
“No option” patients for coronary revascularization: the only thing that is constant is change
Refractory angina pectoris (RAP) associated with myocardial ischemia is a common medical condition, a major cause of patient morbidity and a growing public health burden that affects millions of patients worldwide (1-4). Importantly, despite recent advancements in patient care, there is lack of convincing evidence regarding reduction in both ischemia burden and mortality in this challenging patient population (4). Moreover, a significant proportion of these patients have no revascularization options despite improved interventional procedures and techniques. Patients with RAP are also more frequently hospitalized than controls, often undergoing multiple medical procedures, increasing the economic burden to the healthcare system (5).
Any discussion of the care and prognosis of patients with RAP is not a straightforward one. Nonetheless, the definition of RAP depends on both the objective and subjective assessment of the patient by the caregiver, and depends on the success of the therapeutic procedure and on the adherence rate to optimal medical management in each medical set-up and/or healthcare system. According to the 2013 European Society of Cardiology Guidelines on the management of stable coronary artery disease (CAD) patients, RAP is defined as “a chronic condition caused by clinically established reversible myocardial ischemia in the presence of CAD, which cannot be adequately controlled by a combination of medical therapy, coronary angioplasty or coronary artery bypass graft”. However, as was shown in previous studies (6,7), a patient who initially cannot be adequately controlled by medical and invasive means may eventually receive revascularization later on during the course of ischemic heart disease.
The article by Sharma et al. (8), describes results based on the options in myocardial syndrome therapy (OPTIMIST) program, which describes the experience of a dedicated RAP clinic, recruiting patients from 1996 to 2001 at Hennepin County Medical Center (Minneapolis, MN, USA) and from 2002 to 2014 at the Minneapolis Heart Institute at Abbott Northwestern Hospital (Minneapolis, MN, USA). Of the 1,363 patients in this registry, 342 (25.1%) had eventually undergone revascularization, after a median interval of 2.2 years from initial “RAP” designation, the majority of which were percutaneous coronary interventions (PCI). These patients were then followed up for a median of 5.1 years. Seventy-one of these patients (20.8%) died after a median interval of 4.4 years from baseline. This group, however, had significantly lower mortality rates than patients who were not revascularized (2.0% per year versus 4.4% per year, P<0.001). When assessed by method of revascularization, lesion location and lesion type, PCI for a pre-existing lesion had resulted in higher five-year mortality compared with coronary artery bypass graft surgery (CABG), PCI for new lesions or for restenosis. The study is lacking a systematic quantitative assessment of myocardial ischemic and cardiac function in order to stratify the risk profile and allow for better prognostication of the aforementioned cohort of patients.
Throughout the years, these “no-option” patients were subject to numerous attempts for both pharmacological and non-pharmacological therapies. Some of the non-pharmacological treatments include enhanced external counter-pulsation (EECP) treatment and neurostimulatory techniques, which demonstrated efficacy in ameliorating symptoms and improving quality of life, although convincing evidence regarding reduction in both ischemia burden and mortality is still lacking (9-11). Conversely, transmyocardial or direct myocardial revascularization (TMR/DMR) techniques have been abandoned because they were largely considered ineffective based on a pivotal blinded randomized trial (12). Cell therapy is another field of interest, showing promise of improving outcomes for these patients. However, there are multiple unresolved scientific questions concerning this field of investigation, such as the type of multipotent cells, the therapeutic potency, the risk benefit characteristics and/or appropriate mode of delivery to the myocardium. Recently, the novel coronary sinus reducer, a catheter-mounted hourglass-shaped self-expandable stent that is implanted in the coronary sinus to divert the coronary flow has been shown to improve symptoms and quality of life in patients with RAP (13). However, this treatment has not been validated yet in a blinded randomized trial and also, it was not compared with revascularization therapy, as procedures were performed based on the assumption that the definition of RAP is a permanent one, and that there is no longer an option for PCI or CABG. Thus, more research is needed, geared towards RAP patients in order to improve their symptoms and prognosis.
The current findings suggest that a significant portion of the patients who initially are designated as RAP will eventually undergo successful revascularization, and that those who do may benefit from the procedure, especially when treated at a dedicated clinic for RAP. Importantly, the options for revascularization are continuously evolving as well, showing greater benefit and improved safety over the years. In addition, many of the patients who are designated as “no-option” are survivors of suboptimal PCI, which might translate into worse prognosis (14,15). In the experience of Jax et al. (6), two noteworthy factors that were coupled with success included the allocation of a longer time period and two senior operators to the procedure. These local factors are modifiable, and may reach higher rates of success in patients considered at first evaluation to have RAP. Thus, the obvious conclusion is that the initial assessment of a “no-option” patient might be mistaken, and thus should probably be replaced by a more appropriate “perhaps later-option” or “alternative option” ones. We therefore must consider the definition of RAP as a state of the affairs at a specific point in time, and realize it is a temporary one, in many cases. As is often the scenario, the appropriate management algorithm should include a periodical assessment of the patients, thus eventually allocating a patient from the RAP state to a possible revascularization and/or other therapy, improving or even potentially curing angina.
As the great Greek philosopher Heraclitus once said, so is the case with RAP patients “the only thing that is constant is change” and we may need to adapt to the fact that “no-option” angina status may change over time (Table 1). It is therefore not only the definition of angina that may change, but our own perceptions of this challenging cohort of patients.
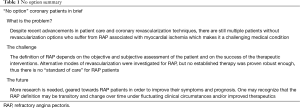
Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2008;117:e25-146. [PubMed]
- Yang EH, Barsness GW, Gersh BJ, et al. Current and future treatment strategies for refractory angina. Mayo Clin Proc 2004;79:1284-92. [Crossref] [PubMed]
- Cheng K, de Silva R. New Advances in the Management of Refractory Angina Pectoris. Eur Cardiol 2018;13:70-9. [Crossref] [PubMed]
- Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949-3003. [Crossref] [PubMed]
- Povsic TJ, Broderick S, Anstrom KJ, et al. Predictors of long-term clinical endpoints in patients with refractory angina. J Am Heart Assoc 2015.4. [PubMed]
- Jax TW, Peters AJ, Khattab AA, et al. Percutaneous coronary revascularization in patients with formerly “refractory angina pectoris in end-stage coronary artery disease” - not “end-stage” after all. BMC Cardiovasc Disord 2009;9:42. [Crossref] [PubMed]
- Barsness G, Tesmer L, Lennon RJ. Treatment of patients previously deemed “unrevascularizable” often includes revascularization J Am Coll Cardiol 2008;51:B60. [abstract].
- Sharma R, Tradewell M, Kohl LP, et al. Revascularization in “no option” patients with refractory angina: Frequency, etiology and outcomes. Catheter Cardiovasc Interv 2018;92:1215-9. [Crossref] [PubMed]
- Zhang C, Liu X, Wang X, et al. Efficacy of Enhanced External Counterpulsation in Patients With Chronic Refractory Angina on Canadian Cardiovascular Society (CCS) Angina Class: An Updated Meta-Analysis. Medicine (Baltimore) 2015;94:e2002. [Crossref] [PubMed]
- Shah SA, Shapiro RJ, Mehta R, et al. Impact of enhanced external counterpulsation on Canadian Cardiovascular Society angina class in patients with chronic stable angina: a meta-analysis. Pharmacotherapy 2010;30:639-45. [Crossref] [PubMed]
- Andréll P, Yu W, Gersbach P, et al. Long-term effects of spinal cord stimulation on angina symptoms and quality of life in patients with refractory angina pectoris--results from the European Angina Registry Link Study (EARL). Heart 2010;96:1132-6. [Crossref] [PubMed]
- Leon MB, Kornowski R, Downey WE, et al. A blinded, randomized, placebo-controlled trial of percutaneous laser myocardial revascularization to improve angina symptoms in patients with severe coronary disease. J Am Coll Cardiol 2005;46:1812-9. [Crossref] [PubMed]
- Verheye S, Jolicœur EM, Behan MW, et al. Efficacy of a device to narrow the coronary sinus in refractory angina. N Engl J Med 2015;372:519-27. [Crossref] [PubMed]
- Williams B, Menon M, Satran D, et al. Patients with coronary artery disease not amenable to traditional revascularization: prevalence and 3-year mortality. Catheter Cardiovasc Interv 2010;75:886-91. [PubMed]
- Kornowski R. Refractory myocardial angina and determinants of prognosis. Catheter Cardiovasc Interv 2010;75:892-4. [PubMed]


