
Predictor of cardiopulmonary complication after pulmonary resection
Pulmonary resection is the standard treatment in patients with stage I-II non-small cell lung cancer. However, despite recent advancements in perioperative management and minimally invasive surgical techniques, the incidence of postoperative cardiopulmonary complication remains as high as 7% to 43% (1,2). To improve the safety of pulmonary resection for lung cancer, it is essential to detect patients at high-risk of postoperative cardiopulmonary complications. Although pulmonary function tests, including a test of the diffusing capacity of the lungs for carbon monoxide and cardiopulmonary exercise test for patients with poor pulmonary function, are the gold standard of preoperative risk assessment (3,4), more convenient methods to detect patients at high-risk are needed.
Regarding this clinical issue, Fu et al. investigated the correlation between high preoperative resting heart rate and cardiopulmonary complications after resection for lung cancer (5). The authors examined 180 patients who underwent pulmonary resection for non-small cell lung cancer at their institution prospectively. Of the 180 patients, 42 (23%) patients developed postoperative cardiopulmonary complications. Cardiopulmonary complication was defined as the presence of the following complications: pleural effusion requiring drainage, arrhythmia, pneumonia, atelectasis, respiratory failure, acute respiratory distress syndrome, mechanical ventilation within 48 hours after surgery, pneumothorax, pyothorax, pulmonary embolism, and myocardial infarction in the study. The most frequent cardiopulmonary complication in the study was pleural effusion requiring drainage (8.3%), followed by arrhythmias (6.1%). The authors demonstrated that age, preoperative beta-blocker therapy, resting heart rate, comorbidities of hypertension, coronary artery disease, revised cardiac risk index, clinical stage > III, elevated cardiac troponin T, and elevated tumor necrosis factor alpha were risk factors for postoperative cardiopulmonary complications using univariate analysis. However, increased preoperative resting heart rate was the only independent predictor of postoperative cardiopulmonary complications using multiple logistic regression analysis [odds ratio (OR): 4.48; 95% confidence interval (CI): 1.17–18.42; P=0.021]. Moreover, receiver operating characteristics curve analysis showed that elevated resting heart rate was a predictor of postoperative cardiopulmonary complications, with a cut-off value of 86 beats per minute (area under the curve: 0.813; specificity: 80.95%; sensitivity: 72.46%; P<0.001).
As Fu et al. indicated in the discussion section, a high resting heart rate has been reported to correlate with cardiac events, such as incidental heart failure, in the elderly or in healthy adults (6-8). Previous studies reported that high resting heart rate correlated with all-cause mortality and cardiovascular mortality in a general population (9). Moreover, high resting heart rate (>87 beats per minute) was reported to be correlated with postoperative myocardial dysfunction and mortality following a non-cardiac surgery (10). The underlying mechanisms linking high resting heart rate to cardiac events in a general population or to postoperative cardiopulmonary complications remain unclear. However, one of the possible explanations is that a high resting heart rate is the result of potential impaired systolic function. Another hypothesis is that high resting heart rate is the cause of elevated myocardial oxygen consumption and decreased myocardial blood flow with shortened diastolic time interval, resulting in myocardial ischemia and damage. Wong et al. reported that heart rate as well as systolic pulmonary arterial pressure are the main determining factors of oxygen consumption in the myocardium of the right ventricle of patients with pulmonary arterial hypertension (11). Although Fu et al. focused on the relationship between resting heart rate and cardiac disease as the underlying mechanisms, high resting heart rate had been reported to correlate with pulmonary disease. Previous reports showed that high resting heart rate correlates with all-cause mortality in patients with chronic obstructive pulmonary disease (12,13). Therefore, the high rates of cardiopulmonary complications in patients with high resting heart rate might be partly explained by the potential impaired pulmonary function.
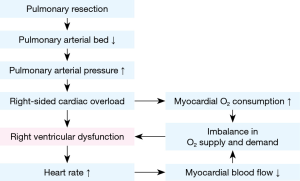
Of all non-cardiac surgeries, pulmonary resection is the surgical procedure that most greatly affects cardiac function. This may be why Fu et al. chose to examine the correlation between resting heart rate and cardiopulmonary complication after pulmonary resection. One of the mechanisms by which pulmonary resection affects cardiac function is changes of cardiopulmonary hemodynamics. Pulmonary resection results in reduction of the pulmonary arterial bed, which raises the pressure of the pulmonary artery and may lead to right ventricular impairment, particularly in patients with potential impaired cardiac function or pulmonary hypertension (Figure 1). Supporting this hypothesis, decreased preoperative right ventricular ejection fraction has been reported as the determinant of cardiopulmonary complication after pulmonary resection (14). Several studies showed that preoperative pulmonary hypertension is the predictor of cardiopulmonary complication after pulmonary resection (15-17). Moreover, we previously reported that an enlarged right main pulmonary artery on computed tomography, which is a well-established surrogate measure of pulmonary hypertension (18), correlated with cardiopulmonary complication after pulmonary resection (1).
One of the most common cardiopulmonary complications after pulmonary resection is atrial fibrillation with a reported incidence of 28% (19). The causes of postoperative atrial fibrillation after pulmonary resection are right-sided cardiac overload, imbalance of the autonomic nerve system, and surgical inflammation. Various agents, including amiodarone, had been reported to prevent postoperative atrial fibrillation. Nojiri et al. reported that an elevated B-type natriuretic peptide level is a risk factor for atrial fibrillation and cardiopulmonary complications after pulmonary resection for lung cancer (2,19). Recently, they also reported that continuous infusion of the low-dose phosphodiesterase III inhibitor-Olprinone, which has pulmonary vasodilatory and inotropic effects, showed a prophylactic effect on postoperative atrial fibrillation after lung cancer surgery in patients with elevated preoperative B-type natriuretic peptide level, using a double-blinded placebo-controlled study (20). These studies indicate the importance of detecting surgical candidates at high-risk for cardiopulmonary complications and supporting postoperative cardiac function in such patients.
I have one concern regarding the definition of cardiopulmonary complication in the literature by Fu et al. They included pleural effusion requiring drainage as a cardiopulmonary complication, and it was the most frequent cardiopulmonary complication in the study. However, pleural effusion is sometimes associated with technical complications such as postoperative hemorrhage or chylothorax. Therefore, it might have been better to exclude pleural effusion from cardiopulmonary complications, because they attempted to examine the correlation between cardiac status and cardiopulmonary complications.
In conclusion, Fu et al. provided valuable insight on the clinical importance of high resting heart rate as the predictor of cardiopulmonary complication after pulmonary resection. Measuring high resting heart rate is an easy to perform, low-cost screening method for patients at high-risk for cardiopulmonary complications. General thoracic surgeons should keep in mind that pulmonary resection is the non-cardiac surgery that mostly affects cardiac function. Cardiopulmonary exercise test or echocardiography can assess cardiac function precisely. However, they are not easy to perform on all surgical candidates. More convenient screening methods to assess impaired cardiopulmonary function, like high resting heart rate, are needed to increase the safety of pulmonary resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Asakura K, Mitsuboshi S, Tsuji M, et al. Pulmonary arterial enlargement predicts cardiopulmonary complications after pulmonary resection for lung cancer: a retrospective cohort study. J Cardiothorac Surg 2015;10:113. [Crossref] [PubMed]
- Nojiri T, Inoue M, Yamamoto K, et al. B-type natriuretic Peptide as a predictor of postoperative cardiopulmonary complications in elderly patients undergoing pulmonary resection for lung cancer. Ann Thorac Surg 2011;92:1051-5. [Crossref] [PubMed]
- Lim E, Baldwin D, Beckles M, et al. Guidelines on the radical management of patients with lung cancer. Thorax 2010;65 Suppl 3:iii1-27. [Crossref] [PubMed]
- Brunelli A, Charloux A, Bolliger CT, et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur Respir J 2009;34:17-41. [Crossref] [PubMed]
- Fu D, Wu C, Li X, et al. Elevated preoperative heart rate associated with increased risk of cardiopulmonary complications after resection for lung cancer. BMC Anesthesiol 2018;18:94. [Crossref] [PubMed]
- Pfister R, Michels G, Sharp SJ, et al. Resting heart rate and incident heart failure in apparently healthy men and women in the EPIC-Norfolk study. Eur J Heart Fail 2012;14:1163-70. [Crossref] [PubMed]
- Nanchen D, Stott DJ, Gussekloo J, et al. Resting heart rate and incident heart failure and cardiovascular mortality in older adults: role of inflammation and endothelial dysfunction: the PROSPER study. Eur J Heart Fail 2013;15:581-8. [Crossref] [PubMed]
- Butler J, Kalogeropoulos A, Georgiopoulou V, et al. Incident heart failure prediction in the elderly: the health ABC heart failure score. Circ Heart Fail 2008;1:125-33. [Crossref] [PubMed]
- Zhang D, Shen X, Qi X. Resting heart rate and all-cause and cardiovascular mortality in the general population: a meta-analysis. CMAJ 2016;188:E53-63. [Crossref] [PubMed]
- Abbott TE, Ackland GL, Archbold RA, et al. Preoperative heart rate and myocardial injury after non-cardiac surgery: results of a predefined secondary analysis of the VISION study. Br J Anaesth 2016;117:172-81. [Crossref] [PubMed]
- Wong YY, Westerhof N, Ruiter G, et al. Systolic pulmonary artery pressure and heart rate are main determinants of oxygen consumption in the right ventricular myocardium of patients with idiopathic pulmonary arterial hypertension. Eur J Heart Fail 2011;13:1290-5. [Crossref] [PubMed]
- Jensen MT, Marott JL, Lange P, et al. Resting heart rate is a predictor of mortality in COPD. Eur Respir J 2013;42:341-9. [Crossref] [PubMed]
- Byrd JB, Newby DE, Anderson JA, et al. Blood pressure, heart rate, and mortality in chronic obstructive pulmonary disease: the SUMMIT trial. Eur Heart J 2018;39:3128-34. [Crossref] [PubMed]
- Okada M, Okada M, Ishii N, et al. Right ventricular ejection fraction in the preoperative risk evaluation of candidates for pulmonary resection. J Thorac Cardiovasc Surg 1996;112:364-70. [Crossref] [PubMed]
- Pierce RJ, Sharpe K, Johns J, et al. Pulmonary artery pressure and blood flow as predictors of outcome from lung cancer resection. Respirology 2005;10:620-8. [Crossref] [PubMed]
- Fee HJ, Holmes EC, Gewirtz HS, et al. Role of pulmonary vascular resistance measurements in preoperative evaluation of candidates for pulmonary resection. J Thorac Cardiovasc Surg 1978;75:519-24. [PubMed]
- Rams JJ, Harrison RW, Fry WA, et al. Operative pulmonary artery pressure measurements as a guide to postoperative management and prognosis following pneumonectomy. Dis Chest 1962;41:85-90. [Crossref] [PubMed]
- Wells JM, Washko GR, Han MK, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med 2012;367:913-21. [Crossref] [PubMed]
- Nojiri T, Maeda H, Takeuchi Y, et al. Predictive value of B-type natriuretic peptide for postoperative atrial fibrillation following pulmonary resection for lung cancer. Eur J Cardiothorac Surg 2010;37:787-91. [Crossref] [PubMed]
- Nojiri T, Yamamoto K, Maeda H, et al. A Double-Blind Placebo-Controlled Study of the Effects of Olprinone, a Specific Phosphodiesterase III Inhibitor, for Preventing Postoperative Atrial Fibrillation in Patients Undergoing Pulmonary Resection for Lung Cancer. Chest 2015;148:1285-92. [Crossref] [PubMed]


