
Hyperprogressive disease: a distinct effect of immunotherapy?
While it has long been recognized that the majority of cancer discoveries and clinical trials ultimately fail to improve disease outcomes, only rarely have therapies appeared to worsen the clinical course of malignancy. Recent examples include the use of certain molecularly targeted therapies beyond tumors harboring the target genomic alteration. A phase 3 study of the epidermal growth factor receptor (EGFR) inhibitor gefitinib as maintenance therapy after chemoradiation for locally advanced non-small cell lung cancer (NSCLC) demonstrated an overall survival more than eight months worse than maintenance placebo (1). This difference was attributed to cancer- rather than toxicity-related factors. For KRAS or PIK3CA mutant NSCLC, the EGFR inhibitor erlotinib may have worse overall and progression-free survival than placebo (2).
Although cancer immunotherapy has demonstrated efficacy across multiple cancer types, in some cases truly revolutionizing the treatment landscape, it has also been linked with the possibility of accelerating disease progression. Increasingly, cases of so-termed hyperprogressive disease (HPD) in patients treated with immune checkpoint inhibitors in multiple disease types have been described (3). In a recent issue of JAMA Oncology, Ferrara and colleagues conducted a multicenter, retrospective study comparing the incidence of HPD in patients receiving checkpoint inhibitor therapy versus chemotherapy (4). This study is notable for its evaluation of survival endpoints, large sample size, and inclusion of patients treated with chemotherapy as a putative control population. The comparison with chemotherapy-treated cases is particularly important, as it provides an estimate of the background rate of HPD in lung cancer. In this analysis, HPD was defined as response evaluation criteria in solid tumors (RECIST)-defined progressive disease at first evaluation plus an absolute increase in tumor growth rate (TGR) by 50% per month after treatment initiation. Cases with pre-treatment TGR (TGRpre) less than 50% required greater than two-fold increase in TGR. With these parameters, HPD occurred in 14% of patients treated with immunotherapy (N=406), compared to 5% of patients receiving chemotherapy (N=59). HPD was associated with decreased overall survival. Among several case characteristics investigated, only high metastatic burden predicted HPD.
As with the entity known as pseudoprogression, HPD raises questions about the optimal means of assessing disease response in patients treated with immunotherapy. Pseudoprogression refers to transient radiographic worsening—new and/or enlarging tumor lesions—prior to subsequent regression. This phenomenon is thought to represent an early influx of tumor-directed immune cells resulting in an early increase in tumor dimensions. Although pseudoprogression is thought to occur in only a minority of cases, these considerations have led to modified radiographic criteria to assess therapeutic response. Immune-related response evaluation criteria in solid tumors (iRECIST) account for modest tumor enlargement and/or emergence of new disease sites without deeming a cancer to have progressed (5,6). Importantly, some reported patterns of pseudoprogression would also meet criteria for HPD, raising the possibility that at least some cancers with apparent accelerated growth could eventually respond.
Further complicating the understanding of HPD, various definitions have been proposed (Table 1). To date, the most commonly used parameters incorporate at least a doubling of TGR after treatment initiation. Champiat and colleagues defined hyperprogression as RECIST-defined progressive disease at first evaluation, with a minimum two-fold increase in tumor growth rate after initiation of therapy (TGRpost) compared to the TGRpre (3). TGR, in turn, has been defined as percentage increase in tumor volume over one month (9). Saada-Bouzid and colleagues employed tumor growth kinetics (TGK), defined as the change in sum of diameters (according to RECIST) per unit of time (7). HPD was defined as a ratio of the post-treatment TGK to pre-treatment TGK (TGKpost/TGKpre) of two or more. Other criteria have incorporated time to treatment failure and absolute increase in TGR (8).

Full table
Across studies, the incidence of HPD among immunotherapy cases ranges from 10–30% (3,4,7). This variation may reflect small sample sizes, differences in HPD definition, differences in cancer type, or availability of radiographic data. The current study by Ferrara and colleagues constitutes the largest series yet reported, more than three times the size of other published cohorts ranging up to 131 patients. For several reasons, rates of HPD may be underestimated in all studies. Generally, inclusion in studies of HPD requires cases to have serial baseline scans prior to the therapy in question. Cases without these time-points are excluded, even if they feature a particularly high rate of tumor growth post treatment. Patients who do not receive a post-treatment scan—possibly due to clinical deterioration, disease progression, or death—are removed. Additionally, no proposed definition of HPD accounts for RECIST non-target lesions such as malignant effusions, bone metastases, or new disease sites.
A number of different patient and tumor characteristics have been associated with the likelihood of HPD (Table 2). These include genomic features such as MDM2 amplification, prior radiation therapy, and advanced age (3,7,8,10). In patients with NSCLC or melanoma treated with immune checkpoint inhibitor therapy, elevated lactate dehydrogenase (LDH) levels and a neutrophil-to-lymphocyte ratio greater than three were significantly correlated with worse survival (11). In the study by Ferrara and colleagues, there was no association between HPD and patient age, serum LDH levels, or neutrophil:lymphocyte ratio (4). However, the authors identified a correlation between HPD and increased metastatic burden, defined as more than two metastatic sites prior to initiation of anti PD-1/PDL-1 therapy (P=0.006). It has also been suggested that instances of HPD are less frequently associated with emergence of new lesions compared to non-hyper PD, although this observation may reflect current HPD definitions (3). In any case, small numbers of patients, heterogeneous study populations, and diverse HPD definitions in published studies limit the ability to render conclusions about HPD predictive factors.
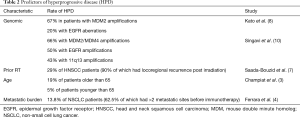
Full table
What biologic mechanisms underlie HPD? A recently published study identified numerous signaling pathways that were upregulated after anti PD-1 therapy that were not originally mutated, suggesting significant alteration of the mutational landscape after anti PD-1 therapy (12). Specifically, the investigators noted increased expression of oncogenic pathways, as well as mutations in known tumor suppressor genes, such as VHL and TSC2. Post-therapy HPD tumors have been noted to have decreased expression of human leukocyte antigens (HLA) and upregulation of several immune checkpoints and modulators including CTLA4, KDR, and CD96 (12). It has also been proposed that decreased immunogenicity plays a role in HPD, with occurrence more frequent with an immunosuppressive phenotype (13).
While it may be years before the mechanisms and predictors of HPD are fully understood, clinicians currently face critical, real-world management questions on a daily basis. Although radiographic evaluation of therapeutic effect is typically straightforward with conventional chemotherapy or molecularly targeted therapy, phenomena such as HPD and pseudoprogression complicate such assessments when using immunotherapy. For patients receiving immune checkpoint inhibitors, how do we reliably distinguish between standard progression, hyperprogression, and pseudoprogression? In what cases should immunotherapy be continued beyond radiographic worsening, with the hopes of eventual response? In a retrospective analysis of second-line immunotherapy trials in advanced NSCLC, it was shown that patients who continued to receive anti-PD-1 therapy after RECIST-defined progression had similar outcomes to patients with stable disease (14). Of course, each treating clinician had some rationale for continuing treatment despite progressive disease in these particular cases. Even some patients with initial HPD in the study by Ferrara and colleagues subsequently demonstrated pseudoprogression, suggesting that even accelerated tumor growth may not be a sufficient predictor of true disease progression (4).
Designing clinical trials to understand the incidence, predictors, and nature of patterns such as pseudoprogression and HPD is not straightforward. A study of immunotherapy in which all patients continue treatment beyond apparent progression could provide key insights into pseudoprogression, but is not clinically practical or ethically feasible. A study of placebo versus immunotherapy in patients with radiographically evident advanced cancer could help characterize HPD, but faces similar limitations. In the absence of such high-level data, clinicians will need to incorporate findings from retrospective reports, as well as their own clinical acumen, to inform, monitor, and manage the growing number of patients treated with immunotherapy.
Acknowledgements
The authors thank Ms. Dru Gray for assistance with manuscript preparation and Helen Mayo, MLS, from the UT Southwestern Medical Library, for assistance with literature searches.
Funding: Supported in part by a National Cancer Institute Midcareer Investigator Award in Patient-Oriented Research (K24 CA201543-01), an American Cancer Society-Melanoma Research Alliance Team Award (MRAT-18-114-01-LIB), and a V Foundation Robin Roberts Cancer Survivorship Award (DT2019-007) (all to DEG).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kelly K, Chansky K, Gaspar LE, et al. Phase III trial of maintenance gefitinib or placebo after concurrent chemoradiotherapy and docetaxel consolidation in inoperable stage III non-small-cell lung cancer: SWOG S0023. J Clin Oncol 2008;26:2450-6. [Crossref] [PubMed]
- Ludovini V, Bianconi F, Pistola L, et al. Phosphoinositide-3-kinase catalytic alpha and KRAS mutations are important predictors of resistance to therapy with epidermal growth factor receptor tyrosine kinase inhibitors in patients with advanced non-small cell lung cancer. J Thorac Oncol 2011;6:707-15. [Crossref] [PubMed]
- Champiat S, Dercle L, Ammari S, et al. Hyperprogressive Disease Is a New Pattern of Progression in Cancer Patients Treated by Anti-PD-1/PD-L1. Clin Cancer Res 2017;23:1920-8. [Crossref] [PubMed]
- Ferrara R, Mezquita L, Texier M, et al. Hyperprogressive Disease in Patients With Advanced Non-Small Cell Lung Cancer Treated With PD-1/PD-L1 Inhibitors or With Single-Agent Chemotherapy. JAMA Oncol 2018;4:1543-52. [Crossref] [PubMed]
- Tazdait M, Mezquita L, Lahmar J, et al. Patterns of responses in metastatic NSCLC during PD-1 or PDL-1 inhibitor therapy: Comparison of RECIST 1.1, irRECIST and iRECIST criteria. Eur J Cancer 2018;88:38-47. [Crossref] [PubMed]
- Seymour L, Bogaerts J, Perrone A, et al. iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol 2017;18:e143-e52. [Crossref] [PubMed]
- Saada-Bouzid E, Defaucheux C, Karabajakian A, et al. Hyperprogression during anti-PD-1/PD-L1 therapy in patients with recurrent and/or metastatic head and neck squamous cell carcinoma. Ann Oncol 2017;28:1605-11. [Crossref] [PubMed]
- Kato S, Goodman A, Walavalkar V, et al. Hyperprogressors after Immunotherapy: Analysis of Genomic Alterations Associated with Accelerated Growth Rate. Clin Cancer Res 2017;23:4242-50. [Crossref] [PubMed]
- Ferte C, Fernandez M, Hollebecque A, et al. Tumor growth rate is an early indicator of antitumor drug activity in phase I clinical trials. Clin Cancer Res 2014;20:246-52. [Crossref] [PubMed]
- Singavi AKSMDKAAPSRJPTALMCOSA. Predictive biomarkers for hyper-progression (HP) in response to immune checkpoint inhibitors (ICI) – analysis of somatic alterations (SAs). Annals of Oncology 2017.25.
- Mezquita L, Auclin E, Ferrara R, et al. Association of the Lung Immune Prognostic Index With Immune Checkpoint Inhibitor Outcomes in Patients With Advanced Non-Small Cell Lung Cancer. JAMA Oncol 2018;4:351-7. [Crossref] [PubMed]
- Xiong D, Wang Y, Singavi AK, et al. Immunogenomic Landscape Contributes to Hyperprogressive Disease after Anti-PD-1 Immunotherapy for Cancer. iScience 2018;9:258-77.
- Faure M, Rochigneux P, Olive D, et al. Hyperprogressive Disease in Anorectal Melanoma Treated by PD-1 Inhibitors. Front Immunol 2018;9:797. [Crossref] [PubMed]
- Kazandjian D, Keegan P, Suzman DL, et al. Characterization of outcomes in patients with metastatic non-small cell lung cancer treated with programmed cell death protein 1 inhibitors past RECIST version 1.1-defined disease progression in clinical trials. Semin Oncol 2017;44:3-7. [Crossref] [PubMed]


