
Closed chest compressions after rib plating
Introduction
Effective conventional closed chest compressions (CCC) in the treatment of cardiac arrest in adults is associated with sternal and rib fractures. Although rare, these fractures can result in life-threatening injuries such as cardiac laceration and pericardial tamponade (1,2). The popularity of surgical stabilization of rib fractures (SSRF) is on the rise, owing to increasing evidence suggesting its association with improved analgesia, faster return to work, reduced hospital stay, and decreased incidence rates of respiratory failure and pneumonia (3,4). The feasibility and effect of cardiopulmonary resuscitation (CPR) on rib plates are still largely unknown (5). To our knowledge, only one previous case report has discussed the effects of CCC on rib plating where hardware failure occurred (6). We present a patient with rib plates who received successful CCC during multiple cycles of CPR.
Case presentation
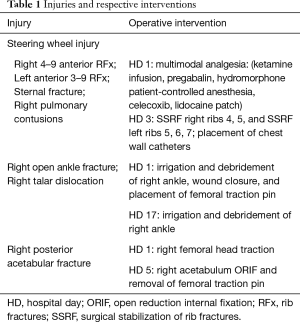
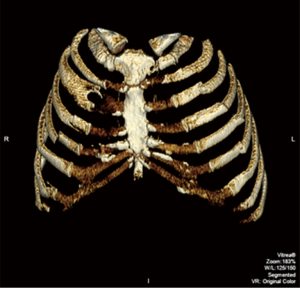
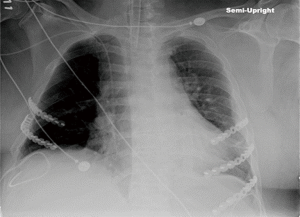
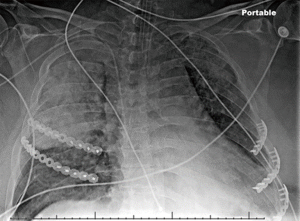
This case report was reviewed and approved by our institution’s ethical review board. A 54-year-old unrestrained driver was transferred from a local hospital to our level 1 trauma center after driving his car off a cliff. His past medical history included chronic obstructive pulmonary disease, diastolic dysfunction, and myocardial infarction on dual antiplatelet therapy status post bare metal cardiac stent placement 2 years ago. He was evaluated and treated according to Advanced Trauma Life Support®. His injuries along with a comprehensive list of operative interventions are shown in Table 1. Of note, he had multiple rib fractures, as shown in Figure 1. He was admitted to the surgical intensive care unit and was placed on multimodal analgesia (Table 1). The patient was not a candidate for paravertebral or epidural pain catheter insertion because of his antiplatelet therapy. Due to increasing pain and oxygen requirements, non-invasive positive pressure ventilation was required. On hospital day (HD) 3, he underwent bronchoscopy, placement of chest wall pain catheters, and SSRF of right ribs 4–5 and left ribs 5–7 using the Synthes MatrixRIB Fixation System (Synthes, West Chester, PA, USA) (Figure 2). On HD 5, he underwent open reduction internal fixation (ORIF) of his right acetabulum and was extubated on HD 6. On HD 8, the patient sustained pulseless electrical activity (PEA) arrest and was treated with CPR for 7 min with ensuing return of spontaneous circulation (ROSC). The cardiac arrest was the result of respiratory failure due to pulmonary embolism, which was confirmed by a subsequent computed tomography (CT). Incidentally, CT images revealed an intact post-CCC SSRF (Figure 3). Physical examinations showed no evidence of chest wall instability, clicking, or crepitation. Anticoagulation and diuresis were started, and the patient was extubated to non-invasive positive pressure ventilation on HD 17. Three days later, he went into a second PEA arrest. CPR was performed for 23 min with ROSC. A follow-up chest X-ray to assess intubation demonstrated right lung consolidation and intact SSRF plates (Figure 4). Unfortunately, the patient remained in multisystem organ failure with refractory hypotension, and his family elected for comfort measures without escalation of care. The patient expired 20 days after presentation.
Full table

Discussion
This case demonstrates that effective CPR after rib plating is possible without prosthetic fracture, periprosthetic fracture, screw pullout, or other deformation of the reconstructed chest wall.
Key metrics for high-quality CPR according to the American Heart Association include insuring adequate CCC depth and achieving complete chest wall recoil (7). The forces needed for effective compressions put significant stress on the rib cage. Skeletal chest injuries from CPR are well documented among individuals without prior rib fractures. The incidence of rib fractures after CPR is reported in over 70% of CPR cases, with a mean number of 7.6 broken ribs per person (8). Despite their rarity, these fractures can result in fatal injuries such as cardiac laceration and pericardial tamponade (1,2). Significant forces required for effective CCC raises the potential concern that a reconstructed chest wall with plate may impede the delivery of chest compressions. Successful CPR implies both ROSC and an uncomplicated neurological recovery (9). Our patient was neurologically intact and achieved ROSC after the first cardiac arrest. Likewise, he had ROSC after the second arrest, but the extent of neurological impairment remains unknown. We conclude that effective CPR is feasible after SSRF.
While SSRF does not appear to impede the delivery of CPR, hardware failure is a legitimate concern due to the application of significant forces to the rib plating system and landing site. For the SSRF hardware to withstand the compressive dynamics of CCC, the implants must be capable of demonstrating both immense strength and dynamic flexibility. Newer systems demonstrated low profile and easier insertion, but achieved the optimal balance of flexibility and strength to mimic normal rib function. Anatomic, pre-contoured plates have been designed and tested to permit not only regular breathing but also to withstand the stress of respiration and other functions of the chest wall. One prospective study following patients that had been treated with the MatrixRIB fixation system found no accounts of hardware failure or loss of initial fixation among 91 rib plates placed at their 6-month follow-up (10). Additionally, the use of bicortical engagement screws through the chest wall cortex and pleural cortex, along with the threaded screw head that engages in threaded plate holes that lock the screw, confers additional plate security and prevents pullout (11). In fact, an in vitro biomechanical study estimated that the combined approach of flexible rib plating with locking screw fixation not only prevents screw loosening and pullout, but can restore up to 77% of the native rib strength (12).
Despite the advances in the rib plating system technology, hardware failure such as screw pullout and additional rib fractures as a result of a single cycle of CPR after SSRF is possible (6). However, our patient experienced neither hardware failure nor additional rib fractures even after receiving multiple extended rounds of CPR at less than 1 week postoperatively. Further reports are needed to elucidate a more delayed effect of CPR on rib plates.
Conclusions
This case report illustrates that rib plates can not only allow effective CPR but also withstand the compressive forces of multiple rounds of CPR without mechanical failure. Further studies are needed to investigate the effects of CPR on rib plates in a larger subset of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: Marcel Tafen is a paid speaker/presenter for Synthes. The other authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient’s legally authorized representative for publication of this manuscript and any accompanying images.
References
- Machii M, Inaba H, Nakae H, et al. Cardiac rupture by penetration of fractured sternum: a rare complication of cardiopulmonary resuscitation. Resuscitation 2000;43:151-3. [Crossref] [PubMed]
- Noffsinger AE, Blisard KS, Balko MG. Cardiac laceration and pericardial tamponade due to cardiopulmonary resuscitation after myocardial infarction. J Forensic Sci 1991;36:1760-4. [Crossref] [PubMed]
- Slobogean GP, MacPherson CA, Sun T, et al. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg 2013;216:302-11.e1. [Crossref] [PubMed]
- Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924-32. [Crossref] [PubMed]
- McKay DR, Fawzy HF, McKay KM, et al. Are chest compressions safe for the patient reconstructed with sternal plates? Evaluating the safety of cardiopulmonary resuscitation using a human cadaveric model. J Cardiothorac Surg 2010;5:64. [Crossref] [PubMed]
- Edgerton CA, Crookes BA, Eriksson EA. Performance of Rib Plate Hardware in an Elderly Woman Receiving Cardiopulmonary Resuscitation after Surgical Rib Fixation. Am Surg 2017;83:e291-3. [PubMed]
- Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S414-35. [Crossref] [PubMed]
- Ihnát Rudinská L, Hejna P, Smatanová M, et al. Injuries associated with cardiopulmonary resuscitation in non-survivors after out-of-hospital cardiac arrest (autopsy study). Soud Lek 2017;62:18-21. [PubMed]
- Youness H, Al Halabi T, Hussein H, et al. Review and Outcome of Prolonged Cardiopulmonary Resuscitation. Crit Care Res Pract 2016;2016:7384649. [Crossref] [PubMed]
- Bottlang M, Long WB, Phelan D, et al. Surgical stabilization of flail chest injuries with MatrixRIB implants: a prospective observational study. Injury 2013;44:232-8. [Crossref] [PubMed]
- Pape HC, Bottlang M. Flexible fixation with locking plates. J Orthop Trauma 2011;25 Suppl 1:S1-3. [Crossref] [PubMed]
- Bottlang M, Walleser S, Noll M, et al. Biomechanical rationale and evaluation of an implan.t system for rib fracture fixation. Eur J Trauma Emerg Surg 2010;36:417-26. [Crossref] [PubMed]


