
The AMAGAMI technique: an easy technique to achieve precise stapling in thoracoscopic segmentectomy
Introduction
As the number of patients presenting with small nodules in the lung (such as ground glass opacity nodules) increases, the demand for sublobar lung resection procedures such as wedge resection and segmentectomy is also increasing. Compared with wedge resection, anatomical segmentectomy tends to be more complicated and technically demanding, especially in completely thoracoscopic approaches. To overcome such technical challenges, the appropriate use of a surgical stapler is very valuable. As postoperative air leakage remains a major obstacle to the success of segmentectomy, a good stapling technique has a substantial impact on the patient’s postoperative course. Moreover, appropriate stapling along the ideal resection line is critical in obtaining sufficient resection margins. In this technical note, we introduce the AMAGAMI technique, which enables the highly effective use of staplers in thoracoscopic anatomical segmentectomy.
The AMAGAMI technique
“AMAGAMI” is a word produced by the combination of two Japanese words: “AMAI”, an adjunct meaning incomplete, and “GAMI”, which was transformed from the verb “KAMU”, meaning to bite or grasp. Incomplete grasping of lung tissue by a stapler, especially the Powered Echelon Flex® (Ethicon, Tokyo, Japan), enables subtle adjustment of the alignment between the stapler and the lung tissue.
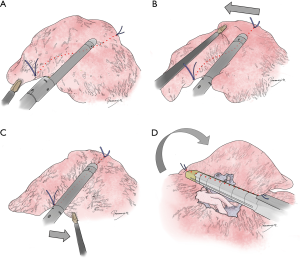
In segmentectomy, a stapler is usually opened in the thoracic cavity, moved to the ideal resection line on the lung tissue, locked by completely grasping the lung tissue, and then fired. In the AMAGAMI technique, the stapler is instead first set on the lung tissue, not necessarily on the ideal resection line, but on an easily accessible position with adequate visualization (Figures 1,2A). The lung tissue is gently grasped by the stapler, but the stapler is not locked. Forceps are then used to easily slide the lung tissue toward the ideal resection line, usually without moving or completely opening the stapler (Figure 2B). This maneuver can be repeated to adjust the alignment between the stapler and the lung tissue (Figure 2C). Once satisfactory alignment has been achieved, the lung is flipped over or the angle of the thoracoscope is changed to visualize the other side of the lung (Figure 2D). The alignment between the stapler and the resection line is then further adjusted before the stapler is fired.

The AMAGAMI technique enables surgeons to hold the lung tissue with a stapler while still being able to mobilize or slide the lung tissue under the stapler to adjust it to the ideal position. In thoracoscopic lung resection, mobilization of a stapler in the limited space of the thorax within a limited field of vision is sometimes challenging. Moreover, only a limited number of forceps or instruments are available in the thorax, especially if a reduced-port approach is employed. The advantage of the AMAGAMI technique is that the lung tissue rather than the stapler is mobilized in the limited space, so that the “bulky” stapler does not interfere with the limited thoracoscopic view. Moreover, atraumatic holding of the lung tissue by the stapler reduces the number of forceps required to attain the ideal alignment between the stapler and the lung tissue; only one instrument in addition to a stapler is needed to do this.
Standing stitches enhance the utility of the AMAGAMI technique
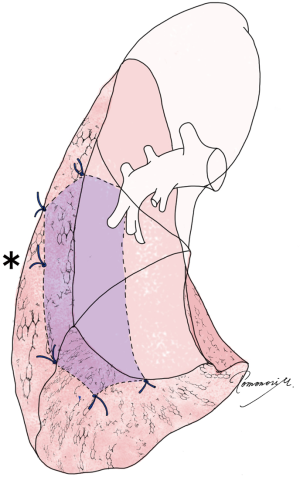
To use the AMAGAMI technique in thoracoscopic anatomical segmentectomy, visualization of the ideal resection line to be aligned with the stapler is very important. To visualize the ideal resection line on the lung, we suggest placing “standing stitches” along the staple line before performing the resection (2). As described previously, standing stitches are stitches placed along intersegmental lines using monofilament suture such as 3-0 proline, with about 1 cm left to enable later visualization (2). The advantage of standing stitches is easy visibility under limited thoracoscopic vision, even from a tangential angle, as the stitches stand out from the lung surface. The standing stitches are very helpful during stapling, as they indicate the appropriate direction of the stapler (Figure 2). The stitches are typically placed at the corner of the targeted segment to be visualized from both sides of the lung at stapling (Figure 3). Additional stitches (asterisks in Figure 3) can be placed if the staple line is long, and a landmark between stitches is helpful. If necessary, additional stitches can be placed even after the stapling procedure is initiated.
There are several different methods used to identify appropriate resection lines in segmentectomies (i.e., intersegmental lines), including but not limited to development of inflation-deflation lines (3), intravenous injection of indocyanine green (4), and virtual-assisted lung mapping (VAL-MAP) (5,6). We prefer using VAL-MAP, a bronchoscopic multi-spot preoperative dye marking technique, as VAL-MAP enables the attainment of sufficient resection margins in lung resection beyond the conventional anatomical segment (2). Regardless of the technique used to identify intersegmental lines, standing stitches should be placed in accordance with the ideal resection lines of the patient.
We have documented the techniques used for stapler-based thoracoscopic segmentectomy, and classified them into three different levels in accordance with the degree of difficulty in stapling. From least to most challenging, these techniques are: linear or Mercedes-Benz mark stapling, U- or V-shaped stapling, and three-dimensional stapling involving the basal segments (2). We have also described the technique for S10 segmentectomy and its variants, as this type of segmentectomy is particularly challenging among the segmentectomy procedures requiring three-dimensional stapling (7). In our experience, this AMAGAMI technique becomes more helpful as the degree of difficulty in stapling increases, such as in three-dimensional stapling. The advantage of the AMAGAMI technique is also better recognized in reduced-portal or uniportal thoracoscopic surgery where visualization and the number of usable instruments is limited. In circumstances such as uniportal thoracoscopic S10 segmentectomy, we consider the use of the AMAGAMI technique in combination with standing stitches to be almost mandatory.
In conclusion, the AMAGAMI technique is a simple maneuver involving a surgical stapler and the lung tissue, which substantially enhances the accuracy and surgeons’ comfort during stapling in pulmonary anatomical segmentectomy, especially in combination with standing stitches. This is particularly useful in difficult and complex anatomical segmentectomy and reduced-portal or uniportal thoracoscopic approaches.
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sato M, Murayama T, Nakajima J. Representative examples of “standing stitches” and the “AMAGAMI” technique are shown in the video. Asvide 2019;6:022. Available online: http://www.asvide.com/article/view/29637
- Sato M, Murayama T, Nakajima J. Techniques of stapler-based navigational thoracoscopic segmentectomy using virtual assisted lung mapping (VAL-MAP). J Thorac Dis 2016;8:S716-30. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Misaki N, Chang SS, Igai H, et al. New clinically applicable method for visualizing adjacent lung segments using an infrared thoracoscopy system. J Thorac Cardiovasc Surg 2010;140:752-6. [Crossref] [PubMed]
- Sato M, Omasa M, Chen F, et al. Use of virtual assisted lung mapping (VAL-MAP), a bronchoscopic multispot dye-marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J Thorac Cardiovasc Surg 2014;147:1813-9. [Crossref] [PubMed]
- Sato M, Kuwata T, Yamanashi K, et al. Safety and reproducibility of virtual-assisted lung mapping: a multicentre study in Japan. Eur J Cardiothorac Surg 2017;51:861-8. [PubMed]
- Sato M, Murayama T, Nakajima J. Thoracoscopic stapler-based “bidirectional” segmentectomy for posterior basal segment (S10) and its variants. J Thorac Dis 2018;10:S1179-86. [Crossref] [PubMed]


