Bronchial aneurysm secondary to tuberculosis presenting with fatal hemoptysis: a case report and review of the literature
Case presentation
A 59-year-old female with repeatedly dry cough for half a year and low-grade fever for four days was referred to our hospital. There was no associated history of hemoptysis. She went to a local hospital where antibiotics (specific type unknown) were prescribed, but her symptoms were not relieved. A chest CT scan was done which revealed multiple focal nodules in the right lung field, enlarged mediastinal lymph nodes and atelectasis (Figure 1A-C). She also had a past medical history of cirrhosis and gastroesophageal varices secondary to chronic viral hepatitis C for which endoscopic band ligation was performed twice to prevent massive bleeding due to gastroesophageal varices.
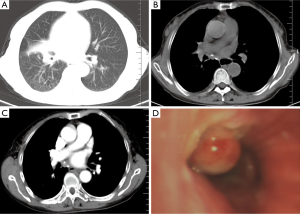
On admission, physical examination was remarkable only for fever of 37.9 °C. The laboratory results were as follows: white blood cell (WBC) count was 4,600 cells/µL with 81.8% neutrophils, C reactive protein (CRP) level was 81.3 mg/L, and erythrocyte sedimentation rate (ESR) level was 77 mm in the first hour. Serum tumor markers were negative. Liver and renal function tests were within normal limits. Coagulation profile was normal. This patient then underwent a bronchoscopy that revealed an obvious pulsatile aneurysm (4 mm × 4 mm) in her right intermediate bronchus (Figure 1D) and its tunica mucosa was irregular. Microbiological tests of sputum specimens were positive for acid fast bacilli. During the bronchoscopy procedure, an unexpected massive episode of hemoptysis developed due to rupture of the aneurysm. Emergency intubation was performed to keep the respiratory tract patent but copious amount of blood emerged from the cannula. Unfortunately, this patient died after 4 hours despite of giving the best supportive care.
Discussion
Fatal hemoptysis is a serious complication of pulmonary tuberculosis (1). We present a rare case of fatal hemoptysis due to bronchial aneurysm in a patient with active pulmonary tuberculosis. Pulmonary tuberculosis is complicated with vascular lesions including pulmonary or bronchial arteritis and thrombosis, bronchial artery dilatation, and Rasmussen aneurysm (2). Meanwhile, tuberculosis can also rarely cause aneurysm formation in other organs, such as brain and aorta (3). The pathogenesis of vascular lesions may be associated with chronic inflammation leading to neovascularization and increased collateral supply from nearby systemic arteries. These newly formed collateral vessels have weak arterial wall and are prone to rupture (4). A rare case of bronchial artery aneurysm presenting with massive hemoptysis due to pulmonary tuberculosis was previously reported, and the definitive diagnosis was made using multidetector computed tomographic (MDCT) angiography (4).
Autopsy and MDCT angiography strategies are more reliable than bronchoscopy for diagnosis of bronchial artery aneurysm. In our case, we attribute the cause of fatal hemoptysis to the rupture of bronchial artery aneurysm which was associated with vascular lesions due to mycobacterium tuberculosis infection. The clinical findings in favor of this are primarily the presence of an obvious pulsatile aneurysm which was detected by bronchoscopy, lesions in the mucosa, luminal stenosis, and microbiological tests of sputum specimens indicative of acid fast bacilli. Additionally, rupture of bronchial aneurysm occurred during bronchoscopy. Secondly, although bronchial and lower tracheal varices, pulmonary hypertension and elevation of pulmonary venous pressure can occur in end-stage alcoholic liver disease with portal hypertension, which has led to massive hemoptysis in previous case reports (5), there were no signs of such bronchial and lower tracheal varices detected by bronchoscopy in our case. Besides, our patient had undergone endoscopic band ligation twice in the past to prevent massive bleeding due to gastroesophageal varices. Thirdly, arterial pulmonary hypertension formation may be due to the presence of portocaval shunts that can cause massive hemoptysis (6), but its detection by radiological imaging is limited. Finally, endobronchial mycotic pulmonary artery aneurysm (PAA) is another cause of massive hemoptysis (7), but no fungus was detected from appropriate sputum sample.
Conclusions
Bronchial artery aneurysm is a rare complication of mycobacterium tuberculosis infection, which may lead to fatal hemoptysis and should always be considered in the differential diagnosis. Detailed radiological examination to rule out the possibility of aneurysm existing in the nearby lesions caused by infectious disease is of prime importance prior to bronchoscopy. Effective and emergent treatment should be performed to control such life-threatening bleeding, including rigid bronchoscopy, endovascular therapy and surgery (8), and endovascular stent-graft repair (9).
Acknowledgements
The Talent Introduction Procedure of Wannan Medical College to Zhi-Wei Lu was used to support the collection and interpretation of patient information.
Disclosure: The authors declare no conflict of interest.
References
- Lee BR, Yu JY, Ban HJ, et al. Analysis of patients with hemoptysis in a tertiary referral hospital. Tuberc Respir Dis (Seoul) 2012;73:107-14. [PubMed]
- Kim HY, Song KS, Goo JM, et al. Thoracic Sequelae and Complications of Tuberculosis. Received 2001;21:839-58; discussion 859-60.
- Saraf R, Limaye U. Ruptured intracranial tubercular infectious aneurysm secondary to a tuberculoma and its endovascular management. Br J Neurosurg 2013;27:243-5. [PubMed]
- Karmakar S, Nath A, Neyaz Z, et al. Bronchial artery aneurysm due to pulmonary tuberculosis: detection with multidetector computed tomographic angiography. J Clin Imaging Sci 2011;1:26. [PubMed]
- Youssef AI, Escalante-Glorsky S, Bonnet RB, et al. Hemoptysis secondary to bronchial varices associated with alcoholic liver cirrhosis and portal hypertension. Am J Gastroenterol 1994;89:1562-3. [PubMed]
- Radulescu D, Duncea C, Donca V. Hepatic cirrhosis associated with arterial pulmonary hypertension. Rom J Gastroenterol 2004;13:341-3. [PubMed]
- Dransfield MT, Johnson JE. A mycotic pulmonary artery aneurysm presenting as an endobronchial mass. Chest 2003;124:1610-2. [PubMed]
- Sakr L, Dutau H. Massive hemoptysis: an update on the role of bronchoscopy in diagnosis and management. Respiration 2010;80:38-58. [PubMed]
- Kasashima F, Endo M, Kosugi I, et al. Mediastinal bronchial artery aneurysm treated with a stent-graft. J Endovasc Ther 2003;10:381-5. [PubMed]


