The problem with sublobar resections
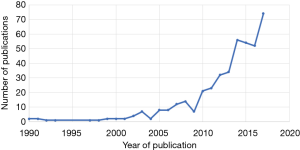
There is a heightened interest in the oncologic efficacy of lobectomy versus sublobar resection in the treatment of early-stage non-small cell lung cancer (NSCLC), as demonstrated by an exponential increase in the number of publications on this topic in recent years (Figure 1). Furthermore, the tremendous interest within the thoracic surgical community was shown at the 1st International Conference on Sublobar Resections for Lung Cancer, held in Paris in January 2018, involving more than 230 thoracic surgeons from 33 countries (1). The importance of this issue and limitations of evidence in the current literature were outlined previously in the journal (2). In brief, historical data from the Lung Cancer Study Group randomized controlled trial has been challenged by results from contemporary observational studies with strict and well-defined patient selection criteria (3,4). With earlier detection of resectable NSCLC through screening programs and increased frailty of an ageing population, more patients are considered for sublobar resections in clinical practice than previously.
To assess the long-term oncological efficacy of sublobar procedures, Subramanian and colleagues conducted a retrospective cohort study using the National Cancer Data Base, to compare lobectomy versus sublobar resection in patients with clinical stage IA NSCLC (5). Selected patients who underwent surgery between 2006 and 2007 were followed through 2012, and registry staff retrospectively obtained additional data on locoregional recurrence information for 5 years following resection. Of the 1,687 patients who met the inclusion criteria, 1,354 underwent lobectomy, 48 underwent segmentectomy, and 285 underwent wedge resection. Patients who underwent segmentectomy and wedge resection were then combined as a sublobar resection group, and matched with patients who underwent lobectomy according to age, gender, race, postcode, income, urban/rural location, academic/non-academic hospital, tumour histology and grade, and comorbidities. Propensity score matching yielded 325 pairs of patients, and demonstrated similar overall survival at 5 years after sublobar resection versus lobectomy (55.6% vs. 61.7%, P=0.561). However, patients who underwent sublobar resections were more likely to have positive margins (6.6% vs. 2.5%, P=0.003) and fewer lymph node sampled (1 vs. 7, P<0.001), with a significantly higher risk of locoregional recurrence (hazard ratio 1.39, 95% confidence interval: 1.04–1.87, P=0.026) and shorter median period to recurrence (17.7 vs. 21.0 months). After excluding patients with positive margins, the 5-year locoregional recurrence was estimated to be 26% for patients who underwent sublobar resection and 20% for those who underwent lobectomy.
The report by Subramanian may be considered as an example of the problems associated with sublobar resections, or the way their data is presented, in the current literature.
- Details about the patient selection process were not presented, and it was not possible to differentiate a healthy patient who could tolerate either a sublobar resection or a lobectomy based on baseline patient characteristics such as pulmonary function or functional status, with a patient who could not tolerate a lobectomy. Previous studies have shown the significantly different overall and disease-free survival outcomes when analysing ‘intentionally selected’ versus ‘compromised’ patients (3).
- Established factors favouring sublobar resections, such as size <2 cm, peripheral location, ground-glass opacification on imaging, favourable adenocarcinoma histopathological subtypes and margins >2 cm were not recorded in the database (3,6).
- Anatomical segmentectomies were categorized together with wedge resections within the sublobar group, without consideration of the significant technical differences between the two procedures, as well as potential differences in their oncological outcome (7). Only 2.8% of patients who met the inclusion criteria underwent a segmentectomy, significantly lower than contemporary series (8).
- No intraoperative details were provided, specifically regarding frozen section analysis of mediastinal and hilar lymph nodes or the assessment of margins. As highlighted by Speicher et al., systematic lymph node evaluation should be mandatory, and its completion may be limited in wedge resections (9). Technically, intraoperative findings of malignancy in intersegmental lymph nodes and/or margins should warrant completion lobectomy (10). It was also not clear how many patients underwent video-assisted thoracoscopic surgery (VATS).
- Due to the lack of adequate systematic lymph node sampling in the sublobar group, it was unclear how many patients were falsely understaged pathologically.
- No follow-up regimens were described, and an unknown number of patients with incomplete recurrence data were excluded from analysis without replacement.
Despite these limitations, it is important not to dismiss the findings by Subramanian, and the authors should be commended on their strong efforts to provide an important snapshot of the ‘real world’ outcomes of sublobar resections. Indeed, the authors stated that up to 70% of all newly diagnosed lung cancer patients in the United States were captured in the National Cancer Data Base, and their results were an accurate reflection of the current clinical practice. Some key findings of the study within the sublobar group warrant further discussion, including the relative high proportion of wedge resections (285/333, 86%), the relatively low number of lymph nodes sampled (median number of lymph nodes, 1) and the relatively high proportion of patients with a positive margin (6.6%). What this implies is that a significant proportion of patients did not undergo the standard of care for eligible surgical candidates, which is video-assisted thoracoscopic anatomical resection with lymph node sampling or dissection (11). It also showed that intraoperative assessment was probably inadequate, compared to rigorous and precise techniques and strategies described previously for sublobar resections (12). Whether these technical procedures were avoided due to patient- or surgeon-related factors remains unclear, and this data may be challenging to elucidate from national databases.
In summary, results from the Subramanian provided a useful benchmark to describe the clinical outcomes of patients who underwent sublobar resections and lobectomies in the United States, but it also clearly demonstrated the limitations of data derived from a national database, whereby important patient selection factors were not captured for analysis. The finding of increased disease recurrence in the heterogenous sublobar resection group must be interpreted with caution. Rather than factors such as ethnicity, residential location and income, clinically relevant radiographic and histopathological prognostic factors must be considered in future studies. Presence of ground-glass opacities, use of preoperative standardized uptake value on positron emission tomography, and more recently, assessment of micropapillary histopathological pattern and the presence of spread through air spaces (STAS) have all been shown to be prognostic for sublobar resections (6,13,14). The crux of the issue may lie with identifying preoperative and intraoperative prognostic factors that can influence the surgeon to decide whether a sublobar resection is oncologically appropriate for an individual patient. There is also a need for surgeons to adequately perform and report sublobar resections, especially anatomical segmentectomies, with appropriate systematic lymph node sampling or dissection, as well as examination of the resection margins intraoperatively.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Gossot D. A conference at the onset of a new era. J Thorac Dis 2018;10:S1131-3. [Crossref] [PubMed]
- Cao C, Tian DH, Wang DR, et al. Sublobar resections-current evidence and future challenges. J Thorac Dis 2017;9:4853-5. [Crossref] [PubMed]
- Cao C, Chandrakumar D, Gupta S, et al. Could less be more?-A systematic review and meta-analysis of sublobar resections versus lobectomy for non-small cell lung cancer according to patient selection. Lung Cancer 2015;89:121-32. [Crossref] [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Subramanian M, McMurry T, Meyers BF, et al. Long-Term Results for Clinical Stage IA Lung Cancer: Comparing Lobectomy and Sublobar Resection. Ann Thorac Surg 2018;106:375-81. [Crossref] [PubMed]
- Tsutani Y, Miyata Y, Nakayama H, et al. Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma: wedge resection or segmentectomy. Chest 2014;145:66-71. [Crossref] [PubMed]
- Koike T, Koike T, Yoshiya K, et al. Risk factor analysis of locoregional recurrence after sublobar resection in patients with clinical stage IA non-small cell lung cancer. J Thorac Cardiovasc Surg 2013;146:372-8. [Crossref] [PubMed]
- Lutz JA, Seguin-Givelet A, Grigoroiu M, et al. Oncological results of full thoracoscopic major pulmonary resections for clinical Stage I non-small-cell lung cancer. Eur J Cardiothorac Surg 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Speicher PJ, Gu L, Gulack BC, et al. Sublobar Resection for Clinical Stage IA Non-small-cell Lung Cancer in the United States. Clin Lung Cancer 2016;17:47-55. [Crossref] [PubMed]
- Gossot D, Lutz JA, Grigoroiu M, et al. Unplanned Procedures During Thoracoscopic Segmentectomies. Ann Thorac Surg 2017;104:1710-7. [Crossref] [PubMed]
- Yan TD, Cao C, D'Amico TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg 2014;45:633-9. [Crossref] [PubMed]
- Gossot D, Zaimi R, Fournel L, et al. Totally thoracoscopic pulmonary anatomic segmentectomies: technical considerations. J Thorac Dis 2013;5 Suppl 3:S200-6. [PubMed]
- Nitadori J, Bograd AJ, Kadota K, et al. Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2cm or smaller. J Natl Cancer Inst 2013;105:1212-20. [Crossref] [PubMed]
- Shiono S, Endo M, Suzuki K, et al. Spread Through Air Spaces Is a Prognostic Factor in Sublobar Resection of Non-Small Cell Lung Cancer. Ann Thorac Surg 2018;106:354-60. [Crossref] [PubMed]


