Prof. Shaf Keshavjee: innovating lung transplantation and facing the challenges of the unknown
Editor’s note
As two of the deadliest malignancies worldwide, lung cancer and esophageal cancer remain a global concern for patients and thoracic surgeons alike. The 2018 AATS meeting, Focus on Thoracic Surgery: Lung and Esophageal Cancer, concentrated on the complex issues involved with treating both lung and esophageal malignancies, while also discussing innovative approaches for improving quality and outcomes.
This two-day program featured a mixture of lectures, relevant case studies, interactive panel discussions and videos. The faculty included local and internationally recognized medical experts in lung and esophageal disease, ensuring attendees received insights from a broad spectrum of leaders in thoracic surgery.
During the meeting, the Editorial Office of the Journal of Thoracic Disease was honored to conduct an interview with Prof. Shaf Keshavjee with the aim to not only share his knowledge and stories with peers across the world, but also to bring better a understanding regarding the developments in the field of lung transplantation.
Expert introduction
Professor Keshavjee completed his residency training at the Affiliated Hospital of Harvard University. He is currently the head of the surgical department at the University Health Network (UHN) in Canada, director of thoracic surgery of Toronto General Hospital (TGH), and director of the lung transplantation project in Toronto (Figure 1).
Professor Keshavjee focuses on the diagnosis and treatment of lung transplantation and thoracic diseases. Toronto General Hospital, where Professor Keshavjee serves, is the largest center of lung transplantation in the world and has a complete lung transplantation management system. In the field of lung transplantation, TGH has completed many first reports in the world: single lung transplantation, double lung transplantation, child lung transplantation, ex vivo lung perfusion (EVLP) and so on.
Professor Keshavjee established the EVLP Toronto system, which has become the mainstream standard of EVLP in the world. It can keep the donor lung at normal body temperature for 12 to 18 hours. Since the successful completion of the world’s first long-term survival lung transplantation in 1983, more than 2,000 cases of lung transplantation have been completed by Prof. Keshavjee, of which more than 460 cases have been treated with EVLP. He has thus won the award for American Lung Transplantation Association Innovation. In addition, he has also received two Queen Elizabeth II Diamond Jubilee Medals, was bestowed the Order of Ontario, and was awarded the country’s highest civilian honour, an appointment as an Officer of the Order of Canada.
Interview summary (Figure 2)

During the interview, when asked about which honour he is the most proud of, he said that it was being an Officer of the Order of Canada, “Because it is the highest civilian honor given by my country for achievements that impact not only Canada but the world.”
Professor Keshavjee has his own opinion on how to overcome the difficult problem of extracorporeal lung support: “with extracorporeal lung support, it gives us the opportunity to support the patient so that we can actually rest the lung. I think the important questions to ask now are: what is the best way to rest the lung, and what kind of patient is suitable for extracorporeal lung support. In a word, technological innovation has made lung transplantation easier and safer. And now it is extracorporeal lung support that enables us to do more complex surgery in various ways.” As a technique which is used to protect donor lungs of lung transplantation, there is no doubt that EVLP can provide invaluable convenience in an operation. Through EVLP, the number of safe donor lungs can be increased by evaluating the quality of donor lung, improving the quality of donor lungs, and then transplanting the assessed high-risk donor lungs successfully. “We now can take out the lungs from the bodies which support them, diagnose what’s wrong with them and treat them, and prepare them for transplantation so that there will be better chance of their lasting longer.” Professor Keshavjee said.
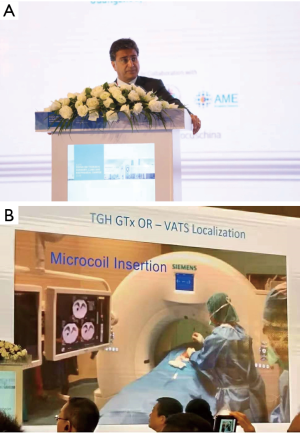
When asked about how to achieve innovative breakthroughs, Professor Keshavjee said: “As a doctor, what you do is look for challenges for problems that are not solved, and then use the research to see how can we fix the problem or how can we make it better.” As a surgeon and scientist, Professor Keshavjee believes that the most interesting thing about doing research is that the answer is always unknown. Professor Keshavjee enjoys the challenges of scientific research and all kinds of unusual results: “You have a hypothesis and you see this is likely to work, and then you get to find out if it works or not, and more often than not we’ve been successful and have been quite excited to say ‘wow, we have found it’. And the answer is going to make a difference.” Professor Keshavjee also said that their team is now committed to the field of genetic modification. Although EVLP doubled the number of lung transplantations performed by Professor Keshavjee, he does not intend to stop there. Instead, with great enthusiasm for challenges and the unknown, he hopes to make greater progress in organ repair through gene technology research (Figures 3,4).
Interview questions
- Localization of small nodules and GGOs is a difficult challenge for thoracic surgeons. Would you like to share with our readers the technique for intraoperative localization that you introduced in your presentation? What is your next step in this research?
- As a widely studied treatment in recent years, many difficulties in extracorporeal circulation operation remain to be overcome, which problem do you think is the most urgent one to be solved?
- As far as we know, you and your team are currently working on molecular diagnostic and gene therapy strategies, could you tell us something about your research progress? What could these strategies do for lung transplantation?
- You are well-known for your innovative research in disease treatment. Could you share your experience with us concerning how to achieve breakthroughs in research?
- Can you share with us any interesting things you encountered while doing your research?
- You have won many awards and honorable titles in the field. Which one you are most proud of?
Acknowledgements
We would like to express our sincerest gratitude to Prof. Shaf Keshavjee for sharing his insights and opinions with us.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Dong W. Professor Shaf Keshavjee: innovating lung transplantation and facing the challenges of the unknown. Asvide 2019;6:024. Available online: http://www.asvide.com/article/view/29639
(Science Editor: Wenbin Dong, JTD, jtd@amepc.org)
(English Language Editor: John Ayric Gray, AME Publishing Company)