
Chest wall stabilization and rib plating in 15-year-old male adolescent after blunt thoracic trauma
Introduction
Rib fractures after blunt trauma to the chest wall are a very common injury in adults, but are less often encountered in the pediatric population due to the bony compliance of the pediatric chest wall (1). Rib fractures carry morbidity and mortality risks, and can lead to long-term disabilities, prolonged narcotic use, pneumonia, respiratory difficulties while complicating the rehabilitation of other injuries. Historically, the treatment for rib fractures has consisted of analgesia, pulmonary toilet, and supplemental oxygen support (2). With the development of plating systems for rib fracture fixation, the practice pattern of rib fracture management is shifting, as a viable operative intervention now exists to improve clinical outcomes (3,4). However, no reported cases exist describing rib plating after trauma in the pediatric population. We report the case of a 15-year-old, 72-kilogram male patient with severe displacement of multiple rib fractures after blunt chest trauma, along with our resultant operative strategy with rib plating for chest wall stabilization.
Case presentation
The patient was a 15-year-old male involved in an all-terrain vehicle accident reportedly being thrown approximately twenty feet from the accident site. During emergency medical transport, the patient demonstrated a decline in respiratory status. He was intubated and required right chest needle decompression due to suspicion of a tension pneumothorax.
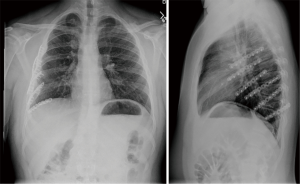
On arrival to the trauma bay, a large bore chest tube was placed into the right chest, and approximately 500 mL of hemothorax was evacuated. After clinical and radiographic evaluation, identification of injuries included: a complex skull fracture, subarachnoid and intraventricular hemorrhage, an odontoid fracture, bilateral mandible fractures, bilateral scapula fractures, a left clavicle fracture, and multiple displaced right rib fractures. The patient’s right-sided chest wall was noted to have complex fractures with significant displacements of ribs number 3 through 10 (Figure 1). Given the number and severity of the chest wall fracture pattern, pulmonary contusion, and continued ventilator dependence, the decision to take the patient to the operating room for chest wall reconstruction with rib plating was reached.
On post-trauma day four, the patient underwent bilateral mandibular open reduction internal fixation (ORIF) with maxillomandibular fixation (MMF), tracheostomy tube placement, and chest wall stabilization using the Synthes MatrixRIB® Fixation System. The chest wall stabilization was performed using a vertical chest wall incision and a muscle sparing technique. Ribs 4–9 were reduced and plated. Rib number 3 was not plated due to the fracture’s minimal displacement. A 28-French thoracostomy tube was placed. A standard, multilayer closure of the chest wall was achieved, and the patient was transferred to the pediatric intensive care unit.
The patient was weaned from the ventilator on post-operative day number 5 and transferred to a rehabilitation center on post-trauma day number 20 where he experienced an uncomplicated recovery and reestablished full functional capacity. Two years after the patient’s discharge, a re-evaluation was conducted with a physical examination, pulmonary function testing, and radiographic imaging (Figure 2) which demonstrated no deleterious impact on bone growth and expected development.
Discussion
The use of rib plating systems for stabilization of the chest wall after injury is becoming more commonly practiced in the adult population with satisfying patient outcomes (2-5), but to the author’s knowledge, no reported cases exist describing the fixation of displaced ribs in the pediatric patient after trauma.
Less mineralization allows for greater chest wall compliance and pliability likely contributing to an overall lower incidence of rib fractures in children compared to adults (1). However, as children age and as bony calcification continues, bone density and skeletal maturity in adolescent, pediatric patients may, in this regard, appear more similar to adults. Despite this, rib fixation for pediatric trauma has not been well investigated, and no consensus or guidelines exist (6).
The authors acknowledge the need to consider pediatric osteosynthesis with anterior fixation hardware and the potential disturbance of the growing skeletal frame and bony immuring in this case (7,8). However, given the lack of growth plates involved in the fractures, and our patient’s size and seemingly mature bony skeleton, these concerns were felt to be outweighed by the benefit of improved respiratory mechanics and pain control. Additionally, periprosthetic fractures in athletes is a known complication of hardware implantation, but it is yet unknown if similar risks apply to rib plating (7). Although much debate exists regarding the degradation of implanted hardware and systemic release of chemical elements, the titanium alloy composition in our applied plating system is thought to be less susceptible to corrosion and considered safe to be retained in situ (7,9).
Chest wall stabilization with rib plating is proving to allow for better pain control, improved respiratory mechanics and the shortening of overall recovery time in adults (10). The clinical significance of pediatric rib fractures has historically been related to the association of concomitant intra-thoracic and intra-abdominal organ injuries (1); however, there is still little literature dedicated to the evaluation of recovery time and the respiratory limitations that may impact recovery after a traumatic event.
Conclusions
Rib fracture fixation is a viable surgical alternative to conservative management strategies for severe chest wall trauma. As data reflecting the positive impact that chest wall stabilization has on the survival and recovery of the trauma patient continues to accumulate, the application of rib plating may eventually be expanded to the pediatric population. Our patient has recovered well and will continue to be followed clinically.
Considerations for offering surgical stabilization of rib fractures in individual cases should focus on several factors including: (I) clinical presentation of each patient including degree of respiratory support; (II) skeletal maturity of the individual patient; (III) degree of disruption and location of the fracture in relation to the remaining bony thorax. More reports of rib plating in the pediatric population are needed to ascertain the utility of the technique in this patient population.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Nakayama DK, Ramenofsky ML, Rowe MI. Chest injuries in childhood. Ann Surg 1989;210:770-5. [Crossref] [PubMed]
- Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma 1994;37:975-9. [Crossref] [PubMed]
- Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924-32. [Crossref] [PubMed]
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. [Crossref] [PubMed]
- Girsowicz E, Falcoz PE, Santelmo N, et al. Does surgical stabilization improve outcomes in patients with isolated multiple distracted and painful non-flail rib fractures? Interact Cardiovasc Thorac Surg 2012;14:312-5. [Crossref] [PubMed]
- Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307-21. [Crossref] [PubMed]
- Hanson B, van der Werken C, Stengel D. Surgeons' beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord 2008;9:73. [Crossref] [PubMed]
- Pretell-Mazzini J, Zafra-Jimenez JA, Rodriguez Martin J. Clinical application of locked plating system in children. An orthopaedic view. Int Orthop 2010;34:931-8. [Crossref] [PubMed]
- Uhthoff HK, Poitras P, Backman DS. Internal plate fixation of fractures: short history and recent developments. J Orthop Sci 2006;11:118-26. [Crossref] [PubMed]
- Majercik S, Cannon Q, Granger SR, et al. Long-term patient outcomes after surgical stabilization of rib fractures. Am J Surg 2014;208:88-92. [Crossref] [PubMed]



