Robotic-assisted right medial and anterior basal segmentectomy (S7+S8)
Introduction
Thoracoscopic S7+S8 segmentectomy is one of the most challenging anatomical segmentectomies. There are few reports on S7+S8 segmentectomy (1). Robotic-assisted thoracic surgery (RATS) is theoretically better than video-assisted thoracic surgery (VATS) in 3D visualization and improved maneuverability and ergonomics, which could simplify the dissection of the vessels and bronchus and make it easier to perform an anatomical segmentectomy (2-5). Robotic pulmonary resection has been proven to be a feasible and safe alternative to traditional thoracoscopic pulmonary resection of lung cancer (6). We have accomplished over 1,000 cases of robotic pulmonary resections with nearly 10-year experience of robotic thoracic surgery. Here we present a sequential three-arm robotic-assisted technique to perform an S7+S8 segmentectomy.
Clinical vignette
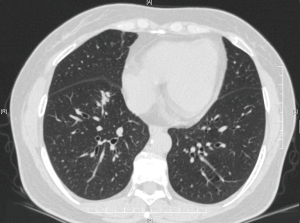
A 54-year-old lady, non-smoker, was admitted to our division with a 17 mm × 12 mm mixed ground glass nodule located in the right lower lobe (Figure 1) which had increased in size in the past 3 months. The pathology was hard to obtain before surgery due to the nodule’s location. No remarkable past medical history or family history. Preoperative pulmonary function test showed forced expiratory volume in 1 s (FEV1) was 1,520 mL, and FEV percentage in 1 s was 60.2%. In order to preserve as much pulmonary function as possible, we scheduled her for robotic S7+S8 segmentectomy (Figure 2).

Preference cards
- 3D high-definition camera (30° lens).
- One Cadiere Forceps: help to retract the vessels and bronchus to facilitate dissection fully.
- One Permanent Cautery Hook (EndoWrist Monopolar Cautery).
- One long double joint oval forceps: help to retract the lung parenchyma.
- One long dissecting forceps: used for blunt dissection around vessels or bronchus.
- ECHELON FLEX™ ENDOPATH® Staplers with a 45 mm reload.
Surgical technique
Patient positioning
The procedure was performed with the patient in the general anesthesia and lateral decubitus position. The da Vinci S Robotic Surgical System (Intuitive Surgical, Inc., Mountain View, CA) was positioned at the head of the patient.
Port placement
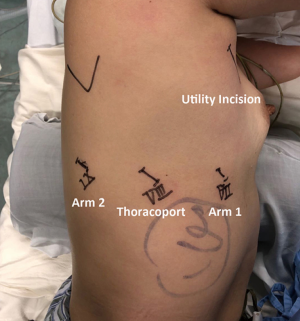
First, a 12 mm Thoracoport was made at the eighth ICS posterior axillary line, and then the camera was introduced to explore the thoracic cavity. Then two 8 mm port incisions were symmetrically made at the seventh ICS mid-axillary line (arm 1) and ninth ICS infrascapular line (arm 2) separately, and a 4 cm utility incision was made at fourth ICS anterior axillary line protected with a soft tissue retractor. After docking the robot, a 30° stereoscopic camera was firstly introduced, and then a Cardiere forceps and a permanent cautery hook were introduced separately through arm 2 and arm 1. The bedside assistant was sitting at the ventral side of the patient with a long suction tip and a long double joint oval forceps to help retract the lung and expose the surgical fields (Figure 3).
Right S7+S8 segmentectomy
- Major fissure and basal segmental pulmonary artery:
- A double joint oval clamp was inserted through the utility incision to grip the right upper lobe and retract it cranially, and a suction tip was inserted to help further expose the major fissure at the same time;
- Complete the posterior part of major fissure from the confluence of the fissures with the hook and all the way down to posterior hilum;
- Dissect the level 11 lymph nodes to expose the basal segmental pulmonary artery;
- Dissect the level 12 lymph nodes between A6, A9+A10, and A7+A8;
- Complete the anterior part of major fissure;
- Fully isolate A7+A8.
- Basal segmental pulmonary vein:
- A double joint oval clamps was inserted through the utility incision to grip the right lower lobe and retract it vertically and dorsally;
- Open the pleura over the inferior pulmonary vein and proceed distally to expose it fully, and identify V6, V7+V8, and V9+V10;
- Isolate V7+V8, and transect it with stapler through the utility incision by the assistant.
- Basal segmental bronchus:
- A double joint oval clamps was inserted through the utility incision to grip the right lower lobe and retract it caudally and dorsally;
- Transect A7+A8 to expose basal segmental bronchus;
- Identify B7+B8 and B9+B10;
- Fully isolate B7+B8, and transect it with stapler through the utility incision by the assistant.
- Intersegmental plane and specimen retrieval:
- Re-inflate the whole lung and demarcate the intersegmental plane with the hook;
- Divide the S7+S8 parenchyma along the demarcation with staplers through the utility incision;
- Pull out the lung with a specimen retrieval bag through the utility incision.
Total skin-to-skin time was 75 min, and blood loss was less than 100 mL. The chest tube was removed on post-operative (PO) day 3 and the patient was discharged on PO day 3.
Discussion
- The utility incision provides enough space for the assistant to use two instruments at the same time, which is crucial to the success of the surgery;
- With our technique, we could manage all the divisions through the utility incision, instead of taking out one of the trocars which could significantly increase the operative time;
- Long dissecting forceps could be used for blunt dissection of vessels and bronchus when needed, even though most of them could be fully isolated with the Cardiere forceps and cautery hook;
- Isolate the vessels and bronchus long enough when the angulation is unsatisfactory so that all the structures could be processed with staplers.
Conclusions
Anatomical S7+S8 segmentectomy is challenging mainly because the branches of basal pulmonary vessels and bronchus lie deeply in the parenchyma, which makes it hard to isolate them, especially in a minimally invasive way entirely. With the 3D vision, the surgeon could identify the structure in the operative fields, and with better maneuverability and ergonomics, RATS has a better performance in dissecting the lymph nodes over VATS especially with intersegmental ones. We always identify all the segmental structures first before we transect them with staplers, and isolate them long enough to facilitate the staplers.
In conclusion, RATS S7+S8 segmentectomy is safe and feasible.
Acknowledgements
Funding: This work was supported by the Shanghai Hospital Development Center Grant (SHDC12016113).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hiebinger A, Weik T, Mertins H, et al. Video-assisted thoracoscopic surgery (VATS) lower lobe bisegmentectomy (S7/8) for a central pulmonary metastasis. J Thorac Dis 2017;9:3296-8. [Crossref] [PubMed]
- Veronesi G, Novellis P, Voulaz E, et al. Robot-assisted surgery for lung cancer: State of the art and perspectives. Lung Cancer 2016;101:28-34. [Crossref] [PubMed]
- Veronesi G. Robotic lobectomy and segmentectomy for lung cancer: results and operating technique. J Thorac Dis 2015;7:S122-30. [PubMed]
- Demir A, Ayalp K, Ozkan B, et al. Robotic and video-assisted thoracic surgery lung segmentectomy for malignant and benign lesions. Interact Cardiovasc Thorac Surg 2015;20:304-9. [Crossref] [PubMed]
- Pardolesi A, Park B, Petrella F, et al. Robotic anatomic segmentectomy of the lung: technical aspects and initial results. Ann Thorac Surg 2012;94:929-34. [Crossref] [PubMed]
- Liang H, Liang W, Zhao L, et al. Robotic versus video-assisted lobectomy/segmentectomy for lung cancer: a meta-analysis. Ann Surg 2018;268:254-9. [Crossref] [PubMed]
- Li JT, Huang J, Luo QQ. Edited right medial and anterior basal segmentectomy (S7+S8). Asvide 2019;6:012. Available online: http://www.asvide.com/article/view/29625