A 7.3×5.3×3.5-cm heterotopic thyroid in the posterior mediastinum in a patient with situs inversus totalis
Introduction
Although ectopic thyroid is clinically benign, it is successfully treated with surgical resection. Ectopic thyroid is at risk of malignant transformation and they can cause serious clinical conditions due to severe bleeding or compression of the adjacent vital organs during progressive enlargement (1,2). Thoracotomy has been widely used to remove ectopic thyroid is because this procedure allows for complete tumor resection in a wide surgical field and has low postoperative mortality and morbidity. After the ectopic thyroid is completely removed, the disease can be completely cured without any additional treatments (1,3).
Case report
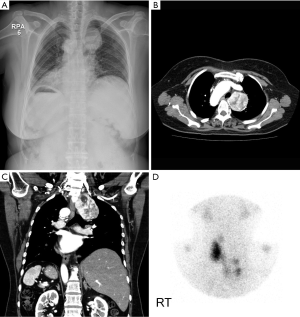
A 62-year-old woman presented at our department due to abnormal findings in chest X-rays. She had undergone a left hemithyroidectomy at a regional hospital 30 years prior to this presentation because of a tiny thyroid nodule in the left thyroid gland associated with hyperthyroidism. Thereafter she was regularly followed up with and her thyroid function test results were normal. At the time of the operation, preoperative evaluation revealed situs inversus totalis without any symptoms and signs. Six years prior to this presentation, the patient underwent brain imaging studies, including MRI, which revealed no abnormal findings. He was taking medications for hyperlipidemia. She was a house wife and had no remarkable family history. She was a non-smoker and a non-drinker. At presentation, her vital signs were stable. Physical examination revealed no specific findings except for a previous thyroidectomy scar. Chest radiographs exhibited situs inversus totalis and a left mediastinal mass. Chest CT revealed a huge well-encapsulated mass in the posterior mediastinum which had no invasion of the trachea, esophagus, or the adjacent lymph nodes suggestive of malignancy. Thyroid scan with radioactive iodine only showed the right thyroid grand alone and a slightly increased iodine uptake in the left mediastinal mass (Figure 1). There were no specific findings in laboratory tests, including the thyroid function test. Esophagogastroscopy revealed no abnormal findings.
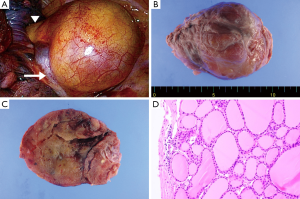
Under general anesthesia, a standard left posterolateral incision was made. The surgical approach was difficult due to the mirror image of the anatomical structures. The mass was bordered by the azygos vein inferiorly, the superior vena cava anteromedially, and the trachea and esophagus medioposteriorly. The mass was removed carefully not to damage the adjacent tissues and blood vessels. There was no direct invasion of the superior vena cava, trachea, or esophagus. The resected mass was well-encapsulated and measured 7.3 cm × 5.3 cm × 3.5 cm. Pathologic examination confirmed benign ectopic thyroid tissue with no invasion of the adjacent lymph nodes (Figure 2). Her dysphagia and atypical chest pain improved. Her hospital course was uneventful and she was discharged from the hospital on the 10th postoperative day. She has been followed up with on a regular basis at our outpatient clinic.
Discussion
Ectopic thyroid is a rare clinical disease entity. The thyroid gland develops at the gestational age of 24 days and starts to migrate at the gestational age of five weeks, during which ectopic thyroid occurs due to abnormal embryological development or thyroglossal duct remnant (4). Thus, ectopic thyroid is usually located on the midline of the anterior neck and inferior to the normal position of the thyroid gland. The most common presentation of the ectopic thyroid is the lingual thyroid which is located along the thyroglossal duct remnant (5).
There have been several reports on unusual locations of ectopic thyroid, such as the axilla, trachea, adrenal gland, and porta hepatis. The most common non-cervical location of ectopic thyroid has been reported to be the thoracic cavity (6). The true primary ectopic thyroid is retrosternal goiter, which is usually located in the anterior mediastinum. However, Madjar et al. (7) reported that 10-15% of all retrosternal goiters were located in the posterior mediastinum. Chin et al. (8) demonstrated that 5 of the 190 patients with goiters had masses in the posterior mediastium on CT scans. Tumors that originate in the posterior mediastinum include neurogenic tumors, Castleman disease, bronchogenic cysts, Bochdalek’s hernia, and mesenchymal tumors. There have been few reports on thyroid tumors arising in the posterior mediastinum. The incidence of such thyroid tumors is relatively low even when primary ectopic goiters and invasion of thyroid carcinomas are included. Though ectopic thyroid rarely develops in the posterior mediastinum, it should be considered in the differential diagnosis of posterior mediastinal tumors (6). Demirhan et al. (3) reported a 62-year-old man who was admitted to the emergency department with atypical chest pain and dysphagia, and was diagnosed as having a posterior mediastinal mass causing esophageal compression. The mass was completely encapsulated and totally localized in the posterior mediastinum as an isolated intrathoracic tumor causing dysphagia, and pathologic sections confirmed the lesion as ectopic thyroid with neither connection with normal thyroid glands nor functional impairment. Karapolat and Bulut (1) reported a 74-year-old Caucasian male with a mass lesion in the right posterior mediastinum, which was successfully resected and confirmed as ectopic thyroid gland with neither connection with normal thyroid glands nor functional impairment. Mace et al. (4) reported an 80-year-old female who presented with an incidental retrosternal mass on magnetic resonance imaging which is consistent with a benign ectopic sequestered thyroid nodule without evidence of malignancy.
True primary ectopic thyroid accounts for less than 1% all goiters, but its accurate incidence has not yet been reported. There have been numerous mechanisms behind the pathogenesis of ectopic thyroid, but the precise mechanisms remain to be elucidated. To the best of our knowledge, this is the first case of a patient with situs inversus totalis who had ectopic thyroid in the posterior mediastinum. The relationship between ectopic thyroid and situs inversus totalis is unclear. Ectopic posterior mediastinal thyroid is generally known to be benign. Thus, it should be distinguished from metastatic lymph nodes of well-differentiated thyroid carcinoma. Most patients with ectopic thyroid show clinical features of euthyroid, while a few patients show clinical features of hyperthyroidism. Thyroid function tests are very useful for preoperative diagnoses as well as postoperative follow-ups and thyroid scan with radioactive iodine is also helpful in making a correct diagnosis and evaluating clinical patterns. However, since in some cases, thyroid scan with radioactive iodine shows negative findings, this diagnostic modality cannot completely rule out ectopic thyroid. Chest computed tomography is the most useful radiological diagnostic modality and provides important information for a safe surgical approach. Although some investigators have demonstrated that magnetic resonance imaging is helpful in the differential diagnosis and treatment of ectopic thyroid, there is still controversy regarding this issue (1,3). Most patients with ectopic thyroid are asymptomatic, whereas a few patients have clinical symptoms and signs due to compression of the adjacent organs, such as cough, dyspnea, wheezing, dysphagia, and obstruction of the superior vena cava (1). It seems likely that our patient complained of intermittent dysphagia due to compression of the adjacent organ by the enlarged ectopic thyroid.
Although ectopic thyroid is clinically benign, it is successfully treated with surgical resection Ectopic thyroid is at risk of malignant transformation and they can cause serious clinical conditions due to severe bleeding or compression of the adjacent vital organs during progressive enlargement (1,2). Thoracotomy has been widely used to remove ectopic thyroid is because this procedure allows for complete tumor resection in a wide surgical field and has low postoperative mortality and morbidity. After the ectopic thyroid is completely removed, the disease can be completely cured without any additional treatments (1,3).
Acknowledgements
This work was supported by Konkuk University.
Disclosure: The authors declare no conflict of interest.
References
- Karapolat S, Bulut I. Ectopic posterior mediastinal thyroid: a case report. Cases J 2008;1:53. [PubMed]
- Shah BC, Ravichand CS, Juluri S, et al. Ectopic thyroid cancer. Ann Thorac Cardiovasc Surg 2007;13:122-4. [PubMed]
- Demirhan R, Onan B, Oz K, et al. Posterior mediastinal ectopic thyroid: an unusual cause for dysphagia. Ann Thorac Surg 2009;88:656-9. [PubMed]
- Mace AD, Taghi A, Khalil S, et al. Ectopic sequestered thyroid tissue: an unusual cause of a mediastinal mass. ISRN Surg 2011;2011:313626.
- Larochelle D, Arcand P, Belzile M, et al. Ectopic thyroid tissue--a review of the literature. J Otolaryngol 1979;8:523-30. [PubMed]
- Vadasz P, Kotsis L. Surgical aspects of 175 mediastinal goiters. Eur J Cardiothorac Surg 1998;14:393-7. [PubMed]
- Madjar S, Weissberg D. Retrosternal goiter. Chest 1995;108:78-82. [PubMed]
- Chin SC, Rice H, Som PM. Spread of goiters outside the thyroid bed: a review of 190 cases and an analysis of the incidence of the various extensions. Arch Otolaryngol Head Neck Surg 2003;129:1198-202. [PubMed]


