A propensity score analysis on the effect of on-pump versus off-pump coronary artery bypass grafting for patients with coronary artery disease
Introduction
Coronary artery diseases (CAD) are very common (1,2), and cause a significant morbidity and mortality in patients with severe stenosis of coronary artery (1-4). Medical therapy confers a poor survival advantage relative to surgical revascularization in some severe CAD patients. Coronary artery bypass grafting (CABG) is indicated for patients with severe stenosis of coronary artery (2), and can be finished by conventional on pump CABG (ONCABG) with cardiopulmonary bypass or off pump CABG (OPCABG) (1,5,6).
OPCABG is now an established procedure, recent studies show OPCABG reduced early operative mortality and the incidences of major complications in redo CABG (7), but it appears not to increase mid-term major adverse cardiovascular and cerebrovascular events over ONCABG (1). There is no conclusion on which option is better than other. Moreover, the studies on OPCABG have reported on relative small cohorts of patients and have lacked statistical adjustment to reduce the differences in selection bias (8). In order to reduce the selection bias, we used a propensity score matching analysis to evaluate the early outcomes of OPCABG versus ONCABG in a consecutive cohort of CAD patients during four years periods.
Materials and methods
Patient selection
This was a retrospective, observational cohort study of data from consecutive CAD patients who underwent CABG at the China-Japan Friendship Hospital between April 2010 and March 2014. The study followed the China-Japan Friendship Hospital ethical and legal requirements, and individual written consent was obtained for surgical management and related medical study.
Inclusion conditions were patients who underwent CABG with complete medical document, the exclusion conditions were those who underwent concomitant percutaneous coronary intervention or carotid thromboendarterectomy (2-4). Surgical procedure selection was at discretion of the operating surgeon. The resulting base sample contained detailed clinical information on 290 patients, including 192 (66.2%) undergoing OPCABG and 98 (33.8%) undergoing ONCABG. A propensity score matching analysis was used to minimize the impact of treatment selection bias and potential confounding, 54 patients who underwent OPCABG were matched with 54 patients who underwent ONCABG.
Definitions
Critical CAD disease was defined as a stenosis of greater than 50% of lumen based on a preoperative coronary angiogram. In-hospital mortality was all deaths after surgery occurring in hospital regardless of time after surgery. A postoperative myocardial infarction (MI) was diagnosed if new Q waves longer than 0.04 ms or a reduction in R waves greater than 25% in at least two continuous leads appear on electrocardiography. Stroke was defined as new onset of global or focal brain injury that persisted for over 72 hours. Acute postoperative renal failure was defined as new requirement of hemodialysis or an elevated creatinine level 50% or greater over baseline preoperative value or >200 mmol/L. Infection was defined septicemia, sternal or leg wound infections after harvesting of great saphenous veins or sternotomy with a positive culture and requiring antibiotics (9).
Surgical management
The heart was exposed via a median sternotomy, proximal aortic atheromathous disorder was palpated manually, and the anastomotic site was tailored to avoid atherosclerotic part. Cardiopulmonary bypass (CPB) was established in a standardized manner with mild hypothermia and a roller pump. For patients undergoing ONCABG, CBP was instituted with the use of ascending aortic cannulation and 2-stage venous cannulation of the right atrium. The proximal anastomosis to the ascending aorta was constructed during a single cross clamp period. Myocardial protection was achieved with intermittent hyperkalemic antegrade warm blood cardioplegia. For OPCABG surgery, the up-to-date stabilizing retractor was used. Distal anastomosis was routinely constructed after proximal anastomosis. During surgery, heparin at 300 IU/kg for the ONCABG and 150 IU/Kg for the OPCABG were used. Activated clotting time was maintained over 480 s for ONCABG and over 300 s for OPCABG. The effect of heparin was reversed with protamine sulphate at 1:1 ratio. At the end of surgery, patients were transferred to the intensive care unit (ICU), a standardized protocol for immediate postoperative care was followed in ICU (10). Outcomes of care observed include reoperation for bleeding, hospital death, stroke, renal failure, and new MI.
Statistical analysis
A nonparsimonious multiple logistic regression analysis was used to determine the propensity for CABG. A propensity score was estimated from the logistic equation for each patient, and was used to match OPCABG patients with those undergoing ONCABG (1:1 match). Independent risk factors for in-hospital mortality were identified by a stepwise, multivariable logistic regression modeling. Table 1 shows all baseline characteristics of covariates under consideration for models. All P values are reported as 2-sided. All statistical analyses were performed. A SPSS statistical software (version 13.0; IBM Corporation, Armonk, NY, USA) and R statistical software were used for study. The Kolmogorov-Smirnov test was used to check for normality of data in the two groups initially. Continuous data were expressed as mean ± SD, and categoric data were expressed as percentages.
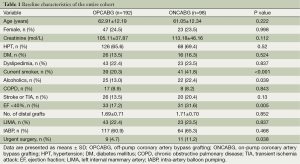
Full table
Differences between groups were compared with the chi-square statistic test for categoric variables and students’ t-tests for continuous variables.
Results
Table 1 shows the baseline characteristics of patients with CAD, 192 patients (66.2%) with CAD underwent OPCABG; 98 patients (33.8%) underwent ONCABG. Compared with the OPCABG group, patients in ONCABG group had a higher prevalence of smoking and alcohol consumption, and lower ejection fraction less than 40% (P<0.05). In addition, patients undergoing ONCABG were more likely received urgent operation (P=0.038). There was no difference in the use of bilateral internal mammary artery between the two groups (P>0.05).
After propensity score matching, 54 pairs of patients were matched (Table 2). In the matched cohorts, no significant difference between the two groups for any covariate was observed. Patients undergoing OPCABG had a lower needs for postoperative intra-aortic balloon pump, but it did not reach a significant difference (P>0.05, Table 2).
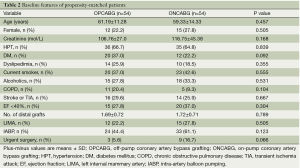
Full table
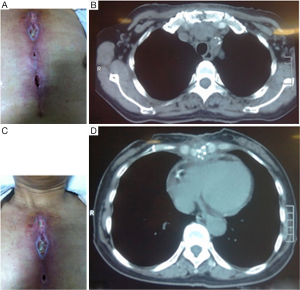
Table 3 indicates that the incidence of postoperative MI in OPCABG group was lower than ONCABG group(3.7% vs. 14.8%, P=0.046), and other clinical outcomes of propensity matched patients were similar in both groups, including rates of blood transfusion, ICU stay and postoperative hospital stay, reoperation rate and hospital mortality. The incidence of wound infection in OPCABG group was higher than in ONCABG group (13% vs. 7.4%, P=0.34). One of the most common organisms cultured from the infected chest wounds was Staphylococcus aureus. Patients with wound infection had a poor healing of the sternal wound and wound dehiscence (Figure 1). The multivariate analysis revealed that a postoperative MI was an independent risk factor for surgical revascularization (odds ratio, 3.4; 95% CI: 0.45-1.09, P=0.046).
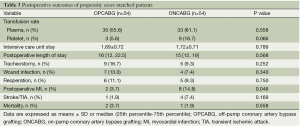
Full table
Discussion
Our propensity score analysis study demonstrates that OPCABG is safe for patients with coronary artery disease and is associated with lower postoperative MI incidence and similar perioperative complications and hospital mortality with respect to ONCABG.
There are controversies about the possible benefits of OPCABG compared to ONCABG. Some institutes still use the ONCABG technique to treat severe CAD patients currently, the main reason is the hemodynamic instability that may occur in performing revascularization on a beating heart. Recent studies show that OPCABG resulted in significantly lower patency rate for arterial and saphenous vein graft conduits, and less effective revascularization than ONCABG. At one year after surgery, patients with less effective revascularization had higher adverse event rates (5). A meta analysis suggest that OPCABG may increase late all-cause mortality by a factor of 1.37 over ONCABG (11). Randomized controlled trials did not find, except for atrial fibrillation, the statistically significant reductions in short-term mortality and morbidity (12). Moreover, one systematic review did not demonstrate any significant benefit of OPCABG compared with ONCABG regarding mortality, stroke, or MI. In contrast, patients in ONCABG group had a better long-term survival (13). In another randomized study, a total of 2539 patients 75 years of age or older were randomly assigned for elective first-time CABG to undergo OPCABG or ONCABG, there was no significant difference between two groups with regard to the composite outcome of death, stroke, MI, repeat revascularization, or new renal-replacement therapy within 30 days and within 12 months after surgery (14).
In order to reduce the patient selection bias, we used propensity score analysis in this study. Our study results were consistent with the data reported (6,9,15-17). The randomized trial and observational study show OPCABG now becomes an established procedure with results comparable to ONCABG, both procedures were associated with similar early and late graft patency, incidence of recurrent or residual myocardial ischemia, need for reintervention, long-term survival, and the similar late mortality (6,9,15-17). Moreover, in comparison to ONCABG, Meta analysis demonstrates that OPCABG reduces the incidence of post-operative stroke and has no substantial effect on mortality or MI (18). Furthermore, other studies showed that OPCABG significantly reduces perioperative mortality with long-term good outcome (19-21). Use of CPB is an independent predictor of in-hospital mortality (14).
Complete revascularization remains the gold standard of CABG. The main goal of surgical revascularization is to reestablish the blood supply to the ischemic cardiac region and to prevent MI (22). One of the great concerns is the early graft patency with OPCABG did not match the excellent outcomes of conventional ONCABG (5,11). The postoperative MI in OPCABG group was higher than in OCCPB group, which might be induced by the blocked graft, as coronary angiography could not be performed in all patients with postoperative MI to verify the presence of blocked graft, it is difficult to assure the graft patency rate in CABG patients. Another concern regarding OPCABG is possible reduced quality of anastomosis on beating heart. As a patient with complete revascularization is more likely free from severe angina than one with incomplete revascularization (22).
The surgical options for ischemic heart disease should be tailed individually to optimize the benefits and minimize the risk of adverse effects, the surgeon should consider bypass options and bypass graft conduit to maximize the long-term benefits of coronary revascularization while minimizing the risks (6,23).
The cause of wound infection in our study is most likely due to the jeopardized immunity of patients leading to the growth of bacteria such as staphylococcus in surgical area, and poor healing of sternal wound and surgical wounds (24) (Figure 1). The preventive approach is to observe the sterilization rule carefully to sterilize the surgical wound area and use antibiotics prophylactically (24).
Study limitations
This is an observational retrospective study rather than a randomized controlled trial; even though a propensity score matched analysis was used in this study, it still has some limitations. Only perioperative outcomes but not long-term follow up results are reported, and data on surgical revascularization rates and graft patency following surgery are not available. There is no report on the degree of stenosis of carotid artery, which is associated with stroke before or after CABG. Long-term follow-up of patients from current study will offer additional evidence.
Overall, our propensity score matching showed that patients in OPCABG group had lower postoperative MI incidence and similar other clinical outcomes in comparison with those in ONCABG group. The short-term effect of OPCABG was similar to that of ONCABG. Based on the current evidence, ONCABG should continue to be the standard surgical option. Yet, OPCABG may be an alternative when there are contraindications for cannulation of the aorta and CPB. Further long-term follow up and randomised clinical trials are warranted to address the optimal treatment.
Acknowledgements
Dr. Ren is the guarantor for this article, designed and wrote this article, and takes responsibility for the integrity of the work as a whole. We thank Dr. Junni Zhang for the statistical analysis, and Mrs Chaozeng Si and Tieshan Zhang for their kind assistance in collecting clinical data. This article was partially supported by China International Cooperation Grant (No. 2013DFA31900).
Disclosure: The authors declare no conflict of interest.
References
- Takagi H, Watanabe T, Mizuno Y, et al. A meta-analysis of large randomized trials for mid-term major cardio- and cerebrovascular events following off-pump versus on-pump coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2014;18:522-4. [PubMed]
- Ren S, Liu P, Ma G, et al. Long-term outcomes of synchronous carotid endarterectomy and coronary artery bypass grafting versus solely carotid endarterectomy. Ann Thorac Cardiovasc Surg 2012;18:228-35. [PubMed]
- Ren S, Fan X, Peng L, et al. Expression of NF-κB, CD68 and CD105 in carotid atherosclerotic plaque. J Thorac Dis 2013;5:771-6. [PubMed]
- Ren S, Li X, Wen J, et al. Systematic review of randomized controlled trials of different types of patch materials during carotid endarterectomy. PLoS One 2013;8:e55050. [PubMed]
- Hattler B, Messenger JC, Shroyer AL, et al. Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: Results from the Veterans Affairs Randomized On/Off Bypass (ROOBY) trial. Circulation 2012;125:2827-35. [PubMed]
- Lu JC, Grayson AD, Pullan DM. On-pump versus off-pump surgical revascularization for left main stem stenosis: risk adjusted outcomes. Ann Thorac Surg 2005;80:136-42. [PubMed]
- Dohi M, Miyata H, Doi K, et al. The off-pump technique in redo coronary artery bypass grafting reduces mortality and major morbidities: propensity score analysis of data from the Japan Cardiovascular Surgery Database. Eur J Cardiothorac Surg 2014. [Epub ahead of print]. [PubMed]
- Börgermann J, Hakim K, Renner A, et al. Clampless off-pump versus conventional coronary artery revascularization: a propensity score analysis of 788 patients. Circulation 2012;126:S176-82. [PubMed]
- Yeatman M, Caputo M, Ascione R, et al. Off-pump coronary artery bypass surgery for critical left main stem disease: safety, efficacy and outcome. Eur J Cardiothorac Surg 2001;19:239-44. [PubMed]
- Yeatman M, Caputo M, Narayan P, et al. Magnesium-supplemented warm blood cardioplegia in patients undergoing coronary artery revascularization. Ann Thorac Surg 2002;73:112-8. [PubMed]
- Takagi H, Matsui M, Umemoto T. Off-pump coronary artery bypass may increase late mortality: a meta-analysis of randomized trials. Ann Thorac Surg 2010;89:1881-8. [PubMed]
- Wijeysundera DN, Beattie WS, Djaiani G, et al. Off-pump coronary artery surgery for reducing mortality and morbidity: meta-analysis of randomized and observational studies. J Am Coll Cardiol 2005;46:872-82. [PubMed]
- Møller CH, Penninga L, Wetterslev J, et al. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev 2012;3:CD007224. [PubMed]
- Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013;368:1189-98. [PubMed]
- Puskas JD, Williams WH, O’Donnell R, et al. Off-pump and on-pump coronary artery bypass grafting are associated with similar graft patency, myocardial ischemia, and freedom from reintervention: long-term follow-up of a randomized trial. Ann Thorac Surg 2011;91:1836-42; discussion 1842-3.
- Fattouch K, Runza G, Moscarelli M, et al. Graft patency and late outcomes for patients with ST-segment elevation myocardial infarction who underwent coronary surgery. Perfusion 2011;26:401-8. [PubMed]
- Virani SS, Lombardi P, Tehrani H, et al. Off-pump coronary artery grafting in patients with left main coronary artery disease. J Card Surg 2005;20:537-41. [PubMed]
- Sá MP, Ferraz PE, Escobar RR, et al. Off-pump versus on-pump coronary artery bypass surgery: meta-analysis and meta-regression of 13,524 patients from randomized trials. Rev Bras Cir Cardiovasc 2012;27:631-41. [PubMed]
- Hong S, Youn YN, Yi G, et al. Long term results of ST-segment elevation myocardial infarction versus non-ST-segment elevation myocardial infarction after off-pump coronary artery bypass grafting: propensity score matching analysis. J Korean Med Sci 2012;27:153-9. [PubMed]
- Mack MJ, Brown P, Houser F, et al. On-pump versus off-pump coronary artery bypass surgery in a matched sample of women: a comparison of outcomes. Circulation 2004;110:II1-6. [PubMed]
- Godinho AS, Alves AS, Pereira AJ, et al. On-pump versus off-pump coronary-artery bypass surgery: a meta-analysis. Arq Bras Cardiol 2012;98:87-94. [PubMed]
- Yi G, Youn YN, Joo HC, et al. Association of incomplete revascularization with long-term survival after off-pump coronary artery bypass grafting. J Surg Res 2013;185:166-73. [PubMed]
- Tranbaugh RF, Dimitrova KR, Lucido DJ, et al. The second best arterial graft: a propensity analysis of the radial artery versus the free right internal thoracic artery to bypass the circumflex coronary artery. J Thorac Cardiovasc Surg 2014;147:133-40. [PubMed]
- Ren S, Sun G, Yang Y, et al. Management of concomitant large aortic aneurysm and severe stenosis of aortic arc. Ann Thorac Cardiovasc Surg 2014;20:84-7. [PubMed]


