
A comparison of fractional flow reserve determination and coronary angiography results in patients with unstable angina and analysis of related factors
Introduction
Unstable angina (UA) is an acute coronary ischemic syndrome between stable angina and acute myocardial infarction (AMI) and is one of the common diseases in clinical emergencies (1). Its clinical instability mainly depends on the instability of the local lesion itself in coronary artery. Effective treatment of UA can increase the survival rate and improve quality of life. One of the most important therapeutic goals is to achieve the immediate relief of AMI. For patients with non-ST-segment elevation acute coronary syndromes (NSTEACS), the goal of revascularization is to treat recurrent myocardial ischemia and thus prevent the progression to myocardial infarction or sudden death (2). Coronary angiography (CAG), as one of the most important means of examination, is used to identify the lesions and guide the treatment. Based on the extent and characteristics of lesions identified by CAG, a decision of revascularization (or not) can be made (1). However, more studies have demonstrated that intervention in nonfunctional stenosis does not benefit patients (3-5). CAG can only evaluate the stenosis degree of coronary artery lesions and cannot accurately determine whether the stenosis caused myocardial ischemia (6). In recent years, more attention has been paid to the determination of myocardial fractional flow reserve (FFR), which can better determine whether coronary artery stenosis causes myocardial ischemia and objectively evaluate whether PCI is required for the coronary artery lesions (7).
In our current study, we explored the investigate the differences and relationship between FFR determination and CAG in patients with UA, and investigated factors affecting FFR value in UA patients.
Methods
Subjects
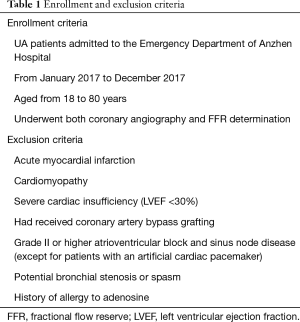
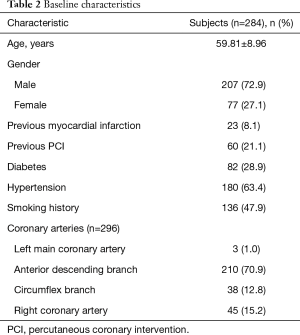
A total of 284 UA patients (296 coronary lesions) who were admitted to the emergency department of Anzhen Hospital Affiliated to Capital Medical University from January 2017 to December 2017 were enrolled in this study. All these patients underwent both CAG and FFR determination. These subjects include 207 males and 77 females, aged from 36 to 80 years, with the average age of 59.81±8.96 years. The diagnosis of UA was based on the Guidelines for the Diagnosis and Treatment of Unstable Angina Pectoris and Non-ST-segment Elevation Myocardial Infarction (1) released by the Chinese Society of Cardiology in 2007. The exclusion criteria were listed in Table 1. All the subjects signed the informed consent forms of percutaneous coronary intervention (PCI) and special lesions before surgery. This study was approved by Anzhen Hospital Ethics Committee (ethic approval number: 201756X) and all patients have signed informed consent forms.
Full table
Main methods
Judging the disease condition by using CAG
CAG examination was performed according to standard Judkins method through femoral artery or radial artery. Coronary artery stenosis was judged by visual assessment by using the following formula: diameter of the normal vessel in the proximal part of stenotic vessel—diameter of stenotic site)/diameter of the proximal part of stenotic vessel ×100%.
FFR determination
FFR measurements were carried out with RADI Analyzer® Xpress monitor (St. Jude Medical) and pressure guidewire. Zero calibration was carried out three times (i.e., zero calibration of catheter chamber pressure channel, aortic pressure, and pressure guidewire) in vitro before measurements, followed by balancing aortic pressure and pressure guidewire pressure to ensure that both pressures in the body were at the same baseline level. Then, the pressure guidewire was delivered to the distal part of the lesion to be measured as far as possible, and 200–300 µg of nitroglycerin was injected into the coronary artery to avoid the impact of arterial spasm on the measurement results. Adenosine triphosphate (ATP) [140–180 µg/(kg·min)] was injected via the median cubital vein to achieve maximum hyperemia. The distal coronary artery pressure (Pd) and aortic pressure (Pa) were measured by pressure guidewire and coronary artery guiding catheter, respectively. FFR values were calculated according to the formula FFR = Pd/Pa.
Comparison between CAG and FFR determination
CAG and FFR determination were performed in all patients, and the roles of these two methods in guiding the treatment of UA were compared and analyzed. CAG: PCI was required if CAG revealed ≥50% stenosis of the left main coronary artery or ≥75% stenosis of other vessels or if FFR was ≤0.8. If angiography and FFR showed contradicting results, we take FFR as PCI indication.
Main measures
The clinical data of all enrolled patients and routine blood test items before and after admission including general data (sex and age), risk factors of coronary heart disease (history of hypertension, smGoking, diabetes, hyperlipidemia, previous myocardial infarction, and previous PCI), blood lipids [triglyceride (TG), total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL)], glycosylated hemoglobin, C-reactive protein (CRP), lesion site, degree of vascular stenosis, and FFR value were recorded. With the FFR value of 0.8 as the cutoff value, the patients were divided into two groups: FFR ≤0.8 group and FFR >0.8 group. The general data and laboratory findings were compared between these two groups, and the possible predictive factors were analyzed.
Statistical analysis
The statistical analysis was completed in SPSS 20.0 software. The continuous data are expressed as mean ± standard deviation, and inter-group differences were compared by using the t-test. The count data are expressed as proportions or percentages and compared using chi square test. The influential factors were analyzed by using Logistic regression analysis. A P value of <0.05 was considered statistically significant.
Results
Comparison between CAG and FFR determination
Of the 284 patients enrolled in the study, all received CAG and FFR determination. Detailed patient characteristics (age, sex, patient’s history, Coronary arteries) were listed in Table 2. Of 296 UA lesions, 160 (54.1%) had ≥75% stenosis and 136 (45.9%) had <75% stenosis; 168 (56.8%) had an FFR value ≤0.8 and 128 (43.2%) had an FFR value >0.8. There was no significant difference between these two examination methods (P=0.508, χ2=0.438). Further analysis showed that 43 (26.9%) of the 160 lesions with angiographic stenosis of ≥75% had an FFR value of >0.8 and did not require PCI; 49 (38.3%) of the 128 lesions with angiographic stenosis of 50–70% had an FFR value of ≤0.8 and needed PCI; 2 of 8 patients with <50% stenosis had an FFR value of ≤0.8 and needed PCI (Table 3). If FFR was used as the “gold standard” of PCI, the sensitivity, specificity, positive predictive value, and negative predictive value of CAG in guiding PCI for UA were 69.6%, 66.4%, 73.1%, and 62.5% respectively.
Full table
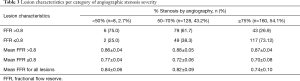
Full table
Comparison of CAG results and FFR for different diseased vessels
CAG showed 296 lesions had different degrees of stenosis [72.6±11.4% (30–99%)]. To compare the difference of FFR and CAG results, we further analyzed the data in different diseased vessels, as shown in Figure 1.
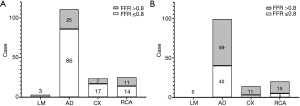
Three lesions (1.01%) were located in the left main coronary artery (LM), where angiography showed severe stenosis (all ≥50% stenosis) and FFR values were ≤0.8%. (Figure 1A). If FFR was used as the “gold standard” of PCI, the sensitivity of angiography was 100%. However, for 210 lesions in the anterior descending branch (AD, 70.95%), angiography and FFR readings were different sometimes. One hundred and eleven cases had ≥75% stenosis as indicated by angiography, among which 86 had an FFR value of ≤0.8 and 25 had an FFR value of >0.8 (Figure 1A). Meanwhile, 99 cases had moderate or mild stenosis (<75% stenosis), among which 40 had an FFR value of ≤0.8 and 59 had an FFR value of >0.8 (Figure 1B). The sensitivity of angiography was 68.25%.
Contradicting results of angiography and FFR were also found in cases of the circumflex branch (CX, n=38, 12.8%) and right coronary artery (RCA, n=45, 15.2%) lesions (Figure 1). The sensitivity of angiography was 85% and 73.68%, respectively.
These results indicated that stent placements based solely on angiography for lesions of anterior descending artery and right coronary artery might have a higher misjudgment rate.
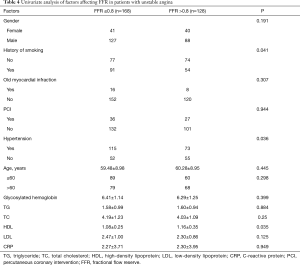
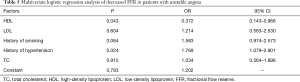
Univariate and multivariate analyses of factors affecting FFR in UA patients
To identify factors affecting FFR in UA patients, we performed univariate analysis. Of the variables considered, smoking history, history of hypertension, and HDL significantly differed between FFR ≤0.8 group and FFR >0.8 group, which indicated that these factors could be predictors of FFR <0.8 in UA patients (Table 4). Further multivariate analysis with Logistic regression demonstrated that history of hypertension is an independent risk factor for FFR in UA patients, and HDL is an independent protective factor (Table 5).
Full table
Full table
Discussion
UA has a unique pathophysiological mechanism and clinical prognosis; if not treated timely, it may develop into AMI or sudden death. Standard intensive therapy for UA includes anti-ischemic therapy, anti-platelet therapy, and anticoagulant therapy; if intensive conservative therapy fails, early interventional therapy is needed to determine the necessity of revascularization. The goal of revascularization in UA patients is to treat recurrent myocardial ischemia and thus prevent progression to myocardial infarction or sudden death (2). The FRISC-II randomized controlled trial (8) enrolled 2,457 high-risk UA patients and divided them into early interventional therapy group (PCI performed within 4 days and CABG within 8 days) and conservative treatment group (PCI only for severe angina). Within 12 months, 78% of the patients in the early interventional therapy group and 43% of the patients in the conservative treatment group underwent revascularization. One year after follow-up, the overall mortality rate significantly declined in the early interventional therapy group (2.2% vs. 3.9%, RR =0.57, 95% CI: 0.36–0.90), along with the significantly decreased incidence of myocardial infarction (8.6% vs. 11.6%, RR =0.74, 95% CI: 0.59–0.94). In addition, the combined incidence of death and MI significantly decreased (10.4% vs. 14.1%, RR =0.74, 95% CI: 0.60–0.92).
CAG remains one of the most important means to assess whether further revascularization is needed. CAG, which can provide the most intuitive morphological data of coronary artery, is still the “gold standard” for the diagnosis of coronary heart disease. However, due to its technical characteristics, CAG has the following shortcomings: (I) the interpretation of angiographic findings is somehow subjective, and the degree of stenosis of coronary artery lesions may be overestimated or underestimated; and (II) CAG can neither further assess the physiological significance of coronary artery stenosis nor determine whether stenosis causes functional ischemia. Unfortunately, both the morphologies and physiological data of the coronary artery are needed to help doctors establish tailored treatment strategies (9).
Myocardial FFR, which can better determine whether coronary artery stenosis causes myocardial ischemia, has gradually become a widely recognized indicator for the invasive evaluation of lesion functions. Treatment strategies guided by FFR have been proven to be safe and economical and can improve the prognosis of patients (4). The guidelines in the United States (IIa, A), the European Society of Cardiology (I, A) and China (IIa, A) recommend the use of FFR for assessing the presence of functional ischemia in borderline lesions and guiding revascularization (7,10,11). In the 2009 FAME study (12,13), 1,005 patients with multivessel coronary artery disease (at least two vessels with >50% lesion) undergoing stenting from 20 centers in Europe and the United States were randomly divided into PCI group and FFR group. FFR determination was performed after CAG for patients in FFR group. Interventional therapy was performed only in patients with FFR ≤0.8, and drug therapy was applied in patients with FFR >0.8. It was found that the number of stents used was 2.7±1.2 in PCI group and 1.9±1.3 in FFR group (P<0.05); the post-operative 1-year all-cause mortality was 3.0% vs. 1.8% (P=0.19); the incidence of MI was 8.7% vs. 5.7% (P=0.07); the rate of revascularization was 9.5% vs. 6.5% (P=0.08); and the 1-year incidence of MI or death was 11.1% vs. 7.3% (P=0.04). The benefit from FFR was estimated to be equivalent to the prevention of 1 major adverse cardiovascular event (MACE) every 20 FFR measurements.
According to the Chinese Expert Consensus on Clinical Application of Fractional Flow Reserve (2016 edition) (14), for patients with acute coronary syndrome, FFR determination for non-culprit lesions should be performed following CAG, so as to guide treatment decision-making, especially the application of PCI. Of important, unnecessary stent implantation may lead to stent-related immediate, short-term, and/or long-term adverse events such as no-reflow, coronary artery dissection, perioperative myocardial infarction, in-stent thrombosis, and in-stent restenosis. These adverse events can lead to serious cardiac dysfunction and sudden death. Therefore, in order to further achieve individualized and accurate treatment and make each UA patient can truly benefit from stenting, the PCI strategy should be established after the physiological images of coronary artery stenosis/lesions are obtained and reviewed. As shown in our study, there were some inconsistencies between the CAG and FFR results. Among the coronary lesions with <50%, 50–70%, and ≥75% stenosis, the proportions of lesions with FFR ≤0.8 were 25%, 38.3%, and 73.1%, respectively. However, it was also found in a previous clinical study that 26.9% of the lesions with >75% stenosis that required interventional therapy had no physiologically functional ischemia and thus did not need interventional therapy; according to previous clinical experience, 25% of the lesions with <50% stenosis had physiologically functional ischemia that had not been treated. Tonino et al. (15) also found that in CAG-confirmed coronary artery lesions with 50–70%, 70–90%, and 90–99% stenosis, the proportions of FFR <0.8 were 35%, 80%, and 96%, respectively. Previous clinical practice recommended that lesions with 70–90% stenosis needed interventional treatment, which led to 20% of patients with moderate and severe lesions were overtreated; in contrast, 35% of patients with borderline lesions with 50–70% stenosis had functional ischemia but were not treated. Our study revealed CAG and FFR readings could be different, that further demonstrated CAG alone has defects in assessing coronary artery ischemia in UA patients.
Moreover, our current study explored the relationship between traditional risk factors for coronary heart disease and FFR. Multivariate analysis verified that hypertension was the only independent risk factor for FFR, and HDL was the independent protective factor. Hypertension is one of the major risk factors for coronary heart disease, Tadashi Murai et al. (16) confirmed that the history of hypertension was a factor affecting the reduction in coronary flow reserve. Our current study also confirmed that the history of hypertension was an independent risk factor for FFR reduction. Besides, TG, TC and LDL were not found to affect FFR in 296 UA patients, when HDL was an independent protective factor. Thus, our study indicated that increasing the HDL level in UA patients can lower the risk of coronary artery functional ischemia. This may due to its important role in anti-inflammation, antioxidation, reverse cholesterol transport and protection of vascular endothelium (17,18). Additionally, many studies (19,20) have demonstrated that HDL is an independent predictor of coronary heart disease. The results of large-scale studies (21) including Framingham Heart Study, CTTP, and MRFIT confirmed that HDL levels were negatively correlated with the occurrence, development, and prognosis of atherosclerosis. Collectively, there is a negative correlation between the level of HDL and the incidence of coronary heart disease, and HDL plays an important role in the prevention and treatment of atherosclerosis.
Unfortunately, patient’s follow-up data was not included in this study, but it will be considered in a future study. Other limitations of our study included the retrospective design without clinical outcomes, making it unable to prove either CAG or FFR has higher accuracy in predicting intervention. More perspective studies are needed to demonstrate the further clinical implication of FFR in patients with UA.
Conclusions
CAG and FFR readings could be different. A combination of CAG and FFR may help to achieve more accurate and tailored treatment of UA. The history of hypertension is an independent risk factor for FFR in UA patients, and HDL is an independent protective factor.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by Beijing Anzhen Hospital Ethics Committee (ethic approval number: 201756X) and written informed consent was obtained from all patients.
References
- Chinese Society of Cardiology. Recommendations for the diagnosis and treatment of unstable angina pectoris. Chin J Cardiol 2000;28:409-12.
- Chinese Society of Cardiology. Guidelines for the Diagnosis and Treatment of Unstable Angina Pectoris and Non-ST-segment Elevation Myocardial Infarction. Chin J Cardiol 2007;35:295-304.
- Li J, Elrashidi MY, Flammer AJ, et al. Long-term outcomes of fractional flow reserve-guided vs. angiography-guided percutaneous coronary intervention in contemporary practice. Eur Heart J 2013;34:1375-83. [Crossref] [PubMed]
- Hu P, Tang MY, Song WC, et al. Fractional Flow Reserve Guided Percutaneous Coronary Intervention Improves Clinical Outcome with Reduced Cost in Contemporary Clinical Practice. Chin Med J (Engl) 2015;128:2000-5. [Crossref] [PubMed]
- Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105-11. [Crossref] [PubMed]
- Park SJ, Kang SJ, Ahn JM, et al. Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv 2012;5:1029-36. [Crossref] [PubMed]
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011;124:e574-651. [PubMed]
- Wallentin L, Lindhagen L, Arnstrom E, et al. Early invasive versus non-invasive treatment in patients with non-ST-elevation acute coronary syndrome (FRISC-II): 15 year follow-up of a prospective, randomised, multicentre study. Lancet 2016;388:1903-11. [Crossref] [PubMed]
- Zhou YJ, Zhao YX, Huo Y. Clinical application and practice of coronary intravascular ultrasound. Beijing: People’s Medical Publishing House, 2008.
- Group of Interventional Cardiology. Chinese society of Cardiology, Editorial Board of Chinese Journal of Cardiovascular Diseases. Chinese Guidelines on the Prevention of Cardiovascular Diseases 2012. Chin J Cardiol 2012;40:271-7.
- Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery. (EACTS)1, European Association for Percutaneous Cardiovascular Interventions (EAPCI), Wijns W, et al. Guidelines on myocardial revascularization. Eur Heart J 2010;31:2501-55. [Crossref] [PubMed]
- Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213-24. [Crossref] [PubMed]
- Fearon WF, Bornschein B, Tonino PA, et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 2010;122:2545-50. [Crossref] [PubMed]
- Reserve Ecegocao FF. Chinese Expert Consensus on Clinical Application of Fractional Flow Reserve. Chin J Cardiol 2016;44:292-7. [PubMed]
- Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol 2010;55:2816-21. [Crossref] [PubMed]
- Murai T, Lee T, Yonetsu T, et al. Variability of microcirculatory resistance index and its relationship with fractional flow reserve in patients with intermediate coronary artery lesions. Circ J 2013;77:1769-76. [Crossref] [PubMed]
- Murphy AJ, Woollard KJ, Hoang A, et al. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol 2008;28:2071-7. [Crossref] [PubMed]
- Rader DJ. Regulation of reverse cholesterol transport and clinical implications. Am J Cardiol 2003;92:42J-9J. [Crossref] [PubMed]
- Zeljkovic A, Spasojevic-Kalimanovska V, Vekic J, et al. Does simultaneous determination of LDL and HDL particle size improve prediction of coronary artery disease risk? Clin Exp Med 2008;8:109-16. [Crossref] [PubMed]
- Satoh H, Nishino T, Tomita K, et al. Risk factors and the incidence of coronary artery disease in young middle-aged Japanese men: results from a 10-year cohort study. Intern Med 2006;45:235-9. [Crossref] [PubMed]
- Gordon DJ, Probstfield JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation 1989;79:8-15. [Crossref] [PubMed]


