
Optimizing intraoperative ventilation during one-lung ventilation—is individualization the road to success?
Avoiding ventilator associated lung injury in surgical patients requiring general anesthesia is a primary focus of anesthetic research—mechanical ventilation should not induce further harm. With the knowledge gained from important clinical and experimental research on the acute respiratory distress syndrome, the principles of lung protective ventilation (LPV) have been transferred to the operating theatre with the aim of reducing postoperative pulmonary complications in patients with healthy lungs.
Patients with pulmonary neoplasia are at high-risk for developing postoperative pulmonary complications after lung resection surgery. Injury to the isolated lung results from lung collapse and direct surgical trauma. The isolation of one lung during one-lung ventilation (OLV) is accompanied by significant changes in pulmonary mechanics and pulmonary perfusion due to hypoxic pulmonary vasoconstriction. The main targets of mechanical ventilation during OLV are therefore preserving oxygenation and preventing injury of the ventilated lung. However, the optimal LPV settings during OLV are largely unknown. Furthermore, there is a lack of evidence regarding the question whether or not the known principles of LPV also apply to patients requiring OLV and if LPV has the potential to reduce the incidence of postoperative pulmonary complications in patients requiring lung resection surgery due to malignant neoplasia.
In a recently published prospective multicenter trial, Marret and colleagues (1) examined the impact of an LPV strategy on postoperative outcome in 346 patients undergoing lobectomy or pneumonectomy for lung cancer. Patients were randomized to receive either an intraoperative LPV [defined as a tidal volume of 5–8 mL/kg ideal body weight (IBM)] or a nonprotective ventilation strategy with tidal volumes of 10 mL/kg ideal body weight without positive end-expiratory pressure (PEEP). Tidal volumes were not changed throughout anesthesia, but were adjusted if the plateau pressure exceeded 30 cmH2O.
The main finding of the study was that major postoperative complications or death occurred in 13.4% in the LPV group vs. 22.2% in the nonprotective ventilation group. Moreover, the rate of other pulmonary complications not included in the primary end point (bronchial stasis, atelectasis, hypercapnia, bronchial fistula) was also significantly reduced in the LPV group. Additionally, the reduction in postoperative pulmonary complications resulted in a significantly shorter median hospital stay (11 days in the LPV group vs. 12 days in the nonprotective group, respectively, P=0.048), while the time of ICU-stay did not differ between both groups.
This publication adds valuable information to our knowledge concerning optimal intraoperative mechanical ventilation of our patients. It provides evidence that the use of lower tidal volumes and PEEP not only improves intraoperative pulmonary physiology, but is also associated with a lower rate of postoperative complications in patients requiring OLV for lung resection surgery. However, the study from Marret and colleagues has some important limitations that have to be kept in mind when interpreting the findings.
First, there is no statement how OLV was performed in the study population, i.e., if double lumen tubes or bronchial blockers were used in equal proportions in both groups. Bronchial blockers lack the possibility of evacuation of the secretions in the dependent lung and might therefore be associated with a higher rate of postoperative bronchial stasis and pneumonia, which were the main complications observed in the study (1). Furthermore, there was no standardized protocol for recruitment maneuvers after conclusion of OLV. It was left at the discretion of the surgeons and anesthetists to determine how the reinflation of the isolated lung was performed, which could however have substantial effects on postoperative outcome.
Second, no information is given regarding the mean duration of OLV in proportion to the total time of mechanical ventilation. Additionally, the authors state that the tidal volumes were not adjusted after the initiation of OLV. The total lung volume is dependent on the patient’s size and gender but independent of total body weight. Lung protective tidal volumes of 5–8 mL/kg IBW however refer to the calculated total lung volume. If approximately half of the total lung volume is not ventilated—which is the case during OLV—the given tidal volume is applied to one lung only and may result in inadequately high tidal volumes during OLV, which may cause potentially injurious mechanical stress and strain to the residual ventilated lung. In the study from Marret et al., the “effective” tidal volume during OLV can be calculated to be about 10–16 mL/kg IBW in the LPV group and up to 20 mL/kg IBW in the nonprotective ventilation group. Therefore, even in the LPV group, the applied tidal volume was considerably outside the range of an LPV strategy. In a prospective cohort study from Amar et al. (2), which failed to show a significant association of an LPV during OLV, missing adaption of tidal volumes after the initiation of OLV was also the main point of criticism.
Indirect evidence for the application of inadequately high tidal volumes during OLV in the study of Marret et al. is found when the driving pressures are analyzed: driving pressures were 22.7±5.6 cmH2O in the control group and 14.1±4.7 (mean ± SD) in the LPV group. Two large studies, one retrospective analysis (3) and one prospective observational study (4), demonstrated higher mortality for patients with acute respiratory distress syndrome if driving pressures exceeded 14–15 cmH2O. Therefore, in the study of Marret et al., even in the LPV group, a significant proportion of patients were not ventilated according to the principles of LPV (1). In a recent meta-analysis of patients with normal lungs during anesthesia, intraoperative driving pressures were also significantly associated with the development of postoperative pulmonary complications (5).
Unfortunately, the effects of PEEP and tidal volumes were not analyzed separately in the study by Marret et al. The observed postoperative complications may therefore also be attributed to the development of intraoperative atelectasis caused by the absence of PEEP in the control group, which would question the concept of “permissive atelectasis” (6) in thoracic surgery patients requiring OLV. However, in the PROVHILO-trial (7), the application of higher PEEP levels in general failed to reduce postoperative complications if low tidal volumes of 8 mL/kg IBW were consequently applied during open abdominal surgery. Conversely, nonprotective ventilation was associated with higher postoperative pulmonary complications in the IMPROVE-trial (8), where a TV of 10–12 mL IBW with no PEEP was compared to a TV of 6–8 mL with a PEEP of 6–8 cmH2O and repetitive recruitment maneuvers in abdominal surgery.
Taken together, there is growing evidence that the lung strain induced by the use of high tidal volumes above 10 mL/kg IBW in combination with high driving pressures is highly injurious even if it is applied for only a relatively short period of time in the operating theatre. If low tidal volumes are applied, PEEP may play a secondary role in healthy lungs but may help to improve pulmonary compliance with the aim at keeping driving pressures low when mechanical ventilation is necessary in patients with preexisting pulmonary disease. Furthermore, the PEEP levels applied in the clinical trials mentioned above were relatively low and the PEEP levels used might be too low to exert a significant effect on postoperative outcomes, even in patients of normal weight.
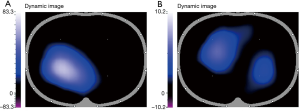
Pereira and colleagues (9) found that individualized PEEP settings using electrical impedance tomography (EIT) were able to significantly reduce intraoperative driving pressures and postoperative atelectasis in open as well as in laparoscopic abdominal surgery. Individual PEEP levels varied markedly across individuals with a median PEEP of 12 cmH2O. PEEP may therefore have no beneficial effects if it is not adapted to the patient’s individual pulmonary mechanics. EIT based PEEP titration might further improve our understanding of LPV in the future.
In a recently published trial in morbidly obese patients undergoing bariatric surgery, individualized PEEP titrated using EIT significantly improved intraoperative oxygenation and end-expiratory lung volume compared to standard ventilation with low PEEP levels but the observed differences vanished after extubation (10).
In conclusion, we suggest that lung protective perioperative management should not only include individualization of mechanical ventilation during surgery but should be extended to measures such as application of continuous airway pressure in the post-anesthesia care unit in high-risk patients.
Perspectively, newer anesthetic concepts in video-assisted thoracoscopic surgery include even the avoidance of endotracheal intubation and performing lung resection surgery with spontaneous breathing laryngeal mask anaesthesia (11) (see Figure 1), or even “tubeless” pulmonary resections (12) harboring the potential for further reducing pulmonary complications and providing faster postoperative recovery in non-small-cell lung cancer thoracic surgery (13).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Marret E, Cinotti R, Berard L, et al. Protective ventilation during anaesthesia reduces major postoperative complications after lung cancer surgery: A double-blind randomised controlled trial. Eur J Anaesthesiol 2018;35:727-35. [Crossref] [PubMed]
- Amar D, Zhang H, Pedoto A, et al. Protective Lung Ventilation and Morbidity After Pulmonary Resection: A Propensity Score-Matched Analysis. Anesth Analg 2017;125:190-9. [Crossref] [PubMed]
- Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372:747-55. [Crossref] [PubMed]
- Laffey JG, Bellani G, Pham T, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med 2016;42:1865-76. [Crossref] [PubMed]
- Neto AS, Hemmes SN, Barbas CS, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 2016;4:272-80. [Crossref] [PubMed]
- Hemmes S, Serpa Neto A, Gama de Abreu M, et al. Intraoperative ventilation: improving physiology, or preventing harm? Br J Anaesth 2016;116:438-9. [Crossref] [PubMed]
- PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology. Hemmes SN, Gama de Abreu M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet 2014;384:495-503. [Crossref] [PubMed]
- Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013;369:428-37. [Crossref] [PubMed]
- Pereira SM, Tucci MR, Morais CCA, et al. Individual Positive End-expiratory Pressure Settings Optimize Intraoperative Mechanical Ventilation and Reduce Postoperative Atelectasis. Anesthesiology 2018;129:1070-81. [Crossref] [PubMed]
- Nestler C, Simon P, Petroff D, et al. Individualized positive end-expiratory pressure in obese patients during general anaesthesia: a randomized controlled clinical trial using electrical impedance tomography. Br J Anaesth 2017;119:1194-205. [Crossref] [PubMed]
- Ambrogi MC, Fanucchi O, Gemignani R, et al. Video-assisted thoracoscopic surgery with spontaneous breathing laryngeal mask anesthesia: preliminary experience. J Thorac Cardiovasc Surg 2012;144:514-5. [Crossref] [PubMed]
- Lirio F, Galvez C, Bolufer S, et al. Tubeless major pulmonary resections. J Thorac Dis 2018;10:S2664-70. [Crossref] [PubMed]
- Liu J, Cui F, Pompeo E, et al. The impact of non-intubated versus intubated anaesthesia on early outcomes of video-assisted thoracoscopic anatomical resection in non-small-cell lung cancer: a propensity score matching analysis. Eur J Cardiothorac Surg 2016;50:920-5. [Crossref] [PubMed]


