European Respiratory Society International Congress best abstract preview from the allied respiratory professionals from assembly 9
Introduction
The 28th European Respiratory Society (ERS) International Congress [2018] in Paris features interesting research findings within the allied respiratory professional assembly (assembly 9). Excellent and high ranked abstracts were selected for this year’s ERS International Congress preview of assembly 9 and are put in the spotlights. A summary of the best three abstracts of every group, i.e., lung function technologists, physiotherapists and nurses, within assembly 9 is presented. Session, timing and location of the presentation of the abstract at this year’s ERS International Congress is indicated in squared brackets following the authors’ name.
Group 9.1: lung function technologists
Lung clearance index versus spirometry in children with cystic fibrosis taking lumacaftor/ivacaftor
There are two common pulmonary function tests to measure the lung function of the paediatric population who live with cystic fibrosis (CF); spirometry and multiple breath washout (MBW). MBW is able to present multiple different measures of lung efficiency and disease severity, the lung clearance index (LCI) has become the most used measure derived from MBW (1). The MBW tends to be a preferable measure for the paediatric CF population; tidal volume breathing makes it feasible to perform, the gasses inhaled are inert, and the gasses used do not participate in any gas exchange within the lungs (2). LCI has been shown in studies to be a more sensitive measurement for paediatric CF than spirometry alone (3). The data being presented by Mulligan et al. (Sunday 16 September, 08:30–10:30 AM, Room 7.3P) is consistent with previous studies in sensitivity changes between spirometry and LCI, as seen pre and post lumacaftor/ivacaftor delivery (Table 1).
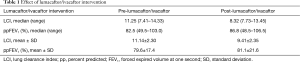
Full table
There is a large utility for LCI in the paediatric CF population when combined with spirometry (4). Clinically LCI is important to assess the need for treatment, the severity of disease, and outcomes of therapies. In a research context, LCI should be included in study design for safety, especially in research that involves CF populations. While the importance of forced expiratory volume at one second (FEV1) should not be dismissed, LCI is more sensitive and helps to complete the diagnostic picture.
Development and pilot evaluation of a quality grading system for paediatric spirometry
ATS/ERS has established standard spirometry guidelines for adult populations for years now, but paediatric patients present different challenges that have made this form of standardization slower to progress (5). Understanding the need to start this process, Perrem et al. (Tuesday 18 September, 10:45 AM –12:45 PM, Room 7.3B) have set out to independently begin creating a model to grade paediatric spirometry; forced vital capacity (FVC) and FEV1.
The creation of a standard grading system is needed and important for the paediatric population. We know this already increases the quality and consistency of testing individually and between technologist, laboratories, and equipment manufacturers (6). Clinically, having standards to adhere to may have a direct impact on the quality interpretation. Without standards to address acceptability and repeatability before interpretation, quality, accuracy, and precision are sacrificed. The same impact should be simulated in research; quality and standardization of testing is paramount to facilitate a consistent evaluation of subject data. Criteria was generated after careful literature review in addition to expert opinion, FEV1 and FVC were both graded. Perrem et al. were able to maintain a high level of repeatability, acceptability, and agreement (91% for FEV1 and 81% for FVC) in review between pulmonologist, respiratory scientists, and technologists. It is important to note that if disagreement existed between reviewers that the most experienced technologist was used as the “gold standard”. This is a very exciting start for a paediatric spirometry quality grading system and standardization, further research should be encouraged to help continue this important development.
The impact of a new reference value set for diffusing capacity for patients with idiopathic pulmonary fibrosis
The Global Lung Function Initiative (GLI) has created new reference values (7). The change of reference values from the 1993 coal reference values (8) to the GLI reference values cannot be taken lightly, as this impacts interpretation of new results and comparison to historical values. Wapenaar-De Korver et al. (Tuesday 18 September, 10:45 AM –12.45 PM, Room 7.3B) have taken an important step for us to understand how this change can impact TLCO interpretation and research inclusion in idiopathic pulmonary fibrosis (IPF) patients. GLI reference values for TLCO are new and aim to provide a better reference set to be used in clinical practice, with data inclusion from 19 centres across 14 countries it seems that there is an all-age reference set (7). Lung function is a critical part of evaluating the respiratory system, thus having a standard set of reference values will aid in diagnosis of disease and health. Results show a slight increase in TLCO across 145 patients, based on using the GLI reference values for TLCO the researchers noted 96 patients would be eligible using European Community for Steel and Coal (ECSC) reference values and 104 using GLI. While slight, the increase should be noted in both clinical and research environments. Clinically pulmonary groups should be careful not to make decisions on small improvements for the IPF patient, a change in reference value can be the only reason an improvement is seen versus an improvement in condition. Special care should be taken to communicate these important changes to physician groups to avoid miss interpretation. IPF has no current cure, creating opportunity for research and inclusion. When selecting reference values researchers should take note of the slight potential increase in inclusion if a DLCO ≥30% is used as criteria. While a slight increase in patients may be seen as small in a pharmaceutical study, it may actually be a very significant improvement when considering the severity and cost of researching new treatments for IPF.
Group 9.2: physiotherapists
Effects of a home-based rehabilitation programme in patients at active treatment for inoperable lung cancer
Lung cancer is among the most prevalent cancers and a major cause of cancer mortality worldwide (9). Non-small cell lung cancer (NSCLC) accounts for 80% of all lung cancers (10) and due to a lack of early specific symptoms, patients are often diagnosed at an advanced stage and present with inoperable disease (11). Therefore, prolonging life and/or improving health-related quality of life (HRQoL) of these patients are the main goals of cancer treatment. Exercise interventions have been shown to prevent deterioration in physical status, improve exercise capacity and muscle strength, reduce fatigue and enhance HRQoL in patients with advanced cancer (12). In advanced NSCLC, there is still a limited number of randomised controlled trials (RCT) assessing the impact of exercise interventions and most of them are hospital-based (12). Although the ideal setting to implement exercise interventions in NSCLC is still under debate (13), home-based interventions have the potential to reduce patient burden associated with travel, improve patients’ adherence to the intervention and promote long-term behaviour change (14). Edbrooke et al. (Wednesday 19 September, 08:30–10:30 AM, Room 7.3O) conducted a multicentre RCT which investigated the efficacy of a home-based multidisciplinary exercise and supportive care intervention versus standard care in patients starting active treatment for inoperable NSCLC. Patients in the experimental group (EG, n=45) received 8 weeks of aerobic and resistance exercise, behaviour change and symptom management telephone support, in addition to standard care. The control group (CG, n=47) received standard care only which did not include any form of exercise training. The study protocol is described in detail elsewhere (15). Patients were assessed at 9 weeks (post-intervention) and 6 months (follow-up). No significant between-group differences were found in physical function outcomes [6MWD (primary outcome), muscle strength and PA], which suggests that a home-based exercise intervention does not provide additional benefit to physical status compared to usual care in patients starting active treatment for inoperable NSCLC. While this is a disappointing finding, significant improvements were found in HRQoL (P=0.005), symptom severity (P=0.001) and exercise motivation (P=0.04) in the EG at 6-month follow-up. The fact that the intervention led to a decrease in symptom severity and an increase in HRQoL is an important outcome, since the usual pattern seen in patients living with advanced cancer is an increase in symptom burden which greatly interferes with patients’ HRQoL (11). Moreover, exercise motivation was significantly improved in the EG at follow-up. High exercise motivation was recently identified as one of the most prominent predictors of adherence to exercise-based interventions in patients with cancer (14). This finding suggests that the home-based exercise intervention implemented by Edbrooke et al. may help patients being more physically active in the long-term.
Impact of a web-based physical activity enhancing intervention during pulmonary rehabilitation in COPD
Physical activity, which includes physical exercise, is reduced in patients with chronic obstructive pulmonary disease (COPD) when compared to healthy individuals (16). Low levels of PA have been associated with poor outcomes, including increased risk of exacerbations (17), hospital admissions and mortality (18). Thus, increasing patients’ PA levels has been identified as a priority for researchers and clinicians worldwide (19,20). Pulmonary rehabilitation (PR) is the cornerstone of COPD management with worldwide known benefits on patients’ exercise capacity and HRQoL (21). As such, and because it includes components of exercise training, education and behaviour change, it would be expected to have a positive effect on patients’ PA behaviour (19,21). However, studies assessing the impact of PR on PA have shown that an increase in exercise capacity does not necessarily translate into meaningful improvements in patients’ PA (22). Alternative methods to produce PA behaviour change are therefore needed. A recent systematic review on interventions aiming at increasing PA in patients with COPD has found that interventions including PA counselling and coaching, especially if combined with exercise training, are promising and should be further explored (22). Mantoani et al. (Monday 17 September, 08:30–10:30 AM, Terminal 7) investigated the impact of a web-based PA enhancing intervention on PA levels of patients attending a 12-week PR programme. Patients with COPD were randomised to either receive a PA enhancing intervention during PR (experimental group, EG=22) or PR alone (control group, CG=22). The PA enhancing intervention consisted of a web-based PA human coaching with weekly individualised targets and objective feedback on patients’ PA measured by an activity monitor (TracmorD, Philips). Patients were assessed at baseline and after 3 months. Findings suggest that the web-based PA enhancing intervention is effective in enhancing patients’ PA levels during PR when compared to PR alone (1,251±2,408 vs. −410±1,118 steps/day, respectively). The authors also found significant improvements (favouring the EG) in patients’ exercise capacity, quadriceps muscle strength, symptoms of anxiety and depression, and HRQoL, which further supports the idea that a more active lifestyle may translate into health benefits for these patients. These are exciting findings which may guide future interventions on PA promotion in COPD. Since information and communication technologies are embedded in people’s everyday lives, the use of e-health interventions (e.g., websites) for PA promotion offer the opportunity to deliver personalised coaching to patients with limited healthcare resource use, facilitate self-management and reach a large proportion of people thereby reducing access disparities (23). Further research with follow-up assessments is needed to support these findings and assess the long-term impact of this web-based PA enhancing intervention in COPD, since maintenance of PA behaviour is a major challenge (24).
Predictors of patients’ completion or response to a 12-month physical activity intervention in COPD
Previous research has shown that, as a complex behaviour, PA is influenced by a combination of factors including individual characteristics, disease-specific factors, psychosocial and environmental factors (19,20,25,26), that may act as barriers or facilitators. However, the extent to which these factors determine long-term maintenance of PA behaviour [which may be different from those involved in behaviour initiation (27)] remains understudied. The study of Koreny et al. (Monday 17 September, 08:30–10:30 AM, Terminal 7) aimed to identify baseline predictors of 12-month completion or response to a PA enhancing intervention in patients with COPD, using logistic multivariable regressions. The authors identified ‘completers’ (i.e., patients attending the final visit) and ‘responders’ (i.e., patients who increased ≥600 steps/day after 12 months when compared to baseline, measured by an accelerometer) of the intervention arm of the Urban Training study (NCT01897298) and investigated the factors that predicted patients’ completion or response to the intervention. The authors found that ‘completers’ (n=132/202) were more likely to live with a partner, live in less disadvantaged neighbourhoods and be already physically active at baseline (≥10,000 steps/day) than ‘non-completers’. From those who completed the study, 36% (n=47) were classified as ‘responders’. The odds of being a ‘responder’ were 2.7 times higher in patients currently working and those with an endocrino-metabolic disease than in ‘non-responders’. These findings suggest that although the decline in patients’ PA levels over time can be determined, in part, by COPD-related factors [e.g., exercise capacity (28)], they do not seem to play a role in maintaining PA behaviour during a 12-month intervention. Instead, factors related to patients’ living context and comorbidities may be associated with long-term maintenance of active lifestyles. It is important to note that, despite the factors identified in the study of Koreny et al. may be regarded as nonmodifiable, they could be used to identify patients with low probability of engaging in and/or maintaining PA behaviour and develop additional strategies to reinforce this behaviour (24). Given the public health importance of promoting the adoption and maintenance of PA by patients with COPD, further research is needed to confirm these findings and identify other factors that may influence patients’ PA behaviour in the long-term.
Group 9.3: nurses
Effectiveness of a hand-held fan for managing dyspnoea in patients with interstitial lung disease
Interstitial lung disease (ILD) is a diverse group of diseases that cause fibrosis or inflammation of the pulmonary parenchyma. Treatment and prognosis of ILD typically depends on the underlying ILD subtype, highlighting the importance of accurate classification and diagnosis (29). Breathlessness is a debilitating feature of ILD (30). Patients with chronic pulmonary disease are often limited in their activities by respiratory discomfort. Reductions in functional status, quality of life, and disability are frequent consequences of this symptom. Dyspnoea is a term used to characterize a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity. The experience derives from interactions among multiple physiological, psychological, social, and environmental factors, and may induce secondary physiological and behavioural responses (31). Research from Galbraith et al. suggests that a hand-held fan that generates airflow over the face can reduce the sensation of breathlessness in patients with advanced respiratory diseases (30). The movement of cool air with a fan has been observed clinically to reduce dyspnoea in respiratory patients. Stimulation of mechanoreceptors of the face or a decrease in the temperature of the facial skin, both of which are mediated through the trigeminal nerve, may alter afferent feedback to the brain and modify the perception of dyspnoea (32). Data from Cassidy et al. (Monday 17 September, 8.30–10.30 AM, Room 7.3J) confirms previous findings. A hand-held fan was provided to 30 patients, mean age 68 years, median time from diagnosis was 4 years and feedback was given via a 4-point Likert-scale questionnaire to rate the frequency of their breathlessness during activities of daily living. All patients agreed/strongly agreed that the fan was effective (100%) and easy-to-use (96.2%), helped improve breathlessness (92%) and relaxation (78.3%), and enabled them to concentrate more on their breathing (91.3%). The authors concluded that healthcare professionals should consider hand-held fans as a practical non-pharmacological option for the management of dyspnoea in ILD patients. From experience in clinical practice, chronic pulmonary patients experiencing an exacerbation often have the need to open windows and for a consistent flow of air in the room. At their homes, patients often use a hand-held fan, ventilation or air conditioner to self-manage their dyspnoea. Breathlessness, however, impedes the performance of daily activities and patients struggle with self-preservation. Instinctively, without suggestion of health care professionals patients use this kind of methods in management of dyspnoea.
The development of an instrument to assess the needs of people with COPD: a Delphi study
The complexity of COPD can negatively impact the lives of people and compromises their capacity to take care of their needs. Unmet needs can lead to significant morbidity, unpleasant emotional experiences and a poor quality of life (33). Self-management educational interventions are carried out to improve the level of respiratory function and therapeutic adherence, and to reduce the occurrence of exacerbations (34). The complexity of COPD, which results from differences in the evolution of the disease, the various therapeutic approaches, frequent exacerbations, the lack of home-based management of symptoms, and reduced social and family relationships, can have a negative impact on the everyday lives of people with the disease and compromise their capacity to take care of their needs (35). These needs can be defined as being the condition of a person being in demand of some necessary, desirable or valuable action or support to achieve optimal well-being (36). The identification of these needs through qualitative evidence can facilitate the creation of interventions aimed at identifying specific needs and personalising patient care (33). Clari et al. (Monday 17 September, 8.30–10.30 AM, Room 7.3J) pointed out that COPD patient-centred self-management interventions firstly have to identify patients’ needs to effectively support the patients to positively adapt their health behaviours and develop skills to manage their disease better. To our knowledge, no tools to measure the needs of people with COPD are present in the literature. The aim was to develop an instrument to assess the needs of people with COPD. Clari et al. used a three-round modified Delphi method to develop an instrument to assess the needs of people with COPD. After three rounds, a consensus was reached on a questionnaire consisting of 25 items distributed across four domains: information needs, needs relating to the symptoms of the disease, needs of family and social support, and needs related to the access to care. The authors concluded that the Needs in COPD Assessment questionnaire could be a useful tool to detect the needs of people with COPD. This tool, which covers a variety of domains, could be an easy to use instrument, but a further study is necessary to validate its psychometric properties before it can be implemented in the clinical context.
Health status among adult asthmatics—a population-based study
Asthma in women is reported to be more severe and associated with higher health care use (37,38). Understanding and using strategies that target this gender-specific difference in disease response and symptom profiles may result in improved asthma-related quality of life and health of asthmatic women (39). However, other factors associated to health have rarely been studied in population-based samples. Data from Stridsman et al. (Monday 17 September, 8.30–10.30 AM, Room 7.3J) determined factors associated with generic health in a population-based adult asthma cohort (the OLIN-studies) in 2012–2014, where n=1,425 subjects were invited to a clinical follow-up. N=1,006 subjects participated, of which n=830 had current asthma. Stridsman et al. described an association between worse physical and mental health in adult asthmatics and female gender, a higher BMI and health care visits due to respiratory symptoms. Eczema was only associated with worse mental health, and increasing age and blood neutrophils ≥5×109/L with physical health. In addition, subjects with allergic asthma seem to have a better physical health than those with non-allergic asthma. An important reason to monitor health status is that it predicts health care utilization among patients who have asthma and for this reason it may be a useful method of identifying patients who are at risk of exacerbation (40,41). The results of the present study indeed confirm that female gender is associated with worse asthma control and health status in adult asthmatics. Furthermore, to improve the patient’s health status and prognosis BMI and health care visits due to respiratory symptoms in the last 12 months should also be taken into consideration. The latter factors should be included in clinical assessment of health status. In assessment of mental health consider the presence of eczema and in physical health increasing age and blood neutrophils ≥5×109/L.
Acknowledgements
Funding: The research of FWO Aspirant Jana De Brandt is sponsored by FWO-grant #11B4718N.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jensen R, Stanojevic S, Gibney K, et al. Multiple breath nitrogen washout: a feasible alternative to mass spectrometry. PLoS One 2013;8. [Crossref] [PubMed]
- Rosenfeld M, Allen J, Arets BH, et al. An official American Thoracic Society workshop report: optimal lung function tests for monitoring cystic fibrosis, bronchopulmonary dysplasia, and recurrent wheezing in children less than 6 years of age. Ann Am Thorac Soc 2013;10:S1-11. [Crossref] [PubMed]
- Kraemer R, Blum A, Schibler A, et al. Ventilation inhomogeneities in relation to standard lung function in patients with cystic fibrosis. Am J Respir Crit Care Med 2005;171:371-8. [Crossref] [PubMed]
- Hoo AF, Thia LP, Nguyen TT, et al. Lung function is abnormal in 3-month-old infants with cystic fibrosis diagnosed by newborn screening. Thorax 2012;67:874-81. [Crossref] [PubMed]
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-38. [Crossref] [PubMed]
- Culver BH, Graham BL, Coates AL, et al. Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am J Respir Crit Care Med 2017;196:1463-72. [Crossref] [PubMed]
- Stanojevic S, Graham BL, Cooper BG, et al. Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur Respir J 2017;50. [Crossref] [PubMed]
- Cotes JE, Chinn DJ, Quanjer PH, et al. Standardization of the measurement of transfer factor (diffusing capacity). Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993;16:41-52. [Crossref] [PubMed]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Zarogoulidis K, Zarogoulidis P, Darwiche K, et al. Treatment of non-small cell lung cancer (NSCLC). J Thorac Dis 2013;5:S389-96. [PubMed]
- Buzaglo J, Gayer C, Mallick R, et al. Understanding the experience of living with non-small-cell lung cancer (NSCLC): a qualitative study. J Community Support Oncol 2014;12:6-12. [Crossref] [PubMed]
- Dittus KL, Gramling RE, Ades PA. Exercise interventions for individuals with advanced cancer: A systematic review. Prev Med 2017;104:124-32. [Crossref] [PubMed]
- Bade BC, Thomas DD, Scott JB, et al. Increasing physical activity and exercise in lung cancer: reviewing safety, benefits, and application. J Thorac Oncol 2015;10:861-71. [Crossref] [PubMed]
- Ormel HL, Schoot GGF, Sluiter WJ, et al. Predictors of adherence to exercise interventions during and after cancer treatment: A systematic review. Psychooncology 2018;27:713-24. [Crossref] [PubMed]
- Edbrooke L, Aranda S, Granger CL, et al. Benefits of home-based multidisciplinary exercise and supportive care in inoperable non-small cell lung cancer - protocol for a phase II randomised controlled trial. BMC Cancer 2017;17:663. [Crossref] [PubMed]
- Vorrink SN, Kort HS, Troosters T, et al. Level of daily physical activity in individuals with COPD compared with healthy controls. Respir Res 2011;12:33. [Crossref] [PubMed]
- Moy ML, Teylan M, Weston NA, et al. Daily Step Count Predicts Acute Exacerbations in a US Cohort with COPD. PLoS One 2013;8. [Crossref] [PubMed]
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax 2006;61:772-8. [Crossref] [PubMed]
- Nici L, ZuWallack R. They can't bury you while you're still moving: A review of the European Respiratory Society statement on physical activity in chronic obstructive pulmonary disease. Pol Arch Med Wewn 2015;125:771-8. [PubMed]
- Watz H, Pitta F, Rochester CL, et al. An official European Respiratory Society statement on physical activity in COPD. Eur Respir J 2014;44:1521-37. [Crossref] [PubMed]
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13-64. [Crossref] [PubMed]
- Mantoani LC, Rubio N, McKinstry B, et al. Interventions to modify physical activity in patients with COPD: a systematic review. Eur Respir J 2016;48:69-81. [Crossref] [PubMed]
- Kreps GL, Neuhauser L. New directions in eHealth communication: opportunities and challenges. Patient Educ Couns 2010;78:329-36. [Crossref] [PubMed]
- Fjeldsoe B, Neuhaus M, Winkler E, et al. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol 2011;30:99-109. [Crossref] [PubMed]
- Gimeno-Santos E, Frei A, Steurer-Stey C, et al. Determinants and outcomes of physical activity in patients with COPD: a systematic review. Thorax 2014;69:731-9. [Crossref] [PubMed]
- Spruit MA, Pitta F, McAuley E, et al. Pulmonary Rehabilitation and Physical Activity in Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2015;192:924-33. [Crossref] [PubMed]
- van Stralen MM, De Vries H, Mudde AN, et al. Determinants of initiation and maintenance of physical activity among older adults: a literature review. Health Psychol Rev 2009;3:147-207. [Crossref]
- Yu T, Frei A, ter Riet G, et al. Determinants of Physical Activity in Patients with Chronic Obstructive Pulmonary Disease: A 5-Year Prospective Follow-Up Study. Respiration 2016;92:72-9. [Crossref] [PubMed]
- Ryerson CJ, Collard HR. Update on the diagnosis and classification of ILD. Curr Opin Pulm Med 2013;19:453-9. [Crossref] [PubMed]
- Galbraith S, Fagan P, Perkins P, et al. Does the use of a handheld fan improve chronic dyspnea? A randomized, controlled, crossover trial. J Pain Symptom Manage 2010;39:831-8. [Crossref] [PubMed]
- Dyspnea. Mechanisms, assessment, and management: a consensus statement. American Thoracic Society. Am J Respir Crit Care Med 1999;159:321-40. [Crossref] [PubMed]
- Schwartzstein RM, Lahive K, Pope A, et al. Cold facial stimulation reduces breathlessness induced in normal subjects. Am Rev Respir Dis 1987;136:58-61. [Crossref] [PubMed]
- Clari M, Ivziku D, Casciaro R, et al. The Unmet Needs of People with Chronic Obstructive Pulmonary Disease: A Systematic Review of Qualitative Findings. COPD 2018;15:79-88. [Crossref] [PubMed]
- Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014. [PubMed]
- Calverley PM. COPD: what is the unmet need? Br J Pharmacol 2008;155:487-93. [Crossref] [PubMed]
- Sanson-Fisher R, Girgis A, Boyes A, et al. The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer 2000;88:226-37. [Crossref] [PubMed]
- The ENFUMOSA cross-sectional European multicentre study of the clinical phenotype of chronic severe asthma. European Network for Understanding Mechanisms of Severe Asthma. Eur Respir J 2003;22:470-7. [Crossref] [PubMed]
- Serra-Batlles J, Plaza V, Morejon E, et al. Costs of asthma according to the degree of severity. Eur Respir J 1998;12:1322-6. [Crossref] [PubMed]
- Clark NM, Gong ZM, Wang SJ, et al. From the female perspective: Long-term effects on quality of life of a program for women with asthma. Gend Med 2010;7:125-36. [Crossref] [PubMed]
- Eisner MD, Ackerson LM, Chi F, et al. Health-related quality of life and future health care utilization for asthma. Ann Allergy Asthma Immunol 2002;89:46-55. [Crossref] [PubMed]
- Magid DJ, Houry D, Ellis J, et al. Health-related quality of life predicts emergency department utilization for patients with asthma. Ann Emerg Med 2004;43:551-7. [Crossref] [PubMed]


