still emerge each year in China. How to reduce case burden to meet the global END-TB target in 2035 has become the biggest challenge to China’s TB control program. Guangzhou, the capital of Guangdong Province, was estimated to have 11,463 new TB cases in 2014, representing an incidence rate of 136 TB cases per 100,000 individuals, which is much higher than the national average rate (68 new TB cases per 100,000 individuals).
Latent tuberculosis infection (LTBI) is defined as a state of persistent immune response to stimulation by Mycobacterium tuberculosis (MTB) antigens without evidence of clinically manifested active tuberculosis (TB) (1). It is estimated that one third of the world’s population is infected with MTB (2), and 5–10% of individuals with a LTBI will eventually progress to active TB (3). Furthermore, this progression rate can reach 40% among children under the age of 5 and with a LTBI (4). However, this progression can be averted by preventive therapy (PT). Sixty to ninety percent of individuals with a LTBI respond to currently available treatments (5), and PT given during childhood could reduce the odds of progression to active TB to less than 0.5% (6). Thus, the World Health Organization (WHO) regards identification and treatment of LTBIs as a tool for achieving global TB control.
Treatment for a LTBI subject involves the psychological challenge of convincing them of the need to treat a non-contagious infection that may never develop active TB with prolonged treatment that may cause potential adverse effects. The risk of developing TB disease following the initial infection depends on several factors, with the most important being the immunological status of the host (7). Some infected individuals may never develop active TB, but develop fatal INH-induced acute liver failure (8,9). Consequently, the potential benefits of treatment need to be carefully balanced against the risk of drug-related adverse events.
The global PT abandonment rates range from 20% to 80%, with the lowest proportions corresponding to clinical research sites (10). Therefore, knowing how to screen for high-risk LTBIs, select a reasonable treatment regimen, improve treatment adherence, and reduce the rate of treatment abandonment are all important factors for those with a LTBI to get benefit from PT. The current studies include only a small amount of data on PT abandonment, tolerance, and effectiveness under conditions of routine care (11-13). The aim of this study was to investigate the effects of PT on TB prevention and control, and describe the factors related to PT abandonment in a secondary vocational school in Guangzhou, southern China. The school had previously experienced an epidemic outbreak of TB, and its high-risk students and staff were screened with the purified protein derivative (PPD) test for LTBIs. A PT program was implemented according to the principle of voluntariness; after which, the participants were followed up for 2 years to observe the protective rate of PT and its ability to reduce the incidence of TB. Factors that influenced adherence of LIBI subjects to the PT protocol were also analyzed.
Methods
Study subjects
An outbreak of TB occurred in a secondary vocational school in Guangzhou, southern China during December 2014. A total of 5,160 individuals (436 staff and 4,724 students) were included in this study. Among the students, 1,760 were first-year students in secondary schools, 1,501 were second-year students, and 1,463 were third-year students. Additionally, 362 subjects with a PPD reaction induration diameter ≥15 mm, or with papules, blisters, and a normal chest X-ray image among 5,160 individuals were included as subjects for observation.
Study design
All of the staff and students were screened for clinical symptoms, and received a PPD skin testing and chest X-ray examination. Those with a reactive PPD induration diameter ≥15 mm, or with papules, blisters, and a normal chest X-ray image were asked to provide 3 sputum specimens (night sputum, morning sputum, and instant sputum) which were microscopically examined for acid-fast bacilli. If necessary, a chest CT examination and a consultation were conducted to exclude pulmonary TB.
PPD skin testing: (I) the PPD skin testing was performed in a uniform manner by professionals in the district TB Control Institute in Guangzhou, which are responsible for TB prevention and control work for the school; (II) PPD (5 TU) produced by the Chengdu Institute of Biological Products Co. Ltd. was intradermally injected (0.1 mL) at 1/3 of the inner side of the left forearm; (III) after 72 h, the local skin induration diameter was observed and measured [induration diameter = (transverse diameter + longitudinal diameter)/2 (mm)]. Papules and blisters were simultaneously recorded when present.
On the basis of full informed consent, the significance of the PT, the prescription for treatment, all possible side effects, and the treatment measures for side effects were all explained to the subjects in our study. In compliance with the principle of voluntariness, and whether the subject agreed to receive PT, the subjects were divided into two groups: a PT group and a control group. The PT group consisted of 156 cases (61 males and 95 females; mean age =17.96 years; range, 15 to 45 years) who received PT. The control group consisted of 206 cases (84 males and 122 females; mean age =18.05 years; range, 14 to 52 years) who did not receive PT. There were no significant differences in age and sex distribution between the two groups (P>0.05).
Subjects in the PT group took INH tablets (10–15 mg/kg/d; maximum dose of 300 mg/d) combined with RFP capsules (10–20 mg/kg/d, maximum dose of 600 mg/d) for three consecutive months. The drugs were provided free by the district TB Control Institute in Guangzhou. All supervision and management activities were performed by the doctors in the district TB Control Institute in Guangzhou, as well as by the school clinic.
Outcome measures: (I) all enrolled subjects in the PT group had normal liver function prior to receiving PT, and liver function tests and a complete blood count were repeated on a monthly basis; (II) the two groups of subjects were observed on a regular basis for 2 years, and all subjects received a chest X-ray examination at the end of the second year. Subjects who were suspected of having TB and/or those displayed chest X-ray abnormalities were asked to provide 3 sputum specimens for smear testing; (III) the district TB Control Institute in Guangzhou was responsible for the registration, verification, diagnosis, and treatment of all TB patients identified during our observation period.
An improved epidemiological questionnaire was used to investigate factors associated with the abandonment of treatment. The questionnaire consisted of three parts: (I) general demographic characteristics: gender, age; (II) history of epidemiology: history of BCG vaccination; (III) influencing factors: source of students (urban or rural), parental education level, body mass index (BMI), family monthly income, discrimination, worry about drug side effects, adverse drug reactions, and the opinions of non-TB specialists. All investigators were trained in a unified manner. Answers to questions provided during face-to-face interviews were used to fill in each item on the questionnaire, and another investigator was responsible for reviewing the quality of the survey.
Statistical analysis
All data were analyzed using IBM SPSS Statistics for Windows, Version 20 software (IBM Corp., Armonk, NY, USA). Differences between groups involving non-normally distributed data were analyzed using the rank sum test, and results are presented as the median value plus the minimum and maximum values. Differences between groups involving categorical data were analyzed using the chi square test, and results are presented as percentages. Univariate logistic regression analysis was used to analyze the relationships between various study factors and subjects abandonment of PT, and results were calculated as an odds ratio (OR) and its 95% confidence interval (95% CI). A multivariate non-conditional logistic regression analysis was then performed on univariate variables that were statistically significant, with the criteria for inclusion being a P value <0.05.
Results
Screening results
The total number of school staff and students eligible for inspection was 5,160, and the actual numbers of individuals inspected by chest X-ray and the PPD test were 4,767 (92.4%) and 4,761 (92.3%), respectively. Nine cases of active pulmonary TB were found (9/5,160, 0.17%). Additionally, 362 subjects had a reactive PPD induration diameter ≥15 mm, or displayed papules and blisters, but had a normal chest X-ray result; According to the study programme, all of the 362 subjects were recommended as the candidates for PT. The overall screening results are shown in Table 1.
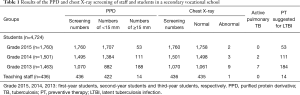
Full table
Medication in the PT group
Based on the principle of voluntariness, 156 cases (156/362, 43.1%) were enrolled in the PT group, and 206 cases (206/362, 56.9%) were enrolled in the control group. Among subjects in the PT group, 69 subjects completed the prescribed course of treatment, for a treatment completion rate of 44.2%. Among the 69 subjects who completed their treatment, 2 (2.9%) experienced 1–2 incidents of drug leakage during their course of treatment, and three leaked the total dose of medication. On average, each subject experienced drug leakage 1.5 times. Furthermore, 87 subjects failed to complete the prescribed course of treatment. Among those, 4 cases (4/87, 4.6%) took the medicine less than 1 month, 12 cases (12/87, 13.8%) took the medicine between 1 to 2 months, and 71 cases (71/87, 81.6%) took the medicine more than 2 months. The reasons for reluctance to continue taking the medicine included a variety of factors.
Rates of TB occurrence in both groups
Among the 156 cases in the PT group who received PT, two cases developed TB within 2 years, for a mean annual incidence rate of 0.64%. One case developed TB 13 months after initiating PT; however, that case had taken the prescription medication for only 1 month. Additionally, 1 case developed TB during the course of PT. Thus, 140 cases took the medicine over 2 months, one case developed TB within 2 years, for a mean annual incidence rate of 0.36%.
Among the 206 cases in the control group who did not receive PT, 20 cases of TB were diagnosed within a period of 2 years, for a mean annual incidence rate of 4.85%. Eighteen cases of TB occurred during the first year of observation, and 2 cases occurred during the second year.
Among the 22 cases developed TB, 15 cases were males and 7 cases were females. Besides, concomitant symptoms were found in 16 cases: 12 cases had a slight cough and a small amount of white sputum, 1 case had bloody sputum, 3 cases had a fever, and 2 cases complained mild chest pain. Twenty cases had a history of BCG vaccination and 18 cases had a TB scar, 11 cases had a history of close contact with individuals having pulmonary TB, 9 cases were boarders, 3 cases had a smoking history, 2 cases had a drinking history.
There was a significant difference in the incidence of TB in the two groups (χ2=9.981, P=0.002). When the incidence rate of TB was regarded as 100% in the control group, the incidence rate in the PT group was 7.4%, indicating that the protective rate of PT for reducing the incidence of TB was 92.6% [the protective rate of PT = (mortality in control group − mortality in PT group)/mortality in control group] ×100%.
The number of progressed to TB among individuals followed up for a period of 2 years in the secondary vocational school
Among 5,160 school staff and students, thirty-three cases had developed TB after 2 years of follow-up; among those, 9 cases were screened out at the first time, and 24 were secondary cases, including 22 cases (91.7%) with a reactive PPD induration diameter ≥15 mm, or with papules and blisters, and 2 cases (8.3%) with a reactive PPD induration diameter <15 mm. Moreover, 21 cases (87.5%) occurred during the first year of observation, and 3 cases (12.5%) occurred during the second year.
Classification of the TB which occurred in both groups
Among the cases of TB which occurred in the PT group, 2 cases were secondary pulmonary TB in which the sample tested negative for bacteria and the chest X-ray showed no cavity. In the control group, there were 17 cases of secondary pulmonary TB, 2 cases of secondary pulmonary TB combined with pleurisy, and 1 case of cervical lymph node TB. Moreover, 9 cases had the samples to be tested positive for bacteria (3 cases were sputum smear-positive and 6 cases were sputum culture-positive), and 3 cases showed cavity formation on a chest X-ray.
Adverse drug reactions
Among the 156 cases in the PT group, 19 cases (12.2%) experienced an adverse drug reaction. The adverse drug reactions included 12 cases of gastrointestinal reactions (7.7%), 3 cases of liver dysfunction (1.9%), 1 case of skin rash (0.6%), 2 cases of peripheral neuritis (1.3%), and 1 case of chest distress (0.6%). Thirteen of the 19 cases discontinued treatment because of adverse reactions, and 6 of the 19 cases completed the course of treatment after establishing symptomatic treatment and liver protection strategies.
Characteristics of LTBIs recommended for PT during the outbreak of pulmonary TB
Among the 362 LTBI cases, 293 hadn’t received or finished the PT, including 206 cases that stopped taking their medicines at the beginning of the observation period and 87 cases who abandoned PT after the treatment began, but before the treatment was completed. Sixty-nine cases completed the entire course of PT. Baseline characteristics of the two groups of subjects are shown in Table 2.
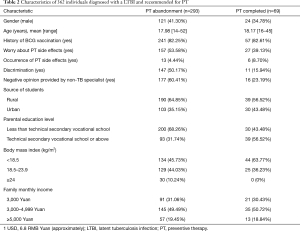
Full table
Univariate and multivariate analyses of baseline variables performed to identify factors associated with abandonment of PT in a secondary vocational school in Guangzhou, southern China
Logistic univariate and multivariate regression analyses were performed using the following factors as independent variables: gender, age, source of students, history of BCG vaccination, parental education level, BMI, family monthly income, worry about adverse drug reactions, the occurrence of adverse drug reactions, opinion of non-TB specialists, and discrimination; the status of PT abandonment served as the dependent variable. Our results indicated that discrimination, worry about adverse drug reactions, a low parental education level, and a negative opinion expressed by a non-TB specialist increased the risk of PT abandonment among LTBI subjects. Detailed results of our analyses are shown in Table 3.
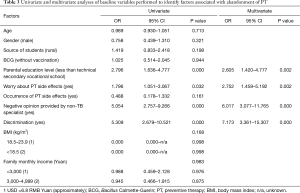
Full table
Discussion
China is still a country with a high burden of TB. Current interventions used to control TB are primarily focused on the early detection and treatment of TB sources, preventing the spread of MTB, and reducing the likelihood of an MTB infection (14). However, it is impossible to reduce or eliminate the source of a TB infection that has not been previously shown to disseminate MTB in the type of population being examined, not to mention successfully preventing LTBIs from progressing to TB, indicating PT can reduce the number of MTB in infected individuals and decrease the likelihood to develop active TB, which is one of the important measures to control TB outbreaks among high-risk groups in low epidemic areas (15,16). In this study, a total of 5,160 staff and students from a secondary vocational school in Guangzhou, southern China were screened using the PPD test, and 362 cases of high-risk LTBI were identified. Based on the principle of voluntariness, there were 156 cases in the PT group and 206 cases in the control group, and both groups were followed up for 2 years. The results showed that 2 cases of TB occurred in the PT group and 20 cases of TB occurred in the control group, and the mean annual incidence rates of 0.36% and 4.85%, respectively. When PT was used to reduce the incidence of TB, its overall protective rate was 92.6%. Among the 362 cases with LTBIs, 69 completed the prescribed course of treatment and 293 hadn’t received or finished the PT. A multivariate logistic regression analysis revealed that discrimination, worry about adverse drug reactions, a low parental education level, and a negative opinion provided by a non-TB specialist were all factors to abandon PT among LTBI subjects. The results of our present study can help officials in the Department of Health and Education to screen subjects in schools and more readily identify those at high risk for a LTBI. Our findings can also help to improve the treatment adherence of LTBI cases, reduce the incidence of TB in those cases, and prevent subsequent outbreaks of TB in schools.
After 2 years of follow-up, our data showed that 33 cases of TB occurred during the school epidemic and 24 were secondary cases; among those, 91.7% with a reactive PPD induration diameter ≥15 mm, or with papules and blisters, and 8.3% with a reactive PPD induration diameter <15 mm. Our results suggest that during the period of the TB epidemic at the school, subjects with a reactive PPD induration diameter ≥15 mm, or with papules and blisters comprised the high-risk population that accounted for 91.6% of TB patients. This estimated rate is significantly higher than the 80.8% rate measured in a study conducted by Tu et al. (17), and the difference might be due to differences in the subject groups and follow-up periods.
INH is an oral anti-tuberculous drug with activity against both intracellular and extracellular MTB. The regimen with daily INH for 6 to 12 months has been the mainstay of LTBI therapy for five decades. Evidence supporting this practice includes a series of randomized clinical trials conducted in the mid-twentieth century which showed that daily administration of INH in treatment of LTBIs reduced the subsequent incidence of TB by 60% to 90% (16). A meta-analysis of placebo-controlled studies found that the OR in the subjects with a LTBI and treated with INH will subsequently develop TB was 0.64 (95% CI, 0.48–0.83), when compared with the placebo-group (18). A longer course of treatment is not conducive for completing therapy. Along with the recent progress made in developing short-term chemotherapy regimens, some PT regimens have also been shortened. The WHO pointed out in the 2016 Global TB Report that subjects with a LTBI and given the therapeutic regimen of INH plus rifampin for 3–4 months had incidences of TB and hepatotoxicity that were equivalent to those among subjects treated with INH alone for 6 months (OR =0.89, 95% CI, 0.65–1.23; OR =0.89, 95% CI, 0.52–1.55) (7). We found that among the subjects who received INH combined with RFP for 3 consecutive months, the protective rate during our 2-year observation period was 86.8%, the adverse reaction rate was 12.2%, and the rate of hepatotoxicity was 1.9%. No serious adverse events were observed. Therefore, the regimen used in our study was reasonable for use as PT in schools, and can be used by the Departments of Health and Education for reducing the incidence of pulmonary TB during future school TB epidemics in the future.
Discrimination is a potential barrier to receiving PT. The discrimination attached to TB in China can lead to the imposition of socio-physical distance and participatory restrictions on those suffering from the disease (19). A full 95% of those interviewed believed that people with TB tend to hide their TB status out of fear of what others may say (20). We found that 147 subjects (50.17%) in the PT abandonment group refused PT or abandoned their treatment due to a fear of discrimination or suffering discrimination. Moreover, a multivariate logistic regression analysis revealed that discrimination was one of major factors associated with PT abandonment (OR =7.173, 95% CI, 3.361–15.307). We speculate that two factors might account this finding: (I) some people believe that a LTBI is actually TB, owing to a lack of understanding of LTBIs in their social groups; (II) many individuals had a poor awareness of the risks associated with contracting a LTBI. Responses to the questions in our survey suggested that discrimination may influence a TB patient’s decision to seek treatment or adhere to a therapeutic regimen. Therefore, future interventions should be directed at improving attitudes and perceptions to potentially reduce the discrimination attached to TB in school populations by the Departments of Health and Education.
Adverse events caused by anti-TB drugs are common in clinical settings, and some events, such as INH-induced acute liver failure, can be severe (8). We also found that students and parents were aware of these possible adverse reactions through the Internet, as 157 (53.58%) subjects in the PT abandonment group refused PT or abandoned their treatment for fear of adverse drug reactions. However, only 13 cases (4.44%) abandoned treatment because of PT side effects. Our univariate logistic regression analysis showed that the incidence of worry about adverse drug reactions in the PT abandonment group was 1.796-fold higher than that in the PT completion group (P=0.032). Moreover, after all confounding factors had been controlled in the multivariate logistic regression analysis, the OR value for this factor was 2.752 (P=0.002), indicating that worry about adverse drug reactions was the main factor associated with PT abandonment in the secondary vocational school. However, the occurrence of adverse drug reactions was not included in our multivariate analysis (P>0.05).
Student adherence to a medication treatment regimen is greatly influenced by their parents’ education level, as parents who are highly educated may have a better understanding of the disease being treated, and be more likely to believe in the benefits of treatment. Previous studies showed that lack of a basic education was the main socio-economic factor associated with TB treatment non-adherence and patients being lost to follow up (21-24). Our study results indicated that students whose parents had a low education level were prone to be non-adherent with PT (OR =2.605; 95% CI, 1.420–4.777).
At present, the benefit of PT for LTBI subjects, and especially the long-term benefit, is controversial. In a recent study, MTB was found in stem cells during the presence of a latent infection. In that case, PT did not completely eliminate the MTB and did not prevent the subsequent development of TB (25). Moreover, genetic alterations found in latent MTB infections may also lead to drug resistance due to PT, and many non-TB specialists hold negative opinions about PT. In our study, 177 subjects (60.41%) in the PT abandonment group accepted the views of non-TB specialists to refuse PT or abandoned their treatment after receiving PT for a while. Furthermore, our multivariate logistic regression analysis showed that the opinions of non-TB specialists increased the risk of LTBI subjects abandoning PT (OR =6.017; 95% CI, 3.077–11.765). Therefore, clinicians, and especially primary-care physicians, need to popularize the knowledge of guidelines used for managing LTBIs as an important component of the "End TB strategy" developed by the WHO.
Study limitations
A limitation of this study is that the students and staff from only one school involved in the TB epidemic in Guangzhou were followed up for a period of 2 years. Additional analyses of the students and staff from other schools involved in the TB epidemic are needed. Future analyses should include non-TB epidemic time periods and extend the follow up period to 5 years. These changes will make it possible to better examine the high-risk LTBI populations present in schools with TB outbreaks, influence school TB prevention programs, and increase subjects adherence to anti-TB treatment.
Conclusions
The results of this study suggest that implementation of PT for high-risk LTBI populations during the school TB epidemic in Guangzhou was clearly beneficial, and the regimen of INH combined with RFP for 3 consecutive months was reasonable. Nevertheless, PT must be initiated in conjunction with “source of infection” control work; otherwise, the source of infection will continue to spread and induce new TB infections, and the practical significance of PT for TB control will not be fully realized. Discrimination, worry about adverse drug reactions, a low parental education level, and accepting the opinion of a non-TB specialist are all factors that may increase the risk for treatment abandonment among LTBI cases. Therefore, gaining the ability to increase communication with LTBI cases and overcome their psychological disorders is a key requisite for improving their treatment adherence. Our implementation of PT involved extensive publicity on campus, as well as coordination among school leaders, the school clinic, and the district TB Control Institute in Guangzhou. We also provided the PT at no cost and on the basis of informed consent. In addition, subjects who received and completed their PT were awarded a nutrition fee of 300 Yuan (RMB). All of these measures helped to guarantee the smooth progress of PT, and can be incorporated into future PT studies.
Acknowledgements
We thank the Health and Family Planning Commission of Guangzhou Municipality, the Guangzhou Centers for Disease Control and Prevention (CDC), the Guangzhou Chest Hospital, the district TB Control Institute in Guangzhou, and the secondary vocational school for their support to conduct this study.
Funding: This work was sponsored by National Natural Science Foundation of China (81470856 and 81360001).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethical Review Board of Guangzhou Centers for Disease Control and Prevention (CDC) and the Ethics Committee of the secondary vocational school (xkyy201506 and gdsmzzyxx201507). The objective of the study was explained in detail to study participants and their parents (students under the age of eighteen), and an informed consent form was signed by each individual and their parents (students under the age of eighteen) before conducting the interview. All of the subjects were voluntary and they could withdraw from the study at any stage if they desired. Participants’ confidentiality was guaranteed by not recording their personal identifiers on the questionnaire.
References
- Mack U, Migliori GB, Sester M, et al. LTBI: latent tuberculosis infection or lasting immune responses to M. tuberculosis? A TBNET consensus statement. Eur Respir J 2009;33:956-73. [Crossref] [PubMed]
- Dye C, Scheele S, Dolin P, et al. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. JAMA 1999;282:677-86. [Crossref] [PubMed]
- Comstock GW, Livesay VT, Woolpert SF. The prognosis of a positive tuberculin reaction in childhood and adolescence. Am J Epidemiol 1974;99:131-8. [Crossref] [PubMed]
- Succi RC. The challenge of diagnosing tuberculosis in children. Rev Paul Pediatr 2014;32:2-3. [Crossref] [PubMed]
- Lobue P, Menzies D. Treatment of latent tuberculosis infection: an update. Respirology 2010;15:603-22. [Crossref] [PubMed]
- Mendonça AM, Kritski AL, Land MG, et al. Abandonment of Treatment for Latent Tuberculosis Infection and Socioeconomic Factors in Children and Adolescents: Rio De Janeiro, Brazil. PLoS One 2016;11. [Crossref] [PubMed]
- World Health Organization. Global tuberculosis report 2016.
- Miyazawa S, Matsuoka S, Hamana S, et al. Isoniazid-induced acute liver failure during preventive therapy for latent tuberculosis infection. Intern Med 2015;54:591-5. [Crossref] [PubMed]
- Durand F, Bernuau J, Pessayre D, et al. Deleterious influence of pyrazinamide on the outcome of patients with fulminant or subfulminant liver failure during antituberculous treatment including isoniazid. Hepatology 1995;21:929-32. [Crossref] [PubMed]
- Hirsch-Moverman Y, Daftary A, Franks J, et al. Adherence to treatment for latent tuberculosis infection: systematic review of studies in the US and Canada. Int J Tuberc Lung Dis 2008;12:1235-54. [PubMed]
- Machado A, Finkmoore B, Emodi K, et al. Risk factors for failure to complete a course of latent tuberculosis infection treatment in Salvador, Brazil. Int J Tuberc Lung Dis 2009;13:719-25. [PubMed]
- Durovni B, Cavalcante SC, Saraceni V, et al. The implementation of isoniazid preventive therapy in HIV clinics: the experience from the TB/HIV in Rio (THRio) study. AIDS 2010;24 Suppl 5:S49-56. [Crossref] [PubMed]
- Sant'Anna CC, David SG, Marques AM. Antituberculosis chemoprophylaxis in a public hospital - study of 100 children. J Pediatr (Rio J) 2000;76:413-20. [Crossref] [PubMed]
- Marks GB, Bai J, Simpson SE, et al. Incidence of tuberculosis among a cohort of tuberculin-positive refugees in Australia: reappraising the estimates of risk. Am J Respir Crit Care Med 2000;162:1851-4. [Crossref] [PubMed]
- Chen W, Cheng S. Latent tuberculosis infection sreening and preventive therapy in students. Zhonghua Jie He He Hu Xi Za Zhi 2016;39:21-4. [PubMed]
- Fox GJ, Dobler CC, Marais BJ, et al. Preventive therapy for latent tuberculosis infection-the promise and the challenges. Int J Infect Dis 2017;56:68-76. [Crossref] [PubMed]
- Tu D, Liu Y, Zhang L. Tuberculin reactivity criteria for chemoprophylaxis in college students. Journal of the Chinese Antituberculosis Association 2006;28:21-4.
- Stagg HR, Zenner D, Harris RJ, et al. Treatment of latent tuberculosis infection: a network meta-analysis. Ann Intern Med 2014;161:419-28. [Crossref] [PubMed]
- Xu W, Lu W, Zhou Y, et al. Adherence to anti-tuberculosis treatment among pulmonary tuberculosis patients: a qualitative and quantitative study. Bmc Health Serv Res 2009;9:169. [Crossref] [PubMed]
- Cramm JM, Finkenflugel HJ, Moller V, et al. TB treatment initiation and adherence in a South African community influenced more by perceptions than by knowledge of tuberculosis. BMC Public Health 2010;10:72. [Crossref] [PubMed]
- Maruza M, Albuquerque MF, Coimbra I, et al. Risk factors for default from tuberculosis treatment in HIV-infected individuals in the state of Pernambuco, Brazil: a prospective cohort study. BMC Infect Dis 2011;11:351. [Crossref] [PubMed]
- Vijay S, Kumar P, Chauhan LS, et al. Risk factors associated with default among new smear positive TB patients treated under DOTS in India. PLoS One 2010;5. [Crossref] [PubMed]
- Tachfouti N, Slama K, Berraho M, et al. The impact of knowledge and attitudes on adherence to tuberculosis treatment: a case-control study in a Moroccan region. Pan Afr Med J 2012;12:52. [PubMed]
- Garrido MS, Penna ML, Perez-Porcuna TM, et al. Factors associated with tuberculosis treatment default in an endemic area of the Brazilian Amazon: a case control-study. PLoS One 2012;7. [Crossref] [PubMed]
- Raghuvanshi S, Sharma P, Singh S, et al. Mycobacterium tuberculosis evades host immunity by recruiting mesenchymal stem cells. Proc Natl Acad Sci U S A 2010;107:21653-8. [Crossref] [PubMed]


