Comparison of additional minocycline versus iodopovidone pleurodesis during video-assisted thoracoscopic bleb resection for primary spontaneous pneumothorax: a propensity score-matched analysis
Introduction
Video-assisted thoracoscopic surgery (VATS) has been widely performed as a minimally invasive surgical approach for the treatment of primary spontaneous pneumothorax (PSP) (1). However, bleb resection through VATS has been known to be associated with higher postoperative recurrence rates, ranging from 5.9% to 24.5% (2,3), than those for thoracotomy (4,5). A higher chance of missed leaking blebs or a less intense pleural inflammatory reaction by the VATS procedure has been suggested as reasons for this phenomenon (6).
To reduce the recurrence rate through enhancement of pleural symphysis, additional procedures, such as combination of parietal pleural abrasion; apical pleurectomy; or chemical, laser, or electrocautery pleurodesis with VATS bleb resection was attempted (7). Among them, additional chemical pleurodesis was reported to be associated with the lowest recurrence rate during VATS bleb resection on the basis of the results of a recent meta-analysis (8). It is clear that the chemical sclerosing agent must reach the maximum possible surface area of a normal mesothelium to obtain the best pleural symphysis, whereas other methods have been proven to be unsatisfactory especially during VATS (7).
Talc, autologous blood patch, minocycline (a tetracycline derivative), bleomycin, silver nitrate, iodopovidone, and OK-432 were reportedly used for additional chemical pleurodesis (9,10). Although talc insufflation during VATS is currently considered the best method for chemical pleurodesis, especially in patients with spontaneous pneumothoraces (11), no consensus has been reached on the best chemical agent for pleurodesis worldwide. Since 2009, minocycline and iodopovidone have been used for pleurodesis in our hospital because of prohibition of the use of talc by the government. Furthermore, both agents are cheap or free to use in Korea. (The price of minocycline for pleurodesis is 0.22 US dollar, and iodopovidone is free to use in the most hospitals in Korea.) No studies comparing the safety and efficacy of iodopovidone and minocycline for additional chemical pleurodesis are currently available. In the present study, we evaluated additional chemical pleurodesis to VATS bleb resection for PSP with iodopovidone or minocycline, and compared the outcomes of both chemical agents using propensity score matching analysis.
Methods
This retrospective study was approved by the Institutional Review Board of our institute, and the need of informed consent was waived (2018GR0211). All patients initially underwent closed thoracostomy and were evaluated using chest computerized tomography (CT). The surgical indications for VATS bleb resection in our hospital are mentioned in a previous report (12,13) and are as follows: the first episode of pneumothorax with complications, bilateral pneumothorax, prior history of ipsilateral or contralateral pneumothorax, or visible blebs or bullae on the chest CT.
Each chemical agent for pleurodesis was prepared in the operating room: 2 mL of 10% iodopovidone mixed with 48 mL of normal saline was used in the iodopovidone group (group I), and 150 mg of minocycline mixed with 100 mL of 5% dextrose solution was used in the minocycline group (group M). After careful inspection for identifying blebs on the lung parenchyma under thoracoscopy, bleb resection was performed using an endostapler. Intraoperative additional pleurodesis with either minocycline or iodopovidone was performed by insufflation under thoracoscopic guidance on the whole pleural cavity of the visceral and parietal pleurae. On completion of the operation, a chest tube was placed up to the apex of the thoracic cavity.
A negative pressure of 15–20 cmH2O was applied to the chest tube, and plain chest radiographs obtained checked daily. The amounts of drainage were recorded accordingly until the day of chest tube removal and any complications related to the intervention were noted. A body temperature higher than 37.5 °C was considered abnormal and prolonged air-leak was defined as a persistence of air-leak for more than 3 days in this study. In addition to these clinical data, the length of hospital stay and duration of chest indwelling were collected from the medical records. Bedside chemical pleurodesis was performed when prolonged air-leak was observed more than 5 days. The chest tube was removed when the amount of drainage was reduced to less than 2 mL/kg daily. Patients were discharged one or two days after chest tube removal, after confirming the absence of visible pneumothorax or pleural effusion on plain chest radiography. The duration of follow-up was defined as the time interval from the operation until the last visit to our outpatient clinic.
Statistics
Student’s t-test and Mann-Whitney U test were used to evaluate the differences among continuous variables, depending on the results of Shapiro-Wilk normality test. Categorical variables were expressed as numbers and percentages, and chi-squared test or Fisher’s exact test was used to compare the two groups. Propensity score matching was performed for a more accurate comparison. Baseline preoperative clinical parameters (age, sex, body mass index, and laterality of lesions) were used for propensity score matching. The recurrence rate was analyzed using the Kaplan-Meier method and compared between the groups using the log-rank test. Two-sided P values <0.05 were considered statistically significant. All statistical analyses were performed using SPSS ver. 20.0 (SPSS Inc., Chicago, IL, USA).
Results
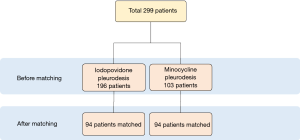
A total of 332 patients underwent thoracoscopic bleb resection for pneumothorax with additional pleurodesis either with iodopovidone or minocycline at Korea University Guro Hospital between February 2009 and October 2013. Among them, 33 patients diagnosed with secondary pneumothorax were excluded from the study, and 299 patients were enrolled for the analysis (Figure 1). The most common indications for VATS bleb resection were the first episode of pneumothorax with visible bleb on chest CT (120/299, 40.1%), ipsilateral recurrent episodes (83/299, 27.8%), the first episode of complicated pneumothorax (74/299, 24.8%), contralateral pneumothorax (17/299, 5.7%), and bilateral pneumothorax (5/299, 0.2%).
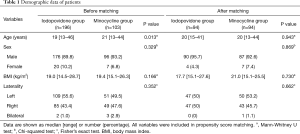
The median duration of follow-up was 14 months (range, 1–94 months). After propensity score matching, 94 patients from iodopovidone group and 94 patients from minocycline group were matched, including 177 men and 11 women with a median age of 20 years (range, 15–44 years) (Table 1). The median body mass index was 19.3 kg/m2 (range, 15.1–27.6 kg/m2).
Full table
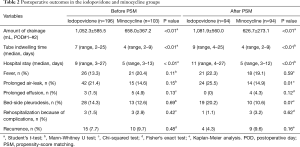
The perioperative outcomes are summarized in Table 2. During the period of hospitalization, no patient developed empyema, acute respiratory distress syndrome (ARDS), arrhythmia, or other severe complication. Sixty-four (30.0%) patients experienced at least one or more complications. The most common complication was fever in 39 patients (20.7%); however, all patients with fever recovered spontaneously. Prolonged air-leak was observed in 38 patients (20.2%); among them, in 9 patients, it was stopped spontaneously within 5 days, and 29 patients (76.3%) who had air leak more than 5 days were treated with 1–2 cycles of additional bed-side pleurodesis. In all cases, bed-side pleurodesis was conducted using minocycline, due to its simplicity in tube management. Prolonged effusion was observed in 4 patients (2.1%); all of them spontaneously recovered. The comparison of complication rates, such as fever (P=0.59), prolonged air-leak (P=0.01), prolonged effusion (P=0.12), and additional bed-side pleurodesis (P=0.07) between the two groups showed no statistical significance.
Full table
However, several significant differences in postoperative course were found between the two groups. The mean amount of drainage during the first postoperative two days was significantly smaller in group M than in group I (626.7±273.1 vs. 1,081±560.0 mL, P<0.01). Moreover, the median duration of chest tube indwelling was significantly shorter in group M compared to group I [4 days (range, 2–9 days) vs. 9 days (range, 4–25 days), P<0.01]. Consequently, the median hospital stay after the surgery was 5 days in group M (range, 3–12 days) and 11 days in group I (range, 4–27 days), and the difference was statistically significant (P<0.001).
Four patients were readmitted due to delayed onset of pleural effusion. Among them, one patient showed pleural effusion with fever and serum leukocytosis. He was treated with antibiotics and pigtail catheter drainage. The other three patients showed eosinophilic effusion without any sign of infection, and were treated with pig-tail catheter. The duration between discharge and readmission was 9–37 days and no statistically difference was found between the two groups (P=0.62).
During the follow-up period (median, 14 months), recurrence occurred in 13 patients (6.9%). The median recurrence-free interval was 4 months (range, 0–32 months) and no difference in recurrence rate was found between group I and group M (4.3% vs. 9.6%, P=0.16). All patients with recurrences were managed with closed thoracostomy with or without bed-side pleurodesis using minocycline, and none of them underwent reoperation.
Discussion
This propensity-score matched data analysis showed that additional pleurodesis with minocycline was associated with smaller amount of postoperative pleural effusion compared to iodopovidone; therefore, shorter hospital stay could be achieved with comparable complications and recurrence rate after the surgery. No patient developed severe complications such as ARDS, confirming the safety of both agents. The only complications found within the postoperative days were fever, persistent air leak, and prolonged effusion.
One of the most common complications was fever. Fever was regarded as a response to inflammatory reaction from chemical pleurodesis. Other studies showed that tetracycline pleurodesis yielded 9–81% of fever complications (14-16), while iodopovidone was associated with fever in 6.1–33% of cases (17,18). In our study, fever occurred in 21 patients from the iodopovidone group (22.3%) and in 18 patients from minocycline group (19.1%), with no statistical difference. Fever spontaneously recovered by conservative treatment in all patients.
Persistent air leak was another common complication in this study (24.5% in group I and 14.9% in group M), which showed higher incidence comparing to other studies (2,6). However, all these air leaks were resolved spontaneously or successfully managed by bedside pleurodesis.
The reported recurrence rate after VATS bullectomy alone was 16.0–23.9% (2,19). A multicenter randomized controlled study in Korea reported a recurrence rate requiring intervention of 5.8% in staple line coverage group and 7.8% in mechanical pleurodesis group (3). The recurrence rate of our study was 4.3% in group I and 9.6% in group M, showing comparable outcomes without statistical difference between the two groups.
Although no statistical difference was found between the outcomes of the two groups, some significant differences existed in postoperative course. Patients who received minocycline pleurodesis had a shorter duration of chest tube indwelling and hospitalization after the surgery. These results indicate that minocycline may provide better quality of postoperative care compared to iodopovidone. The mechanism of different amounts of drainage remains unclear. Iodopovidone has low pH and strong oxidative and cytotoxic properties, which may induce a potent inflammatory response, and subsequently, pleural fibrosis (20). Minocycline, a derivative of tetracycline, is as effective as tetracycline in inducing pleural inflammation and fibrosis (21). In an animal study, the inflammatory response after iodopovidone pleurodesis seemed to be similar to that after minocycline (22). Furthermore, in the same study, the dosage of iodopovidone did not induce any difference in outcomes. Our policy of the timing of tube removal was uniformly applied in both groups. In these regards, the differences in the postoperative course between the two agents were not presupposed and the difference between the minocycline- and iodopovidone-induced amounts of drainage was unknown.
Another unique finding of our study was the late onset of pleural effusion after additional pleurodesis. Four patients showed delayed onset of pleural effusion, which was not visible on chest radiography during the first postoperative visit after discharge. Except one patient who presented with fever, all other three patients who were readmitted showed eosinophilic effusion without any symptom. This result might be related to an infrequent hypersensitivity to the sclerosing agent; however, the sample size was not sufficient to find a clear explanation of this finding.
This study has a retrospective design and is not without limitations. First, because of the relatively short duration of follow-up, the recurrence rate was possibly underestimated. Second, the protocol for pain management was not uniform during the study period; therefore, direct pain comparison between the two agents was not possible. Finally, pre- and post-operative pulmonary function test could not be performed because our national health care system strictly refrained from providing financial support for this test.
In conclusion, this study confirmed the safety of both minocycline and iodopovidone for additional pleurodesis. However, we carefully recommend minocycline pleurodesis over iodopovidone pleurodesis because of the better postoperative recovery associated with minocycline.
Acknowledgements
Funding: This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI17C0654).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by the Institutional Review Board of our institute, and the need of informed consent was waived (2018GR0211).
References
- Kim H, Kim HK, Choi YH, et al. Thoracoscopic bleb resection using two-lung ventilation anesthesia with low tidal volume for primary spontaneous pneumothorax. Ann Thorac Surg 2009;87:880-5. [Crossref] [PubMed]
- Horio H, Nomori H, Kobayashi R, et al. Impact of additional pleurodesis in video-assisted thoracoscopic bullectomy for primary spontaneous pneumothorax. Surg Endosc 2002;16:630-4. [Crossref] [PubMed]
- Lee S, Kim HR, Cho S, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg. 2014;98:2005-11. [Crossref] [PubMed]
- Sawada S, Watanabe Y, Moriyama S. Video-assisted thoracoscopic surgery for primary spontaneous pneumothorax: evaluation of indications and long-term outcome compared with conservative treatment and open thoracotomy. Chest 2005;127:2226-30. [Crossref] [PubMed]
- Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med 2000;342:868-74. [Crossref] [PubMed]
- Chen JS, Hsu HH, Kuo SW, et al. Effects of additional minocycline pleurodesis after thoracoscopic procedures for primary spontaneous pneumothorax. Chest 2004;125:50-5. [Crossref] [PubMed]
- Tschopp JM, Rami-Porta R, Noppen M, et al. Management of spontaneous pneumothorax: state of the art. Eur Respir J 2006;28:637-50. [Crossref] [PubMed]
- Sudduth CL, Shinnick JK, Geng Z, et al. Optimal surgical technique in spontaneous pneumothorax: a systematic review and meta-analysis. J Surg Res 2017;210:32-46. [Crossref] [PubMed]
- How CH, Tsai TM, Kuo SW, et al. Chemical pleurodesis for prolonged postoperative air leak in primary spontaneous pneumothorax. J Formos Med Assoc 2014;113:284-90. [Crossref] [PubMed]
- Agarwal R. Iodopovidone: an inexpensive and effective agent for chemical pleurodesis. Lung Cancer 2007;55:253-4. [Crossref] [PubMed]
- Noppen M, De Keukeleire T. Pneumothorax. Respiration. 2008;76:121-7. [Crossref] [PubMed]
- Lee DK, Kim HK, Lee K, et al. Optimal Respiratory Rate for Low-Tidal Volume and Two-Lung Ventilation in Thoracoscopic Bleb Resection. J Cardiothorac Vasc Anesth. 2015;29:972-6. [Crossref] [PubMed]
- Kim H, Kim HK, Kang DY, et al. A comparative study of two- versus one-lung ventilation for needlescopic bleb resection. Eur Respir J 2011;37:1183-8. [Crossref] [PubMed]
- Alfageme I, Moreno L, Huertas C, et al. Spontaneous pneumothorax. Long-term results with tetracycline pleurodesis. Chest 1994;106:347-50. [Crossref] [PubMed]
- Light RW, O'Hara VS, Moritz TE, et al. Intrapleural tetracycline for the prevention of recurrent spontaneous pneumothorax. Results of a Department of Veterans Affairs cooperative study. JAMA 1990;264:2224-30. [Crossref] [PubMed]
- Light RW, Vargas FS. Pleural sclerosis for the treatment of pneumothorax and pleural effusion. Lung 1997;175:213-23. [Crossref] [PubMed]
- Aelony Y. Talc pleurodesis vs iodopovidone. Chest 2003;123:1318-9; author reply 9. [Crossref] [PubMed]
- Agarwal R, Khan A, Aggarwal AN, et al. Efficacy & safety of iodopovidone pleurodesis: a systematic review & meta-analysis. Indian J Med Res 2012;135:297-304. [PubMed]
- Nakanishi K. An apical symphysial technique using a wide absorbable mesh placed on the apex for primary spontaneous pneumothorax. Surg Endosc 2009;23:2515-21. [Crossref] [PubMed]
- Agarwal R, Paul AS, Aggarwal AN, et al. A randomized controlled trial of the efficacy of cosmetic talc compared with iodopovidone for chemical pleurodesis. Respirology 2011;16:1064-9. [Crossref] [PubMed]
- Light RW, Wang NS, Sassoon CS, et al. Comparison of the effectiveness of tetracycline and minocycline as pleural sclerosing agents in rabbits. Chest 1994;106:577-82. [Crossref] [PubMed]
- Guo Y, Tang K, Bilaceroglu S, et al. Iodopovidone is as effective as doxycycline in producing pleurodesis in rabbits. Respirology 2010;15:119-25. [Crossref] [PubMed]