Effectiveness and safety of diagnostic flexi-rigid thoracoscopy in differentiating exudative pleural effusion of unknown etiology: a retrospective study of 215 patients
Introduction
Pleural effusion, a condition commonly encountered in respiratory medicine, is classified as transudative or exudative based on criteria established by Light (1,2). Among the most common causes of exudative pleural effusion are tuberculosis, malignant tumors, parapneumonic effusion, and connective tissue disease. The accurate diagnosis of pleural effusion is challenging because even after thoracocentesis and/or closed pleural biopsy, 25-40% of pleural effusions remain undiagnosed (3). Although the accuracy of Light’s criteria to identify pleural exudates is very high, a recent review has described a relatively lower specificity when applying these criteria (4). Recent reports have shown that after a series of tests including chest CT, bronchoscopy, experimental examination of hydrothorax and exfoliative cytology, about 1/4 of exudative pleural effusions were not diagnosed (5,6). Previously, such patients were given antituberculosis treatment, and malignant pleural effusion was considered if there was no response to the initial therapy. However, accurate diagnosis required thoracotomy and video-assisted thoracoscopic surgery. General anesthesia, significant trauma, high cost and high risk are major disadvantages of these procedures. Medical thoracoscopy is now increasingly used in the diagnosis and treatment of pleural effusions following the availability of video-assisted thoracoscopic equipment and improvements in the clinical skills of respiratory physicians. Both rigid and flexi-rigid thoracoscopy have been shown effective in the diagnosis of pleural diseases.
Attempts to obtain a diagnosis for pleural effusion usually involve fluid aspiration and analysis and closed-needle biopsy specimens of the pleura. However, the results of such procedures are often not satisfactory (7). Flexi-rigid thoracoscopy has been available for clinical use in China since 2004. This relatively new technique has the advantages of requiring only local anaesthesia, ease of operation, low cost, wide vision, reduced complication rates and high patient tolerability. It has been used mainly for the diagnosis and treatment of pleural effusions that could be confirmed by the conventional methods (8,9). In particular, it has a high diagnostic value for malignant pleural effusions (10,11), and pleurodesis can be performed directly for malignant pleural effusions with increasing pleural fluid.
The aim of this retrospective study of 215 patients was to evaluate the effectiveness and safety of diagnostic flexi-rigid thoracoscopy in differentiating exudative pleural effusions of unknown etiology.
Materials and methods
Patients
A total of 215 patients with undiagnosed exudative pleural effusion were consecutively recruited in the Department of Respiratory Medicine, the First College of Clinical Medical Science of China Three Gorges University and Yichang Central People’s Hospital, China, between January 2011 and February 2013. The cohort included 118 males and 97 females, with a mean age of 46.5 years (range, 16-80 years). The etiology had not been determined in any of the patients after a series of evaluations including chest CT scan, fiber bronchoscopy, laboratory examination of pleural effusions and exfoliative cytology. Blind percutaneous pleural biopsy was excluded because of its low diagnostic rate. Light’s criteria and cholesterol determination in pleural fluid were used to exclude transudative pleural effusions. Histopathology of caseating granulomas or microbiology of acid-fast bacillus was used to make a diagnosis of tuberculous pleurisy. Postoperative patients with unknown etiology were registered and were entered into a strict follow-up system.
Flexi-rigid thoracoscope and ancillary equipment
The flexi-rigid thoracoscope that was used (LTF-240, Olympus Corporation, Tokyo, Japan) has a rigid shaft and a flexible tip. Its accessories and ancillary equipment include a light source (EVIS-240) and TV system, a flexible trocar, biopsy forceps, closed thoracic drainage tubes and bottles.
Preoperative preparation
Preoperative examinations included routine complete blood count, blood type, coagulation function, hepatic and renal function and an electrocardiogram, which, combined with the patient’s general condition, assessed the feasibility of the procedure. All patients had a Karnofsky performance status (KPS) >70, and patients with surgical contraindications such as severe cardiopulmonary diseases were excluded. Emergency measures such as endotracheal intubation and cardiopulmonary resuscitation were prepared. Large amounts of free pleural effusion could be directly located with ultrasound; however, patients with small amounts of pleural effusion (78 cases) required a preoperative artificial pneumothorax. The edge of the capsule was chosen for tube insertion in patients with an encapsulated pleural effusion.
Thoracoscopy and postoperative evaluation
The patients were positioned on their uninjured side and were supplied with oxygen through a nasal catheter. Preoperative treatment included intramuscular injection of diazepam (10 mg) and tramadol (0.1). Insertion of the thoracoscope through the chest wall was performed under local anesthesia using 10 mL of 2% lidocaine. A 1-1.5 cm transverse skin incision for tube insertion was made with a scalpel parallel to the rib along the 5-7th intercostal space, between the anterior axillary line and midaxillary line. Blunt dissection proceeded from superficial fasciae to parietal pleura to expose the pleural cavity. Then, a flexible trocar was placed, and the flexi-rigid thoracoscope was inserted into the pleural cavity. The visceral, parietal and diaphragmatic pleura around the incision were inspected in a medial, anterior, superior, posterior, lateral and inferior order. As much pleural fluid as possible was aspirated, and a pleural biopsy was performed. Any fibrous adhesions or pus mass, if present, was removed using biopsy forceps and a freezing probe. If necessary, normal saline and iodophor were used to wash the pleural cavity. At the end of the procedure, a closed thoracic drainage tube was inserted and attached to a closed drainage bottle. The optimal time of extubation was determined according to the amount of fluid in the drainage bottle. Intraoperative blood pressure, respiration, heart rate, cardiac rhythm and blood oxygen saturation was monitored. Postoperative treatments included ECG monitoring, oxygen therapy and wound care. The tolerance to operation, surgical complications and postoperative pathological diagnosis rate were recorded precisely.
Results
Preoperative diagnoses included 105 cases of right pleural effusion, 62 cases of left pleural effusion and 48 cases of bilateral pleural effusions. Chest radiography and ultrasound demonstrated large amounts of pleural effusion in 74 patients and encapsulated pleural effusion in 45 patients. Bloody pleural fluid was found in 117 of these patients, yellow or grass-green pleural fluid in 97, and chocolate-colored, turbid pleural fluid in one patient. Thoracoscopy and biopsy was successfully performed in all of the patients, including 38 patients who had pleural adhesions. There were no severe complications and the operative time averaged 35 min.
Thoracoscopic findings
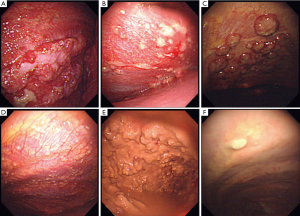
Early tuberculous pleuritis was characterized by hyperemic, edematous pleura with uniformly distributed white nodules that were frequently seen in the costophrenic sinus. The pleura become adhesive, encapsulated and fibrinous at later stages. The appearance of metastatic pleural tumors of the parietal pleura or diaphragm varied from a diffuse infiltration to off-white nodules. Angiogenesis was observed around the lesions, some of which were shaped like a cauliflower. A single lesion was quite rare. Malignant pleural mesothelioma was semitransparent, yellowish white or claret-colored, smooth, sessile, with a ‘cluster of grapes’ appearance like multiple granulomas. The tumors were occasionally widespread along the pleural surface, with varied thickness, unclear boundaries and diffuse thickening. One patient with tuberculosis complicated by pyothorax presented with extensive, irregular, festering, pale nodules. A single off-white nodule was observed in a patient with pulmonary schistosomiasis. Thoracoscopy revealed glandular tissue hyperplasia on the costophrenic angle in a patient with lymphoma (Figure 1).
Pathological results of pleural biopsy
All of the patients were successfully taken a biopsy. There were 97 patients with malignant tumors. Adenocarcinoma occurred in 43 of the patients, squamous carcinoma in 15, small cell carcinoma in 19, malignant pleural mesothelioma in 16, malignant lymphoma in one. Atypical malignant cells unable to been accurately classified were seen in three patients. A total of 91 patients were diagnosed with tuberculous pleuritis by histopathology or microbiology. Chronic inflammation and fibrinous pleuritis of histopathology were considered as negative findings of semirigid thoracoscopy, which was found in 25 patients and they had regular follow-ups. Eleven of them were highly suspected and treated by antituberculosis therapy. One patient was pathologically confirmed to have tuberculosis complicated by empyema by a pleural decortication. Pulmonary schistosomiasis occurred in one patient, who had a positive reaction on a Paragonimus antigen intradermal test. A definitive diagnosis could not be made in 25 patients who had regular follow-ups. The total diagnosis rate was 88.4% (190/215).
Complications
All the patients had stable vital signs intraoperatively. Minimal to moderate hemorrhage observed at the biopsy site did not require special treatment. Subcutaneous emphysema occurred in ten cases postoperatively. The patients had complete remission following conservative treatments such as administration of oxygen. Six patients without preoperative fever had an elevated temperature of around 37.5-38.5 °C postoperatively. The body temperature of these patients returned to normal within five days after symptomatic treatments. There were no complications such as aeroembolism, pleural reaction or wound infection.
Discussion
Our retrospective analysis showed that the diagnostic rate of exudative pleural effusion with unknown etiology using flexi-rigid thoracoscopy was approximate to 90%. All the patients including the oldest one at 80 years of age were able to undergo thoracoscopic surgery and pleural biopsy. This confirmed the safety of the operation and its tolerance by patients. There were few surgical complications; ten cases of subcutaneous emphysema and six cases of postoperative fever among 215 patients. All were alleviated through symptomatic treatments. There was strong relationship between thoracoscopic appearance and primary disease or tumor classification. In this study, 91 patients (42.3%) were diagnosed with tuberculous pleuritis, and another 11 patients were considered to have tuberculosis because of their clinical manifestations although chronic inflammation was observed pathologically. The ADA values in tuberculous pleural effusions were 34-86 U/L (median: 52 U/L). Tuberculous pleuritis occurred in patients of all ages, most of which lacked the typical clinical symptoms of tuberculosis. The thoracoscopic characteristics of tuberculous pleuritis appeared as small nodules or wheat grain-like nodules with extensively fibrotic adhesions. Some patients at an early stage of progression had the appearance of inflammation such as hyperaemia and edema or a diffuse, single nodule could be observed. Thoracoscopic decortication can be applied directly to fibrotic tissue to avoid pleural adhesion and hypertrophy. Pulmonary schistosomiasis occurred in one patient, in whom a single white nodule was found on the pleura microscopically. Thus, careful observation is required for surgeons to find suspicious lesions and perform multi-site and multi-point biopsies.
About half of these patients (97/215, 45.1%) with pleural effusions of unknown etiology were finally diagnosed with malignant pleural effusions, in which lung and breast cancers were the most frequent. The lower part of pleural cavity (e.g., the dome of the diaphragm and Harrison’s groove) was often involved in malignant pleural metastasis. Macroscopically, tumors had multiple nodules, and were often shaped like a cauliflower or a bunch of grapes. Close attention should be paid when performing biopsies because of the possibility of angiogenesis surrounding lesions. Clinically, it was difficult to distinguish malignant pleural mesothelioma and metastatic adenocarcinoma. Thus, microscopic characteristics and immunohistochemistry were used to identify them. Thoracoscopy had a high diagnostic rate for malignant pleural effusions, and the small number of false negative results usually occurred in cases of serious pleural adhesions, early malignant mesothelioma and with inexperienced operators. The latest fluorescence-assisted thoracoscopy, when used in diagnosis and clinical staging of malignant pleural disease, was shown to be superior traditional thoracoscopy for detecting micrometastasis lesions that were invisible to the naked eye (10). A recent study indicated that the degree of pleural adhesion as seen by thoracoscopy was an important predictor of survival time of patients with malignant pleural effusions (12). There was also a positive correlation between the degree of pleural adhesion and prognosis (13). For repeatedly occurring malignant pleural effusions, pleurodesis was a better choice, with talc as an effective sclerosing agent (14,15). There was no significant difference of effectiveness between spray or perfusion application of talc. However, talc spray had a higher probability of success for malignant pleural effusion induced by primary lung or breast cancer (16,17). Patient tolerance and safety were both acceptable for talc pleurodesis.
The flexi-rigid thoracoscopy has been designed to combine the best features of rigid thoracoscope and flexible bronchoscope with a proximal rigid shaft and a distal flexible tip, and can be maneuvered akin to the flexible bronchoscope. It has good sensitivity, excellent specificity in diagnosis of exudative pleural effusion of undetermined etiology and the capability to treat pleural diseases directly. Compared with rigid thoracoscopy, flexi-rigid thoracoscopy has several benefits like less need for analgesia and sedation, minimal compression over the rib and the underlying neural structures, easier maneuvering and less complications. The disadvantage would be a smaller size of biopsy tissue and the difficulty to obtain tissue from fibrous pleura. Moreover, rigid thoracoscopy scores over flexi-rigid thoracoscopy in adhesiolysis and management of empyemas (18,19). Improved clinical techniques and understanding of the surgical indications and tolerance of patients allow for strict selection criteria and comprehensive preoperative assessment to avoid, or reduce occurrence of serious complications. Combining the guidelines with experience, thoracoscopy can be performed to directly identify the etiology of pleural effusions, of which the most likely are malignant pleural effusions (20). Once diagnosed with malignant pleural effusions, the survival time of patients is limited, with a poor prognosis. Early, standardized treatment could help to improve the quality of life and extend the survival time of such patients (21,22). For patients with tuberculous pleural effusion diagnosed by thoracoscopy, decisive application of corticosteroids, would promote the regression of pleural effusion when antituberculosis treatment was ineffective. Also, changing empiric antituberculosis treatment to antituberculosis treatment after diagnosis was beneficial to the decisive application of corticosteroids, which would promote the regression of pleural effusion when anti-tuberculosis treatment was ineffective. On the other hand, complete aspiration of pleural fluid using flexi-rigid thoracoscopy could reduce the production of fibrotic adhesions and toxic symptoms. Elimination of fibrotic adhesions in the pleural cavity could reduce the occurrence of pleural hypertrophy and chest deformity.
Although the accuracy of Light’s criteria is very high, a decrease in specificity has been noted when applying these criteria. In our study, the concentration of pleural fluid cholesterol >1.55 mmol/L was chosen as an exclusion criterion to improve specificity, and still few transudate pleural effusion cases were probably included in this study (23). Also, for the patients definitively diagnosed with malignant pleural effusions, systemic chemotherapy or targeted therapy was the main choice considering the patient’s tolerance. A small number of patients were given postoperative intrapleural chemotherapy but not talc pleurodesis under thoracoscope, which was considered in our subsequent studies.
Conclusions
Diagnostic flexi-rigid thoracoscopy, with the guidance role for primary disease, has the higher diagnosis rate in differentiating exudative pleural effusion of unknown etiology, and it is worthy to wider clinical use because of its satisfactory effectiveness and safety.
Acknowledgements
This study was supported by a grant from the natural science foundation of Hubei Province (NO: 2012FFB06301), the science and technology research foundation of Yichang City (NO: A12301-12).
Disclosure: The authors declare no conflict of interest.
References
- Hean O, Shang-Miao C, Chien-Ming L, et al. Bedside pleuroscopy in the management of undiagnosed exudative pleural effusion with acute respiratory failure. Anaesth Intensive Care 2013;41:473-5. [PubMed]
- Kim JJ, Sa YJ, Cho DG, et al. Intractable hiccup accompanying pleural effusion: reversible clipping of an intrathoracic phrenic nerve. Surg Laparosc Endosc Percutan Tech 2013;23:357-9. [PubMed]
- Prabhu VG, Narasimhan R. The role of pleuroscopy in undiagnosed exudative pleural effusion. Lung India 2012;29:128-30. [PubMed]
- Porcel JM. Identifying transudates misclassified by Light’s criteria. Curr Opin Pulm Med 2013;19:362-7. [PubMed]
- Harvey-Taylor J, Zhang Y, Kuderer V, et al. Diagnosis of systemic amyloidosis and amyloidosis mediated cardiomyopathy by VATS pleural biopsy for chronic pleural effusion. J Thorac Dis 2013;5:E112-4. [PubMed]
- Li J, Bao QL, Wang Y, et al. Diagnostic value of the FHIT and p16 mRNA loss and the K-ras gene mutation in pleural fluids for malignant pleural effusion. Cancer Biomark 2013;13:49-58. [PubMed]
- Atta MA, Hela SA, Hatata IA, et al. Fiberoptic thoracoscopy in management of exudative pleural effusion. Egyptian Journal of Chest Diseases and Tuberculosis 2012;61:405-11.
- Michaud G, Berkowitz DM, Ernst A. Pleuroscopy for diagnosis and therapy for pleural effusions. Chest 2010;138:1242-6. [PubMed]
- Brims FJ, Arif M, Chauhan AJ. Outcomes and complications following medical thoracoscopy. Clin Respir J 2012;6:144-9. [PubMed]
- Casal RF, Eapen GA, Morice RC, et al. Medical thoracoscopy. Curr Opin Pulm Med 2009;15:313-20. [PubMed]
- Ishida A, Nakamura M, Miyazawa T, et al. Novel approach for talc pleurodesis by dedicated catheter through flexi-rigid thoracoscope under local anesthesia. Interact Cardiovasc Thorac Surg 2011;12:667-70. [PubMed]
- Pikin O, Filonenko E, Mironenko D, et al. Fluorescence thoracoscopy in the detection of pleural malignancy. Eur J Cardiothorac Surg 2012;41:649-52. [PubMed]
- Mouchantaf FG, Villanueva AG. The long-term prognosis of patients with the diagnosis of nonmalignant pleural effusions after pleuroscopy. J Bronchology Interv Pulmonol 2009;16:25-7. [PubMed]
- Inoue T, Ishida A, Nakamura M, et al. Talc pleurodesis for the management of malignant pleural effusions in Japan. Intern Med 2013;52:1173-6. [PubMed]
- Srour N, Amjadi K, Forster A, et al. Management of malignant pleural effusions with indwelling pleural catheters or talc pleurodesis. Can Respir J 2013;20:106-10. [PubMed]
- Jimenez CA, Mhatre AD, Martinez CH, et al. Use of an indwelling pleural catheter for the management of recurrent chylothorax in patients with cancer. Chest 2007;132:1584-90. [PubMed]
- Basso SM, Mazza F, Marzano B, et al. Improved quality of life in patients with malignant pleural effusion following videoassisted thoracoscopic talc pleurodesis. Preliminary results. Anticancer Res 2012;32:5131-4. [PubMed]
- Dhooria S, Singh N, Aggarwal AN, et al. A randomized trial comparing the diagnostic yield of rigid and semirigid thoracoscopy in undiagnosed pleural effusions. Respir Care 2014;59:756-64. [PubMed]
- Agarwal R, Aggarwal AN, Gupta D. Diagnostic accuracy and safety of semirigid thoracoscopy in exudative pleural effusions: a meta-analysis. Chest 2013;144:1857-67. [PubMed]
- Stefani A, Natali P, Casali C, et al. Talc poudrage versus talc slurry in the treatment of malignant pleural effusion. A prospective comparative study. Eur J Cardiothorac Surg 2006;30:827-32. [PubMed]
- Roberts ME, Neville E, Berrisford RG, et al. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii32-40. [PubMed]
- Kastelik JA. Management of malignant pleural effusion. Lung 2013;191:165-75. [PubMed]
- Hamal AB, Yogi KN, Bam N, et al. Pleural fluid cholesterol in differentiating exudative and transudative pleural effusion. Pulm Med 2013;2013:135036.


