Survival of the fittest: the role of video-assisted thoracoscopic surgery in thoracic impalement injuries
Introduction
Trauma is the leading cause of death among those under the age of 45 in Taiwan (1). According to the literature, thoracic injuries account for approximately 25% of trauma-related deaths, with an estimated one-third of these mortalities being immediate because of injury severity (2).
The incidence of penetrating thoracic trauma associated with the use of firearms, stabbings, and impalement in urban trauma centers has been increasing, with the majority being secondary to gunshot wounds in North America (3). In contrast, gunshot-associated injuries are rare in Taiwan. Instead, injuries due to stabs and impalement occur more frequently.
Thoracic impalement injury is rare and among the most severe forms of thoracic trauma because of its high morbidity and mortality. Kelly et al. (4) introduced principles for the management of impalement injuries in 1995. After healthcare professionals provide basic life support to minimize blood loss and avoid further damage, the impaling object should be left in situ during patient transport; if necessary, truncation should be performed beyond the edges of the skin.
Penetrating trauma to the chest has significant on-scene mortality, directly related to the organs involved (5). Pre-hospital mortality rates are high owing to the involvement of the heart and great vessels. However, patients who reach the hospital in a hemodynamically stable state might be considered to sustain injury that did not affect vital internal structures.
Traditionally, open thoracotomy has been the standard approach for the safe retrieval of an object impaled in the chest. A wide incision provides the surgeon excellent exposure and allows removal of the object under direct vision, as well as expeditious repair of associated vascular or visceral injuries.
The use of video-assisted thoracoscopic surgery (VATS) has recently provided an alternative way to simultaneously diagnose and manage patients with thoracic trauma (6). With exhaustive work-ups of imaging studies, VATS has become a technically feasible scouting procedure.
Hence, we aimed to conduct a retrospective study of VATS for managing thoracic impalement injuries at our institution, while attempting to define the feasibility and value of exploratory VATS.
Methods
This study was approved by the institutional review board of Kaohsiung Medical University Hospital (approval number: KMUHIRB-E(I)-20170051) and the need for informed consent was waived. We performed a retrospective review of thoracic impalement injuries receiving exploratory VATS from November 2010 to July 2016. Four patients received VATS-based management for thoracic impalement injuries.
Patient 1
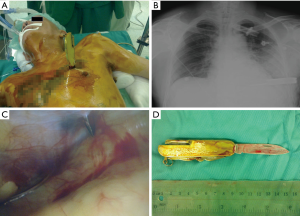
A 54-year-old man with a history of schizophrenia, sustained a self-inflicted injury involving a knife impaled above the left nipple in the chest (Figure 1A). He was transported to a small community hospital. Although he was hemodynamically stable, level-I surgical capabilities were not available; thus, transfer was requested. Before transfer, he was endotracheally intubated because of agitation and to ensure that the embedded knife remained undisturbed. On arrival, he appeared hemodynamically stable, with his breath-sounds equal, without obvious decrease. Follow-up chest X-ray demonstrated one metallic foreign body extending into left chest cavity with slight increased left opacity (Figure 1B). Hemopneumothorax was not evident, and he was emergently taken to the operating room. With the patient stable under general anesthesia, exploratory VATS was performed. Operative findings showed the knife (Figure 1C) piercing through the mediastinum without injury to heart and lung (Figure 1D). Extraction was performed under direct vision without hemorrhage. He had an uneventful postoperative recovery.
Patient 2
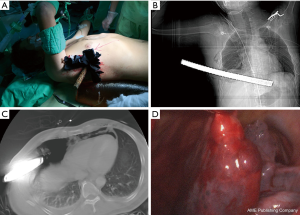
A 47-year-old male construction worker fell two stories and sustained an impalement injury to his right lower chest. In the emergency department, the patient was awake and alert, vital signs were normal, and he complained of shortness of breath and right chest pain. Physical examination revealed relatively diminished breath-sound in the right chest. An iron drill had impaled into the right thoracoabdominal region, below the nipple, without other external trauma (Figure 2A). Anterior-posterior chest X-ray revealed a moderate amount of fluid collection in the right lung field, with a foreign body seen at the lung base, (no pneumothorax was observed) (Figure 2B). Focused abdominal sonography for trauma (FAST) revealed right hemothorax without evident intraperitoneal fluid in Morrison’s pouch in accordance with the radiological findings. Because of possible hindering of the foreign body, closed thoracostomy was not performed. Since the patient remained hemodynamically stable, he was transferred to the operating room directly. VATS was performed initially in the left decubitus position for clot evacuation (Figure 2C), followed by laparoscopy in the supine position. Intraoperative findings included diaphragmatic and liver lacerations with the iron drill penetrating through the pleural cavity into the peritoneal cavity (Figure 2D). The drill was extracted under direct laparoscopic vision and lacerations were repaired securely. The patient recovered well without sequelae.

Patient 3 (7)
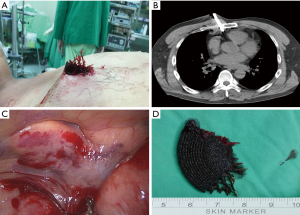
A 39-year-old male construction worker fell from height and landed with his right lateral chest on an iron rod. After the rod was sawed, the patient was rushed to the emergency department. He was hemodynamically stable and alert upon arrival. No other traumatic injuries were observed upon gross examination. The point of entry of the rod was the sixth intercostal space and midaxillary line (no exit site was observed) (Figure 3A). Enhanced computed tomography (CT) revealed the rod to be crossing the entire right chest cavity through the mediastinum with mild hemopneumothorax (Figure 3B,C).
After close monitoring, VATS was performed in the left semi-decubitus position, allowing for an easier surgical approach and urgent sternotomy or thoracotomy, if necessary (Figure 3A). A 2-cm thoracoscopic incision was made at the eighth intercostal space and posterior axillary line. Under direct vision, the rod was carefully removed without bleeding. Retained blood clots was evacuated. Other than minor lung contusion, there was no injury to the heart, great vessels, or diaphragm (Figure 3D). The patient was discharged soon after.
Patient 4
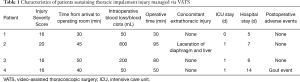
A 44-year-old worker was brought to the emergency department after an angle grinder explosion. On arrival, he was alert and hemodynamically stable. One major fragment of the grinder disc had embedded in his right anterior chest (Figure 4A). There was no other apparent injury. Hemothorax or pneumothorax was insignificant on chest radiography. Given his hemodynamic stability, a non-enhanced chest CT was performed and revealed the trajectory of foreign body insertion and the surrounding pneumomediastinum and pneumopericardium (Figure 4B). Owing to suspicion of injury to mediastinal or pericardial structures, an exploratory right single-port VATS was initiated through fifth intercostal space on the midaxillary line, which ultimately revealed mediastinal hematoma without internal thoracic vessel and cardiac injury (Figure 4C). The foreign body (Figure 4D) was extracted under direct thoracoscopic vision, followed by chest wall debridement. He made an uneventful recovery.
Results
VATS was successfully utilized as a diagnostic and therapeutic strategy in 4 patients with thoracic impalement injuries (Table 1). All patients met the institutional criteria of trauma-team activation and the multidisciplinary approach was applied. In particular, under meticulous surveillance of the trauma-team members, closed thoracostomy was not adopted for patient 2 and 3 who actually had hemothorax or pneumothorax. This was primarily due to the patient’s relatively stable condition throughout the course of resuscitation and radiologic investigation while the trauma team was concerned with possible dislocation of the impaled object during chest tube insertion. Instead, we prepared the emergent thoracotomy tray with experienced personnel at the trauma bay, and expedited the surgery. Perioperative courses were uneventful in all patients undergoing exploratory VATS. Only patient 2 sustained extrathoracic injury, who received subsequent laparoscopic intervention for repairing the partial laceration of diaphragm and liver. In patient 4, the postoperative hospital stay was relatively lengthened because of gout event. All patients resumed their daily activities without morbidity during the follow-up period.
Full table
Discussion
VATS is safe and effective for elective major thoracic procedures worldwide. Since Branco first described thoracoscopy to aid in the diagnosis and treatment of patients with penetrating chest injuries in 1943 (8), its use in acute thoracic trauma treatment has gained increasing popularity over the last several decades. VATS has proved to be effective for hemodynamically stable patients with retained hemothorax, persistent pneumothorax, empyema, and mediastinal or diaphragmatic exploration (9), even for penetrating thoracic injuries with retained foreign bodies (10,11). Nevertheless, reports regarding the use of VATS for thoracic impalement injuries are still sparse (12-18). Our results strengthen the importance of VATS-based approaches to major chest trauma management.
Comparing similar cases in the literature (Table 2), we found that the injuries were mostly attributed to violent assault or fall. The common impaled objects were knives or iron rods. Bowley et al. (19) reported that thoracic impalements are most commonly right sided, presumably because of the reduced risk of striking the heart or great vessels on the left. Patient who survived till the hospital are a kind of a “natural selection” group. Thus, their chances of survival are high. Patients with impalements involving the left chest could be managed via VATS if detailed imaging was performed (Table 2).
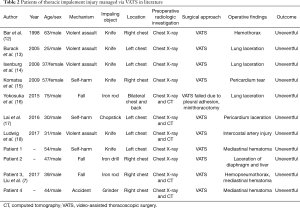
Full table
Thoracotomy undoubtedly has been the standard approach to treat thoracic impalement injury owing to its safety and good exposure of the intrathoracic cavity. In hemodynamically normal patients undergoing thorough imaging-based assessment in conjunction with multidisciplinary team work, VATS (7,13), and even non-operative management (20) may take a preceding role because the impaled object was preoperatively assumed to generate limited damage to adjacent structures.
Beyond preoperative assessment, uneventful anesthesia in one-lung ventilation and optimized operative position are also paramount. Perioperative tactics formulated by anesthesiologist and surgeons is essential. All our 4 patients were positioned in the supine or semi-decubitus position for better surgical approach and were prepared for conversion to open thoracotomy or cardiopulmonary bypass, if necessary.
In addition to the widely-known benefits including less invasiveness, decreased pain, and early postoperative recovery, VATS enables creation of an intercostal incision away from the penetrating wound without disturbing the impaled object. This provides visual surveillance during the extraction process, and eventually eliminates the need for conventional thoracotomy, as previously reported in literature (7,14). In the present study, VATS was employed successfully for extracting impaled objects in all patients without the conversion to open thoracotomy. Moreover, clot evacuation, diaphragmatic repair, and mediastinal debridement were also managed concomitantly. It is noteworthy that our study demonstrates the capability of VATS in handling a wide array of impaled foreign bodies, including a knife, iron drill, iron rod, and disc of a grinder, in time-critical needs of severely injured patients.
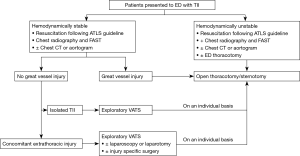
Advancement and spreading of knowledge are crucial to translate science into action. Since the use of VATS in thoracic impalement injury has not been validated well in literature, we here propose a management algorithm for thoracic impalement injury based on our experience and the principles of ATLS (Figure 5). We still emphasize that the use of VATS should be contraindicated in circumstances of hemodynamic instability, severe intrathoracic adhesions, intolerance of one-lung ventilation, and possible injuries to cardiac or great vessels. Conversion to sternotomy or thoracotomy should be promptly attempted to ensure the patient’s safety. Greater precision of trauma care in the fast-paced setting could be achieved with the implementation of the complementary role of VATS in the specific group.
Although our results are promising. The generalizability is limited by the extremely small sample size thanks to the inherent rarity of thoracic impalement injury and the anticipated underutilization of VATS. Nevertheless, to our knowledge, this is the first study to report the comparatively large series of thoracic impalement injury managed by VATS. Although our results are quite preliminary, we believe this is a first step towards better and personalized care for maximizing the merit of VATS in chest trauma.
In conclusion, just like the famous phrase “survival of the fittest,” those who could reach the hospital alive with thoracic impalement injuries might have been naturally selected. Multidisciplinary approaches to balance timeliness and precision is warranted. VATS-based management could be a tool enabling strategic superiority for managing hemodynamically stable patients with thoracic impalement injuries.
Acknowledgements
The authors thank the help of Meng-Chien Hsieh on language revision.
Funding: This work was partially supported by grants from the Kaohsiung Medical University Hospital (KMUH103-3R63) and the Ministry of Science and Technology, Taiwan, R.O.C. (MOST 106-2314-B-037-037).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the institutional review board of Kaohsiung Medical University Hospital (approval number: KMUHIRB-E(I)-20170051) and the need for informed consent was waived. Patient informed consent cannot be obtained because the patient could not be traced and we assure the information can be sufficiently anonymized throughout the manuscript. Additionally, images used in our manuscript are anonymized by the removal of any identifying marks and are not accompanied by text that could reveal the patient’s identity through clinical or personal detail.
References
- Ministry of Health and Welfare, Taiwan R.O.C. 2016 statistics of causes of death. Available online: https://www.mohw.gov.tw/dl-33662-7bc7488c-e7bd-46a3-9d24-60e0a277444f.html
- Prabhakar G, Graeber G. Chest trauma: minimal access cardiothoracic surgery. In: Yim APC, Hazelrigg SR, Izzat MB, et al. editors. London: WB Saunders, 2000:308-15.
- Baillot R, Dontigny L, Verdant A, et al. Penetrating chest trauma: a 20-year experience. J Trauma 1987;27:994-7. [Crossref] [PubMed]
- Kelly IP, Attwood SE, Quilan W, et al. The management of impalement injury. Injury 1995;26:191-3. [Crossref] [PubMed]
- Davis JS, Satahoo SS, Butler FK, et al. An analysis of prehospital deaths: Who can we save? J Trauma Acute Care Surg 2014;77:213-8. [Crossref] [PubMed]
- Manlulu AV, Lee TW, Thung KH, et al. Current indications and results of VATS in the evaluation and management of hemodynamically stable thoracic injuries. Eur J Cardiothorac Surg 2004;25:1048-53. [Crossref] [PubMed]
- Liu YW, Tsai DL, Chou SH, et al. Video-assisted thoracoscopic surgery for thoracic impalement with an iron rod. Ann Thorac Surg 2017;104:1438-9. [Crossref] [PubMed]
- Branco J. Thoracoscopy as a method of exploration in penetrating injuries of the thorax. Dis Chest 1946;12:330-5. [Crossref] [PubMed]
- Smith JW, Franklin GA, Harbrecht BG, et al. Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. J Trauma 2011;71:102-5; discussion 105-7. [Crossref] [PubMed]
- Williams CG, Haut ER, Ouyang H, et al. Video-assisted thoracic surgery removal of foreign bodies after penetrating chest trauma. J Am Coll Surg 2006;202:848-52. [Crossref] [PubMed]
- Yu PS, Chan HH, Lau RW, et al. Penetrating thoracic injury with retained foreign body: can video-assisted thoracic surgery take up the leading role in acute management? J Thorac Dis 2016;8:2247-51. [Crossref] [PubMed]
- Bar I, Rivkind A, Deeb M, et al. Thoracoscopically guided extraction of an embedded knife from the chest. J Trauma 1998;44:222-3. [Crossref] [PubMed]
- Burack JH, Amulraj EA, O'Neill P, et al. Thoracoscopic removal of a knife impaled in the chest. J Thorac Cardiovasc Surg 2005;130:1213-4. [Crossref] [PubMed]
- Isenburg S, Jackson N, Karmy-Jones R. Removal of an impaled knife under thoracoscopic guidance. Can Respir J 2008;15:39-40. [Crossref] [PubMed]
- Komatsu T, Neri S, Fuziwara Y, et al. Video-assisted thoracoscopic surgery (VATS) for penetrating chest wound: thoracoscopic exploration and removal of a penetrating foreign body. Can J Surg 2009;52:E301-2. [PubMed]
- Yokosuka T, Kobayashi T, Fujiogi M, et al. An unusual case of thoracic impalement injury with severe pleural adhesion. Gen Thorac Cardiovasc Surg 2015;63:298-301. [Crossref] [PubMed]
- Lai CC, Liu CY. Trans-pericardial penetration in a stab injury to the chest. Eur J Cardiothorac Surg 2016;49:1015. [Crossref] [PubMed]
- Ludwig C, Koryllos A. Management of chest trauma. J Thorac Dis 2017;9:S172-S177. [Crossref] [PubMed]
- Bowley DM, Gordon MP, Boffard KD. Thoracic impalement after ultralight aircraft crash. J Thorac Cardiovasc Surg 2003;125:954-5. [Crossref] [PubMed]
- Frangos SG, Ben-Arie E, Bernstein MP, et al. Thoracic stab wound with impaled knife. J Trauma 2006;60:1379. [Crossref] [PubMed]


