
Clinical features and treatment outcomes of airway foreign body aspiration in adults
Introduction
Aspiration of foreign bodies (FBs) into the airway can be life-threatening. Patients may present with either acute symptoms like respiratory failure requiring urgent intervention or with non-life-threatening respiratory symptoms such as chronic cough, hemoptysis, dyspnea, and wheezing (1). Adult patients can remain asymptomatic for months to years leading to delayed diagnosis (2,3). Serious complications such as granulation tissue formation, recurrent pneumonia, atelectasis and endobronchial stenotic scarring can occur in cases of delayed diagnosis and removal (4,5).
Airway FBs can be successfully removed with either flexible or rigid bronchoscopy. Although the benefits of flexible bronchoscopy include ease of use, widespread availability and lack of requirement for general anesthesia, its disadvantages include difficulties in maintaining airway patency and patient cooperation. In contrast, airway patency is easily maintained with rigid bronchoscopy and a variety of rigid forceps available for FB extraction provide significant advantages. The primary limitations of rigid bronchoscopy are the need for general anesthesia and lack of availability. In pediatric patients, rigid bronchoscopy is the treatment of choice (6-9), mainly due to its ability to provide a secure airway, while 90% or more adult cases can be successfully resolved with flexible bronchoscopy at specialized centers (4,10,11). There are numerous discussions (12,13), but scarce data on what factors to consider when choosing between flexible or rigid bronchoscopy for FB removal in adults.
The aim of this study was to evaluate the clinical characteristics of adult patients with airway FBs and review the outcomes for flexible and rigid bronchoscopy. In addition, we aimed to identify factors associated with success or failure of each treatment modality.
Methods
Study population
A retrospective review of medical records was performed for all patients who underwent bronchoscopic removal of airway FBs at Samsung Medical Centre (a 1,960-bed, university affiliated, tertiary referral hospital in Seoul, Republic of Korea) between January 1999 and March 2017. Patients younger than 18 years were excluded. The study was approved by the Institutional Review Board of Samsung Medical Center (IRB No. 2017-08-033). Informed consent was waived because of the retrospective nature of the study.
Bronchoscopic procedure
Flexible bronchoscopy (Olympus, Tokyo, Japan) was performed with topical anesthesia (lidocaine) and sedatives (midazolam). Rigid bronchoscopy (Karl-Storz, Tuttlingen, Germany) under general anesthesia as the first-line modality for airway FB removal was considered in patients who had a need for airway protection due to unstable vital signs or impacted FB identified on chest imaging. Accessories used to remove airway FBs included biopsy forceps (FB-21C-1 or FB-36C-1, Olympus, Tokyo, Japan), rat tooth grasping forceps (FG-26C-1, Olympus, Tokyo, Japan), snares (SD-7C/18C-1, Olympus, Tokyo, Japan), and optical forceps (10352U, Karl-Storz, Tuttlingen, Germany).
Data collection and analysis
Demographic and baseline patient characteristics including age, sex, comorbidities, symptoms, clinical course before admission to our hospital, duration between aspiration and bronchoscopic removal of airway FBs, radiographic findings and pulmonary function test results were collected. To assess the methods of airway FB removal, we collected the following data: location and types of airway FBs, equipment used to remove airway FBs, and clinical outcomes.
Continuous variables are presented as the median and interquartile range (IQR) and were analyzed using the Mann–Whitney U test. Categorical variables are presented as numbers (percentages) and were analyzed by Pearson’s chi-square test or Fisher’s exact test. A P value less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software (IBM SPSS Statistics ver. 23, Chicago, IL, USA).
Results
Patients characteristics
During the study period, a total of 103 adult patients with airway FBs were hospitalized and underwent bronchoscopy. The baseline characteristics of the study population are summarized in Table 1. The median age was 64 years (IQR, 51–77 years) and 72 (70%) were male. Fifty-five (53%) patients had no comorbidities. The primary presenting symptoms were cough (75%), sputum production (49%), and dyspnea (36%), however, acute choking event only occurred in 5%. Fifty-eight (56%) patients presented immediately to the hospital for persistent respiratory symptoms after aspiration. The remaining 45 patients did not present to the hospital immediately, and their airway FBs were diagnosed during investigation for recurrent pneumonia (n=31), poor response to asthma treatment (n=7), or asymptomatic health screening (n=7). Thirty-eight (37%) were referred to our hospital after previous failed attempts to remove the airway FB at other hospitals. Of these 38 patients, three patients referred to our hospital after failure of rigid bronchoscopy and underwent rigid bronchoscopy without flexible bronchoscopy in our hospital due to impacted airway FB. The median duration between aspiration and bronchoscopic removal of the airway FB at our hospital was 21 (IQR, 3–129) days. Chest radiographs were normal for 26 (25%) patients, while 31 (30%) patients had a radio-opaque FB. The majority of patients (62/77, 81%) had a visible airway FB on chest computed tomography (CT).
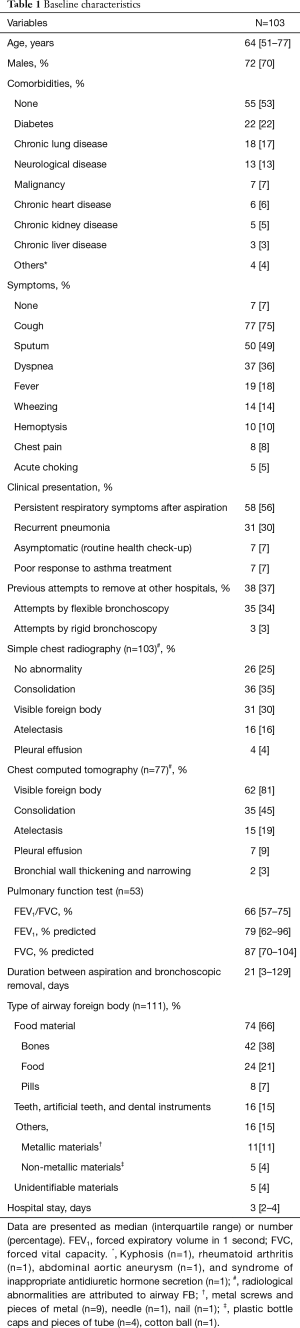
Full table
Bronchoscopy findings
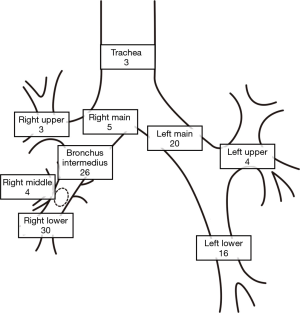
Locations of airway FBs are shown in Figure 1. Among the 103 total patients, there were 111 airway FBs (seven patients had two airway FBs and one patient had three airway FBs). Airway FBs were more commonly located in the right bronchi (61%). The most common types of airway FB were food material (66%) and teeth including dental prostheses and instruments (15%) (Table 1).
Removal technique and clinical outcomes
The clinical course of patients with FB aspiration is shown in Figure 2. Eleven of the fifty-four patients (20%) who underwent flexible bronchoscopy had a failed first attempt. If we exclude 12 patients referred from other hospital, failure rate of flexible bronchoscopy in our institution is 4.8% (2/42). Ten patients were converted to rigid bronchoscopy and one patient underwent a second attempt with flexible bronchoscopy under mechanical ventilation. The success rate of flexible bronchoscopy was 43 out of 54 cases (80%).
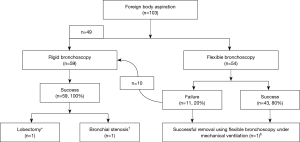
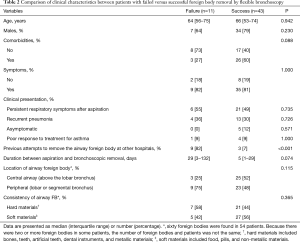
We compared clinical characteristics between patients with failed and successful FB removal by flexible bronchoscopy (Table 2). Previous attempt failure at another hospital was significantly more common among patients with a flexible bronchoscopy failure than in those with success [9/11 (82%) vs. 3/43 (7%), P<0.001]. In addition, patients with flexible bronchoscopy failure tended to have a longer duration between aspiration and bronchoscopic removal (median 29 vs. 5 days, P=0.074) and a more peripheral airway FB [9/12 (75%) vs. 23/48 (48%), P=0.115] than those with flexible bronchoscopy success; however, these differences were not statistically significant.
Full table
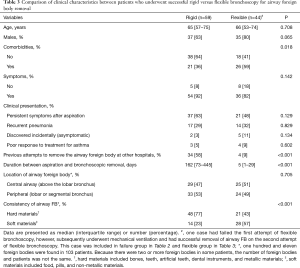
A total of 59 patients, including 10 patients who were converted from flexible to rigid bronchoscopy and 49 patients who underwent rigid bronchoscopy as the first attempt, underwent rigid bronchoscopy under general anesthesia. The success rate was 100%. Comparison of clinical characteristics according to successful procedure modalities (rigid vs. flexible bronchoscopy) to remove the airway FB are shown in Table 3. Rigid bronchoscopy was preferred to flexible bronchoscopy in patients with no comorbidities [38/59 (64%) vs. 18/44 (41%), P=0.018], a previous attempt to remove the airway FB at another hospital [34/59 (58%) vs. 4/44 (9%), P<0.001], longer duration between aspiration and bronchoscopy removal (median 162 vs. 5 days, P<0.001), and airway FB of hard consistency [48/62 (77%) vs. 21/49 (43%), P<0.001].
Full table
There were no acute procedure related complications. However, delayed complications occurred in two cases. A 26-year-old female who had no past medical history visited the hospital for four months of persistent cough and sputum production. After a failed attempt at FB (bean) removal from the left lower lobar bronchus using flexible bronchoscopy, she was referred to our hospital and had successful FB removal with rigid bronchoscopy. Three years later, the patient developed a broncho-esophageal fistula with recurrent pneumonia necessitating lobectomy. A 78-year-old male with chronic kidney disease was referred to our hospital for two weeks of fever. A FB (chicken bone) in the left lower lobar bronchus causing fibrosis and airway obstruction was removed with rigid bronchoscopy. Although he was asymptomatic six weeks later, he developed obstruction of the left lower lobar bronchus and required airway stenting.
Discussion
In our study, airway FB occurred more commonly in adult males and the FB was more frequently located in the right bronchus. Cough was the most common symptom and 30% of FBs were radiopaque on simple chest radiographs. These findings are consistent with published studies (1,11,14). About half of patients presented with chronic symptoms (recurrent pneumonia or poor response to asthma treatment) or no symptoms rather than with acute choking. In our study, acute choking events occurred in only 5%, which is in the lower range of 7–23% reported in previous studies on adult airway FBs (1,14). These low rates contrast with those of pediatric studies, which reported acute choking episodes in 46% of cases (15). This difference between pediatric and adult patients might be related to airway size and airway FB location. FBs may be more likely to be centrally located in children due to their smaller airways, while FBs in adults, who have larger airways, tend to be peripherally located. The other possible explanation is selection bias where patients with acute symptoms were treated at primary care clinics while those with less severe presenting symptoms and longer duration to FB removal developed complications and tended to present to tertiary centers.
About half of our patients (54/103, 52%) underwent flexible bronchoscopy as first line for FB removal. Our flexible bronchoscopy success rate of 80% is within the range of 61–100% reported by a recent large systematic review (11). In addition, we evaluated the differences between failed and successful flexible bronchoscopy cases. The only factor significantly associated with failure was a previous attempt to remove the airway FB at another hospital. We found trends toward association between longer duration from aspiration to removal attempt and peripherally located FB and flexible bronchoscopy removal failure, although these relationships were not statistically significant. Delayed diagnosis of FB aspiration and peripherally located FB frequently result in granulation tissue formation and FB impaction, which makes removal by flexible bronchoscopy more difficult (1,11,16).
In the present study, a total of 59 patients underwent rigid bronchoscopy, and 100% were successful. None of our patients required surgery to remove their airway FB. Of the 103 total patients, 49 (47%) were managed with rigid bronchoscopy as the first line. The proportion of adult patients managed directly with rigid bronchoscopy in practice can vary from 3% to 40% depending on practice setting and availability of rigid bronchoscopy (11,17).
Numerous publications have reported on the use of flexible or rigid bronchoscopy for airway FB removal. A recent systematic review yielded 107 articles on bronchoscopic airway FB removal (11). However, there are no studies on factors to consider when deciding between flexible and rigid bronchoscopy to maximize cost-effectiveness and minimize failure rate. It is not feasible for rigid bronchoscopy to be available in all hospitals; therefore, it would be valuable to have methods for identifying patients with airway FBs who should be referred to a tertiary hospital with rigid bronchoscopy capabilities. In our study, patients with successful airway FB removal by flexible bronchoscopy had fewer previous attempts to remove the airway FB at other hospitals (9% vs. 58%, P<0.001), shorter duration between aspiration and FB removal (median 5 vs. 162 days, P<0.001), and FB of soft consistency (57% vs. 23%, P<0.001) than those in whom rigid bronchoscopy was used. Therefore, we infer that rigid bronchoscopy could be considered in the patients with a previous failed attempt, longer duration from FB aspiration, and FB of hard consistency. Factors leading to use of rigid bronchoscopy as the first-line modality are often cited to be FB size, nature and chronicity (11,17). In addition to airway instability, rigid bronchoscopy tends to be the preferred first-line modality when FB are large, sharp and embedded in granulation tissue. Our practice is similar to those of tertiary referral centers with an established rigid bronchoscopy practice (6,17,18). However, unlike the retrospective study by Hsu (17), we did not include stent removal as the source of iatrogenic airway FBs in our analysis.
Our study has several limitations. First, our study was retrospective and observational in design therefore the factors we found to be associated with successful rigid bronchoscopy may not be causal. We are unable to account for confounding factors such as size, shape, and nature of margin of airway FB, which could potentially be associated with outcomes. Our findings should be confirmed by larger and higher quality studies. Second, our center is a tertiary referral center, which likely led to some selection bias. In addition, our conclusions cannot be easily applied to other centers where rigid bronchoscopy may not be readily available. In particular, significant bias could potentially have been introduced through clinical selection of patients for rigid bronchoscopy as the first attempt. In our institute, rigid bronchoscopy was considered as the first-line modality for airway FB removal in patients who had a need for airway protection or impacted FB identified on chest imaging. Although these situations are generally considered as the indications for the rigid bronchoscopy (12,13), there could be a selection bias that might have influenced the significance of our results.
Conclusions
In conclusion, we found that previous attempts to remove airway FBs at other hospitals, delayed diagnosis of FB aspiration, and peripherally located FB could be associated with failure of flexible bronchoscopy for airway FB removal. In contrast, rigid bronchoscopy could be used to successfully remove airway FBs even in patients with previous failed attempts, delayed diagnosis of FB aspiration, and FB of hard consistency. Although these findings should be confirmed by further studies, these associations may serve as a basis for further work to identify factors that can assist us in selecting patients for expedited rigid bronchoscopy in order to avoid multiple interventional attempts and for selecting patients most appropriate for flexible bronchoscopy to minimize the cost of excessive utilization of rigid bronchoscopy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of Samsung Medical Center (IRB No. 2017-08-033). Informed consent was waived because of the retrospective nature of the study.
References
- Dong YC, Zhou GW, Bai C, et al. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern Med 2012;51:2515-9. [Crossref] [PubMed]
- Debeljak A, Sorli J, Music E, et al. Bronchoscopic removal of foreign bodies in adults: experience with 62 patients from 1974-1998. Eur Respir J 1999;14:792-5. [Crossref] [PubMed]
- Nguyen LH, Nguyen DH, Tran TN, et al. Endobronchial foreign bodies in Vietnamese adults are related to eating habits. Respirology 2010;15:491-4. [Crossref] [PubMed]
- Mise K, Jurcev Savicevic A, Pavlov N, et al. Removal of tracheobronchial foreign bodies in adults using flexible bronchoscopy: experience 1995-2006. Surg Endosc 2009;23:1360-4. [Crossref] [PubMed]
- Ling Hsu AA, Pena Takano AM, Wai Chan AK. Beyond removal of endobronchial foreign body. Am J Respir Crit Care Med 2014;189:996-7. [Crossref] [PubMed]
- Casalini AG, Majori M, Anghinolfi M, et al. Foreign body aspiration in adults and in children: advantages and consequences of a dedicated protocol in our 30-year experience. J Bronchology Interv Pulmonol 2013;20:313-21. [Crossref] [PubMed]
- Ayed AK, Jafar AM, Owayed A. Foreign body aspiration in children: diagnosis and treatment. Pediatr Surg Int 2003;19:485-8. [Crossref] [PubMed]
- Zhang X, Li WX, Cai YR. A time series observation of Chinese children undergoing rigid bronchoscopy for an inhaled foreign body: 3,149 cases in 1991-2010. Chin Med J (Engl) 2015;128:504-9. [Crossref] [PubMed]
- Yadav SP, Singh J, Aggarwal N, et al. Airway foreign bodies in children: experience of 132 cases. Singapore Med J 2007;48:850-3. [PubMed]
- Blanco Ramos M, Botana-Rial M, Garcia-Fontan E, et al. Update in the extraction of airway foreign bodies in adults. J Thorac Dis 2016;8:3452-6. [Crossref] [PubMed]
- Sehgal IS, Dhooria S, Ram B, et al. Foreign Body Inhalation in the Adult Population: Experience of 25,998 Bronchoscopies and Systematic Review of the Literature. Respir Care 2015;60:1438-48. [Crossref] [PubMed]
- Mehta AC, Dasgupta A. Bronchoscopic approach to tracheobronchial foreign bodies in adults pro-flexible bronchoscopy. J Bronchology Interv Pulmonol 1997;4:173-8.
- Díaz-Jiménez JP. Bronchoscopic approach to tracheobronchial foreign bodies in adults pro-rigid bronchoscopy. J Bronchology Interv Pulmonol 1997;4:159-72.
- Chen CH, Lai CL, Tsai TT, et al. Foreign body aspiration into the lower airway in Chinese adults. Chest 1997;112:129-33. [Crossref] [PubMed]
- Foltran F, Ballali S, Passali FM, et al. Foreign bodies in the airways: a meta-analysis of published papers. Int J Pediatr Otorhinolaryngol 2012;76 Suppl 1:S12-9. [Crossref] [PubMed]
- Kogure Y, Oki M, Saka H. Endobronchial foreign body removed by rigid bronchoscopy after 39 years. Interact Cardiovasc Thorac Surg 2010;11:866-8. [Crossref] [PubMed]
- Hsu AA. Endoscopic intervention of lower airway foreign matter in adults-a different perspective. J Thorac Dis 2015;7:1870-7. [PubMed]
- Cravo J, Marques MAT. Endobronchial foreign bodies in adults - Flexible bronchoscopy as a first approach. Pulmonology 2018;24:198-9. [Crossref] [PubMed]


