
Effects of acute hypercapnia on cognitive function in patients undergoing bronchoscope intervention
Introduction
Surgical patients may develop postoperative cognitive impairment or reduction, such as postoperative delirium (POD) or postoperative cognitive dysfunction (POCD), especially in aged patients. The incidence range of both POD and POCD are between 8.9% percent and 46.1% (1), which may be affected by physiological as well as immunological variations, and the hereditary risk elements (2,3). Despite the fact that no biomarkers for diagnosis and prognosis of postoperative cognitive impairments are available, the central cholinergic shortage from deregulation of cholinergic anti-inflammatory pathways leading to boosted inflammation, emerged as the most significant hypothesis (4). Additionally, hyperbaric oxygen, acupuncture, and lidocaine, dexmedetomidine may be neuroprotective against postoperative cognitive impairment (5-7).
Hypercapnia may be a double-edged sword on postoperative cognitive impairment. Acute hypercapnia elevates intracranial pressure, lowers cerebral perfusion, and triggers cerebral ischemia (8,9). Nevertheless, there are numerous research works that have revealed that hypercapnia possessed neuroprotective, whereby the fundamental processes counted on decreases in excitatory amino acids degrees, rise of oxygen supply, as well as a minimization of cerebral metabolism (10). Extensive use of acute permissive hypercapnia, being a lung protective strategy, is recommended for in ventilation therapy. Furthermore, clinical data suggest that permissive hypercapnia is not likely to exert impact on the performances of patients (11). Despite some supposed neuroprotective impacts revealed by some earlier research works, hypercapnia cause by general anesthesia may also adversely affect cognitive function in the newborn rats (9). The conclusive cognitive impacts of permissive hypercapnia in medicine is still unclear.
In this research work, we studied the cognitive function of the patients that had undergone bronchoscope intervention (BI), and its association with plasma biomarkers of cholinergic anti-inflammatory pathway as well as direct neuronal damage.
Methods
Study design and patient objectives
Patients, who have undergone BIs in the period between February 2016 and December 2016, were employed from China Meitan General Hospital. The approval for the research was received from the ethics committee of China Meitan General Hospital in Beijing, China. An informed consent was signed by every patient prior to the administration of anesthesia. In case of disagreement of the patient with the blood test, the detection of the cognitive scale was still be tried. Clinical Trial Registration Identifier: ChiCTR-POC-15007483.
Every BI was carried out by the professionally expert endoscopists using electric flexible (Pentax, Japan) or rigid bronchoscope. The inclusion criteria were followed as hereunder: (I) age ≤70 years; (II) operation duration between 30 and 120 min; (III) airway impediment was less than 90 percent; and (IV) literate.
Exclusion criteria were: (I) having a history of cerebrovascular disease (for instance, stroke and heart surgery); (II) drug user and alcoholic (>1 drink/day); (III) illiterate (unable to take part in the assessment); and (IV) diagnosed with hypoxia or hypercapnia prior to the intervention.
Anesthetic settings and maintenance
During operation, patients were monitored with followings; electrocardiogram, pulse oximetry, bispectral index, percutaneous application of carbon dioxide (Transcutaneous monitoring system TCM400, Radiometer Medical Aps, Denmark) as well as arterial blood gases (ABG) analysis (blood gas analyzer, GEM Premier 3500, Instrumentation Laboratory, Lexington, MA, USA) were carried out all through the procedure.
Administration of general anesthesia was provided using fast-recovery medication, which include propofol, remifentanil, and rocuronium. Intravenous infusion of propofol and remifentanil both was administered to maintain a profound anesthetic level. Mechanical ventilation was carried out with the use of jet ventilation (Jiangxi Teli Medical Instruments, China). The respiratory rate amounted to be between 16 and 30 bpm, whereby the driving pressure stood between 40 and 60 PSI through the intervention.
If the SpO2 values amounted to be less than 90 percent or the PaCO2 values amounted to be above 100 mmHg, the endoscopists would seize interruption, followed by the performance of manual conventional ventilation. The procedure will be resumed when the PaCO2 value lowered to less than 80 mmHg.
Cognitive function tests
For the purpose of evaluating cognitive activity, every patient underwent MMSE and MoCA a day before the surgery (T0), as well as at 7 days (T7). Both MMSE and MoCA tests were carried out with the help of a sole psychologist, who was blinded to the research groups.
Serum samples
Blood specimens (3 mL) were obtained using venipuncture with a tube (vacuum system) that did not have anticoagulants by an expert. Serum was attained with the centrifugation of blood sample at 5,000 ×g for a period of 5 minutes and was stored at a freezer at a temperature of −70 °C until analysis.
Serum specimens were used to measure levels of S100B, neuron-specific enolase (NSE), interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), malondialdehyde (MDA), superoxide dismutase (SOD) prior to T0, T1 and T7.
Measurements of the degrees of S100B, NSE, IL-6 as well as TNF-α were carried out with the use of an enzyme-linked immunosorbent assay (ELISA) kit (Wanlei Biologic Company, Shenyang, China) in accordance with the instructions of the manufacturer. Determination of both MDA and SOD concentrations was carried out with the use of enzymatic approaches in adherence with the guidelines of manufacturer (Jiancheng Biologic Project Company, Nanjing, China). Every research staff wasn’t aware of the observations of the clinical analysis.
Statistical analysis
All data have been displayed as the means ± SD. Analysis of Intergroup numerical data, which includes IL-6, TNF-α, MDA, SOD, S100B as well as NSE concentrations were carried out using repeated measures ANOVA. Analysis of nominal data was carried out with the help of χ2 test. The dissimilarities between the values were regarded as being significant at P<0.05. Each and every statistical test and graph was carried out with the use of Statistical Program for Social Sciences 20.0 software (SPSS, Inc., Chicago, IL, USA).
Results
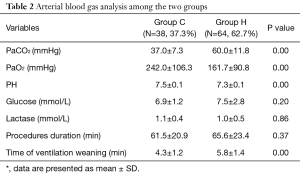
A total of 102 patients registered for this research work had accomplished cognitive tests; with 64 patients (62.7%, 64/102) possessing moderate hypercapnia all through BI. Thirty-six patients completed collection of blood specimens, including 20 patients who had developed moderate hypercapnia. Presentation of the demographic data has been made in the Tables 1,2. No significant differences were observed in age, body weight, male, education, diabetes mellitus, coronary heart disease (CHD), chronic obstructive pulmonary disease (COPD), and operation duration between the two groups. In respect of recovery time exit ed substantial dissimilarities. In accordance with artery blood specimens test, blood glucose and lactase both exhibited no considerable dissimilarities (see Table 2).

Full table
Full table
MMSE as well as MoCA tests was carried out at pre-operation and 7 days after operation. In comparison with the preoperative MMSE scores, Group Hypercapnia (Group H) on 7 days after surgery, exhibited a significant increase (P=0.00). Nevertheless, the MMSE scores in Group H didn’t exhibit higher increase as compared with that in the Group H (P=0.11). In comparison with the preoperative MoCA scores, Group H on T7 subsequent to surgery exhibited a significant increase (P=0.00). Meanwhile, the MoCA scores in Group H exhibited considerably higher increase as compared with that in the Group C (P=0.01) (see Table 3).

Full table
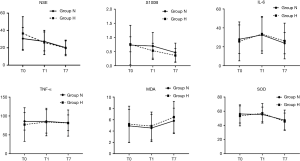
Analyses of IL-6, TNF-α, MDA, SOD, S100B as well as NSE concentrations were carried out using repeated measures ANOVA. No substantial dissimilarities were observed in serum S100B and NSE levels both between Group H and Group C (P=0.23, P=0.14, correspondingly). Serum IL-6 as well as TNF-α levels shared similarity in the two groups (P=0.69, P=0.71, correspondingly). Serum SOD as well as MDA levels shared similarity in the two groups (P=0.51, P=0.95, correspondingly) (see Figure 1).
Discussion
Hypercapnia, being an intricacy of anesthesia has made appearance in different books and articles. The key purpose of anesthesia is to maintain physical and physiological homeostasis. Controlled ventilation therapy has been increased exceptionally in special surgeries, such as BI, lung volume reduction surgery, video-assisted thoracoscopy, etc. Hypercapnia frequently occurs due to hypoventilation secondary to limited airway pressure and/or tidal volume. BI, having airway stenosis, made use of the same airway with anesthesia and therapy. In addition, jet ventilation at high driving pressure increase the risk of barotrauma. To the best of our knowledge, no report is available that investigates the cognitive effects of hypoventilation in BI.
This research work primarily aimed at investigating the association of hypercapnia and cognitive activity in BI patients with the help of biochemical brain markers, and neuropsychological assessments. The key findings were hereunder: (I) moderate hypercapnia leaded to increasing cognitive function in patients who had undergone BI; (II) both S100B and NSE levels exhibited considerable similarities in the two groups. (III) both the serum IL-6 and TNF-α levels shared similarity in the two groups (P=0.69, P=0.71, correspondingly).
Typical use of MMSE as well as MoCA is made as a representation of cognitive capabilities, which include memory, attention as well as language, in addition to having been illustrated for being a meaningful instrument for evaluating cognitive activity (12). Our research work put to application both the MMSE and the MoCA in order to evaluate cognitive activity. Earlier research works illustrated that both mild and moderate hypercapnia possessed neuro-protective activity in rats, whereby the possible mechanisms were decreases in excitatory amino acids degrees, rise in oxygen supply, as well as a decrease cerebral metabolism. As discovered by our former studies, mild and moderate hypercapnia had no association with damaging outcomes. In this research work, MMSE scores in Group H in T7 exhibited considerable increase as compared with pre-operation (P=0.00), despite the fact that the MMSE scores in Group H was not to be considerably higher as compared with Group C (P=0.16). In comparison with the preoperative MoCA scores, Group H on T7 exhibited a considerable increase (P=0.00). At the same time, MoCA scores in Group H amounted to be considerably higher as compared with that in Group C (P=0.01), which suggested that mild and moderate hypercapnia augmented cognitive activity with the help of neurocognitive function tests. At the same time, MoCA possesses more sensitivity in comparison with MMSE.
Both S100B and NSE are termed as serum markers of neuronal damage, in addition to being extensively utilized in diagnosis as well as prognosis of cognitive impairment subsequent to various surgeries. As evidenced by the researches, serum concentrations of both S100 and NSE exhibit increase in the evaluation of cognitive impairment subsequent to various surgeries (13,14). Accordingly, the S100B protein discharge emerges as a reasonable contestant for assessing occurrence, methodology, as well as performance of POCD. NSE is termed as an isoenzyme of the glycolytic enzyme enolase, which is typically discovered in the cytoplasm of neurons as well as cells of neuro-endocrine demarcation. Empirical observations have revealed the fact that NSE is in line with the level of cognitive impairment (15,16). As discovered by our research work, the serum S100B protein as well as the NSE degrees exhibited a decrease on T7, meanwhile, no considerable dissimilarities were observed for the two groups. These data suggested that BI is likely to enhance cognitive function on the improvement of airway obstruction and respiratory function, while the neuroprotective impact of acute hypercapnia (60–100 mmHg) was not certain.
As suggested by the research works, the scale of inflammatory feedback is regarded as a risk element regarding cognitive dysfunction subsequent to a key surgery (17). Surgical trauma leads to the activation of the peripheral inborn immune system that furthers gives rise to the discharge of inflammatory mediators that damages cognitive activity (18). Peng et al. (17) carried out a meta-analysis for the purpose of investigating the association between POCD and inflammatory markers. As revealed by their observations, that IL-6 is likely to act as a precursor for guiding the avoidance as well as cure of POCD. Serum TNF-α level is also recommended for being a crucial mediator of inflammation stimulated neuronal dysfunction. As revealed by our findings, both IL-6 and TNF-α level did not emerge as considerable groups at the three time points researched. Findings made by us and others suggest that inflammatory feedback is likely to have responsibility for POCD. Hypercapnia is termed as the most efficient regulator of the diameter of the blood vessels. Hypercapnia, being a consequence of hypoventilation, has been presented to boost blood flow in morbidly overweight patients or sepsis rats (19-21). In this research work, SOD as well as MDA levels exhibited to dissimilarities between the two groups. The latent cause leading to this phenomenon could suggest that short-term acute hypercapnia exposure enhances cerebral oxygenation in response to hypoxia.
This study holds numerous constraints. First, the effect of hypercapnia on cognitive function may be confounded by the changes of blood oxygen level. Hypoxia is usually defined PaO2 <60 by most previous studies. The average PaO2 in the Group H was 161.7 and did not reach the level of significant hypoxia. The reason was that PaO2 in hypercapnia group was significantly lower than control group (161.7±90.8 vs. 242.0±106.3), but both were at the levels above physiological range and less likely to contribute to the cognitive function changes. Overall, the finding in ABG (Table 2) suggested that hypercapnia, but not hypoxia, may contribute to changes of cognitive function. Secondly the number of plasma specimens was quite small, which was likely to exert impact on the observations. Accordingly, there appeared a requirement to carry out prospective thorough growth as well as assessment with long-term and stern hypercapnia. Thirdly, the graveness as well as the time period of hypercapnia required being brought under control for the purpose of making the changes of cognitive tests and plasma markers as less. Ultimately, the source of our conclusion was the patients that had BI subjected to general anesthesia. This conclusion should not recommend to other patients.
To conclude, mild and moderate hypercapnia augmented cognitive activity with the help of MMSE tests and MoCA tests, whereby the latent reasons are not sure. As suggested by this research work, hypercapnia up to 100 mmHg during anesthesia is less likely to contribute to cognitive dysfunction. Mild hypercapnia for short time is during BI is less likely to cause severe mental adverse outcome.
Acknowledgements
Funding: This paper was supported by Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding (code: Z Y L X 2 0 1 8 1 0).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The approval for the research was received from the ethics committee of China Meitan General Hospital in Beijing, China (No. K14-27). An informed consent was signed by every patient prior to the administration of anesthesia.
References
- Benson RA, Ozdemir BA, Matthews D, et al. A systematic review of postoperative cognitive decline following open and endovascular aortic aneurysm surgery. Ann R Coll Surg Engl 2017;99:97-100. [Crossref] [PubMed]
- Qiao Y, Feng H, Zhao T, et al. Postoperative cognitive dysfunction after inhalational anesthesia in elderly patients undergoing major surgery: the influence of anesthetic technique, cerebral injury and systemic inflammation. BMC Anesthesiol 2015;15:154. [Crossref] [PubMed]
- Androsova G, Krause R, Winterer G, et al. Biomarkers of postoperative delirium and cognitive dysfunction. Front Aging Neurosci 2015;7:112. [Crossref] [PubMed]
- Inouye SK. Delirium in older persons. N Engl J Med 2006;354:1157-65. [Crossref] [PubMed]
- Brown C 4th, Deiner S. Perioperative cognitive protection. Br J Anaesth 2016;117:iii52-61. [Crossref] [PubMed]
- Zhou C, Zhu Y, Liu Z, et al. Effect of dexmedetomidine on postoperative cognitive dysfunction in elderly patients after general anaesthesia: A meta-analysis. J Int Med Res 2016;44:1182-90. [Crossref] [PubMed]
- Gholipour Baradari A, Habibi MR, Habibi V, et al. Administration of lidocaine to prevent cognitive deficit in patients undergoing coronary artery bypass grafting and valve plasty: a systematic review and meta-analysis. Expert Rev Clin Pharmacol 2017;10:179-85. [Crossref] [PubMed]
- Marshall O, Chawla S, Lu H, et al. Cerebral blood flow modulation insufficiency in brain networks in multiple sclerosis: A hypercapnia MRI study. J Cereb Blood Flow Metab 2016;36:2087-95. [Crossref] [PubMed]
- Zhou Q, Cao B, Niu L, et al. Effects of permissive hypercapnia on transient global cerebral ischemia-reperfusion injury in rats. Anesthesiology 2010;112:288-97. [Crossref] [PubMed]
- Glodzik L, Randall C, Rusinek H, et al. Cerebrovascular reactivity to carbon dioxide in Alzheimer's disease. J Alzheimers Dis 2013;35:427-40. [Crossref] [PubMed]
- Cheng Q, Zhang J, Wang H, et al. Effect of Acute Hypercapnia on Outcomes and Predictive Risk Factors for Complications among Patients Receiving Bronchoscopic Interventions under General Anesthesia. PLoS One 2015;10:e0130771. [Crossref] [PubMed]
- Cooley SA, Heaps JM, Bolzenius JD, et al. Longitudinal Change in Performance on the Montreal Cognitive Assessment in Older Adults. Clin Neuropsychol 2015;29:824-35. [Crossref] [PubMed]
- Kok WF, Koerts J, Tucha O, et al. Neuronal damage biomarkers in the identification of patients at risk of long-term postoperative cognitive dysfunction after cardiac surgery. Anaesthesia 2017;72:359-69. [Crossref] [PubMed]
- Olsson B, Lautner R, Andreasson U, et al. CSF and blood biomarkers for the diagnosis of Alzheimer's disease: a systematic review and meta-analysis. Lancet Neurol 2016;15:673-84. [Crossref] [PubMed]
- Xu JH, Zhang TZ, Peng XF, et al. Effects of sevoflurane before cardiopulmonary bypass on cerebral oxygen balance and early postoperative cognitive dysfunction. Neurol Sci 2013;34:2123-9. [Crossref] [PubMed]
- Goncalves CA, Leite MC, Nardin P. Biological and methodological features of the measurement of S100B, a putative marker of brain injury. Clin Biochem 2008;41:755-63. [Crossref] [PubMed]
- Peng L, Xu L, Ouyang W. Role of peripheral inflammatory markers in postoperative cognitive dysfunction (POCD): a meta-analysis. PLoS One 2013;8:e79624. [Crossref] [PubMed]
- Terrando N, Eriksson LI, Ryu JK, et al. Resolving postoperative neuroinflammation and cognitive decline. Ann Neurol 2011;70:986-95. [Crossref] [PubMed]
- Hager H, Reddy D, Mandadi G, et al. Hypercapnia improves tissue oxygenation in morbidly obese surgical patients. Anesth Analg 2006;103:677-81. [Crossref] [PubMed]
- Stubs CC, Picker O, Schulz J, et al. Acute, short-term hypercapnia improves microvascular oxygenation of the colon in an animal model of sepsis. Microvasc Res 2013;90:180-6. [Crossref] [PubMed]
- Rupp T, Esteve F, Bouzat P, et al. Cerebral hemodynamic and ventilatory responses to hypoxia, hypercapnia, and hypocapnia during 5 days at 4,350 m. J Cereb Blood Flow Metab 2014;34:52-60. [Crossref] [PubMed]


