Longitudinal changes in depression screening results in cardiac surgery patients
Introduction
The global burden of heart disease and unipolar depression is forecasted to exceed all other medical illness by year 2020 (1). The prevalence of depression in primary care settings has been shown to range between 5–10% in different countries, the prevalence of major depression is two-times higher in women than men and depression is associated with increased morbidity and mortality in the general population (2). Among patients with heart disease the prevalence of major depression has been reported to be between 15% and 40% (3,4). Depression can have profound effects on social functioning, quality of life, and physical health through associations with cardiovascular disease, the leading cause of preventable death worldwide. An association between depression and increased morbidity and mortality has been confirmed among patients going through cardiac surgery (5-8). Patients going through cardiac surgery have reported poorer health related quality of life than the general population (9,10). This is in line with what has been reported in other cardiovascular disease populations (11,12).
Depression can be hard to detect if only traditional depression symptoms are taken into account (13). The American Heart Association and the US Preventive Services Task Force recommend depression screening in all patients with heart disease since 2008 (14). This suggestion has not been without controversy as there is limited evidence for benefits from depression screening, such as improved coronary heart disease and depression outcomes (15,16). However, Smolderen and colleagues recently showed that patients with myocardial infarction and treated depression had 1-year mortality rates that were similar to patients without depression. On the other hand, patients with untreated depression had higher 1-year mortality in comparison with patients without depression (17).
In a prior study, we investigated the feasibility of a depression screening program in cardiac surgery patients and found a satisfactory response-rate in elective patients (18). The aim of the present study was to investigate longitudinal changes in depression screening results up to one year following surgery, and to evaluate the results separately for men and women.
Methods
Study design
This was a prospective population-based study. We introduced a depression screening project at the cardiac surgery department at Karolinska University Hospital between 2013 and 2016. The project was approved by the human research ethics committee in Stockholm (Dnr: 2013/35-31/4). All participants gave informed consent before entering the study. The Swedish version of PHQ-9 was used. The PHQ-9 is a validated depression screening instrument in patients with heart disease and recommended by the American Heart Association (19). Patients scheduled for elective surgery received the PHQ-9 by mail about 2 weeks before surgery. Urgent patients were asked, if possible, to fill out the PHQ-9 prior to surgery on the ward as part of the standard clinical routine. Baseline characteristics, medical history, and medications were gathered from patient charts, and registered in a study database with the results from the PHQ-9 questionnaires. One year after the surgical procedure all patients who had filled out PHQ-9 at baseline were sent the PHQ-9 with a letter asking to fill out the questionnaire again and send it back with the enclosed prepaid envelope.
Population
All patients above 18 years of age planned for heart surgery at Karolinska University Hospital were eligible for inclusion in the study.
Screening instrument
The PHQ-9 includes the 9 criteria upon which the diagnosis of DSM-IV depressive disorders is based, and is a 9-item self-report questionnaire that assesses symptoms of depression. The 9 items of PHQ-9 can be scored from 0 (not at all) to 3 (nearly every day) per separate item, and overall scores can range from 0 to 27. A score ≥10 is considered predictive for an episode of major depression with a sensitivity and specificity of 88% (19). The 9 items ranges from item 1: “Little interest or pleasure in doing things?” to item 9 that identifies suicidal ideation and states: “Over the last 2 weeks, how often have you been bothered by the following problem: thoughts that you would be better off dead, or of hurting yourself in some way?”. Answer choices and scores are as follows: “not at all” (score 0), “several days” (score 1), “more than half the days” (score 2), or “nearly every day” (score 3). The PHQ-9 questionnaire is filled out by the patient and only takes a few minutes.
Statistical analysis
Baseline characteristics were described with frequencies and percentages for categorical variables and means and standard deviations for continuous variables. We used t tests for continuous variables and chi-square tests for categorical variables.
Results
Baseline characteristics
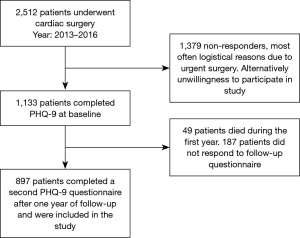
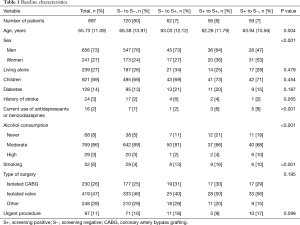
During the period 2013–2016, 2,512 patients underwent cardiac surgery; 1,133 (45%) completed PHQ-9 before surgery and were included in the study. Among patients scheduled for elective surgery 990/1,544 (64%) completed the PHQ-9 questionnaire at baseline, and among urgent patients the response rate was 143/968 (15%). Fifteen percent (166/1,133) had a PHQ-9 score ≥10 suggestive of major depression at baseline. Reporting elevated depression scores were twice as common in women as in men 23% vs. 12% at baseline. One year after surgery, 1,084 patients were alive, of these 897 (83%) persons filled out PHQ-9 again. Our final cohort consisted of 897 patients with a completed PHQ-9 at baseline and after one year (Figure 1). The total mean age was 65.73 years, including 656 men (73%) and 241 women (27%) (Table 1). Patients that remained screening positive from baseline to follow-up after one year were younger and more often active smokers compared with patients that were screening negative at baseline or at follow up. This was also noted among patients with at least one positive depression screen at any time during the study (Table 1).
Full table
Longitudinal changes
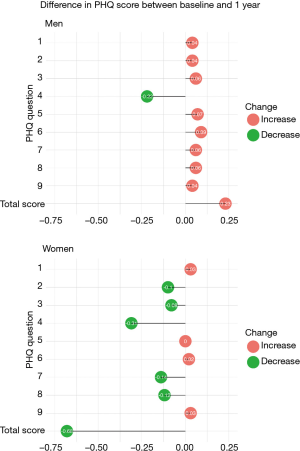
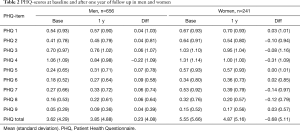
The majority of patients, both men and women, that were screening negative at baseline were still screening negative after one year. At follow up, 547 (92%) men and 173 (91%) women that were screening negative at baseline were still screening negative at follow-up after one year (Figure 2). There was no difference between men and women. A lower proportion of men compared with women (44% vs. 61%) improved from screening positive at baseline to screening negative after one year of follow-up, although this difference was not statistically significant (P=0.069). The total score difference in PHQ between baseline and one year had increased with 0.23 points among men and decreased with 0.68 points in women (Table 2 and Figure 3). Item 4 “feeling tired or having little energy” was the only item with a decreased score in men after one year. Among women five of nine items had decreased scores, including item 4, which was the item with the most apparent change in both men and women. Among patients who were screening negative at baseline, 7.6% of the men and 8.9% of the women, were screening positive after one year of follow-up.
Full table
Discussion
In this population-based prospective cohort study investigating the one year longitudinal outcomes of depression screening in cardiac surgery patients, we found that a positive depression screen at baseline was twice as common in women compared to men. Women who screened positive at baseline were to a larger extent than men screening negative after one year. Women generally decreased in PHQ-9 scores after one year while men increased in PHQ-9 scores on average. Almost 10% of those who were screening negative at baseline, were screening positive after one year.
In a longitudinal study by Tully et al., PHQ was administered 30 days after cardiac surgery and was re-administered after six-month follow-up (10). They found that approximately 10% had a positive depression screen at baseline and at 6 months follow-up and that patients with a positive depression screen was at a higher risk of major adverse cardiac events and reported significantly poorer quality of life (10). The proportion of patients who were screening positive at baseline and after one year of follow-up in our study was similar to what was reported by Tully et al. (10).
A recent longitudinal study investigated the impact of elevated depression scores on HADS preoperatively and one year after coronary artery bypass grafting (CABG) on all-cause mortality after 11 years. Like in our study the proportion of patients with elevated depression and anxiety scores was greater among women. The researchers found in their analysis by sex that both men and women that symptoms of depression were associated with increased mortality but results from the sex-specific analyses showed no evidence of sex-disparities (20).
In a study by Mallik et al. it was found that depressive symptom severity at baseline was associated with lower improvement in functional status at 6 months after CABG (21). This association was stronger in women than in men. Physical and psychological functioning were assessed the month before CABG with the Medical Outcomes Trust Short Form 36-Item Health Survey (SF-36). The association between depressive symptom severity at baseline and lower improvement in functional status at 6 months after CABG could be due to poorer diets, hygiene, self-care, compliance with cardiac treatment regimens and low participation in cardiac rehabilitation (21,22).
In our study we found that women improved in depression scores to a larger extent than men. The gender difference in depressive disorder is a complex integration of biology, society and culture (23). One possible explanation to our findings, that more women than men with depressive symptoms at baseline seem to improve over a 12 months period, could be that it is more socially acceptable for women to seek medical help. Traditional depressive symptoms (e.g., sadness, crying) may not be in line with societal ideals of masculinity. Therefore, men might be reluctant to report experiencing these symptoms and seek help (13). It could also be that depression takes different shapes in men and women. Anger, irritability, risk-taking behaviors, and substance abuse can be symptoms of depression in men replacing more traditional symptoms such as sleep problems and withdrawal from social occasions (13).
Palacios et al. investigated the long-term trajectories of anxiety and depression in a cohort of 803 patients with coronary heart disease (24). The patients were assessed every 6 months for 3 years. Despite consistent reporting of high depression and anxiety symptoms, only approximately half of the patients had these symptoms mentioned in their medical notes (24). This suggests that it is difficult to identify mental comorbidity in patients with cardiac disease and repeated depression screening could be helpful.
Previous studies regarding depression and heart disease have focused on patients with coronary artery disease and the possible link between depression and inflammation. In a preplanned study to The Frailty Aortic Valve Replacement study (25), Drudi et al. showed that depression is highly prevalent among patients with aortic stenosis undergoing transcatheter aortic valve replacement and surgical aortic valve replacement, affecting as many as 1 in 3 patients, and seems to be associated with a increased risk of all-cause mortality (26). They found that patients with a persistent depression from baseline to 12 months had a significantly higher mortality risk than those with resolved depression. Our study included patients with different types of heart disease and the prevalence of depression was 15%. This indicates that depression screening is important in all patients with heart disease.
Limitations
A strength of our study includes the prospective population-based design. All patients received standard of care but we lack information regarding possible depression treatment during follow-up. Other limitations included the lack of a clinical examination by a psychiatrist and that we did not record postoperative complications in the study.
Conclusions
We found that twice as many women as men had a positive depression screen at baseline, and that almost 10% of all who were screening negative at baseline, were screening positive after one year. Women who screened positive at baseline were to a larger extent than men screening negative after one year, and women decreased in PHQ-9 scores, whereas men tended to increase their scores. Our results indicate that repeated screening is probably of value in both men and women in order to detect symptoms of depression because if depression is detected, it is more likely to be treated.
Acknowledgements
Funding: This work was supported by grants from the Swedish Society of Medicine (grant number SLS-593391 to U Sartipy); the Swedish Heart-Lung Foundation (grant numbers 20160522, 20160525 to U Sartipy); the Mats Kleberg Foundation (grant number 2017-00096 to U Sartipy); Karolinska Institutet Foundations and Funds (grant number 2016fobi47721 to U Sartipy); Swedish Heart and Lung Association (grant number E101/16 to U Sartipy]; Åke Wiberg Foundation (grant number M17-0089 to U Sartipy); Magnus Bergvall Foundation (grant number 2017-02054 to U Sartipy); the regional ALF agreement between Stockholm County Council and Karolinska Institutet (grant number 20160329 to U Sartipy).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the human research ethics committee in Stockholm (Dnr: 2013/35-31/4) and written informed consent was obtained from all patients.
References
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997;349:1498-504. [Crossref] [PubMed]
- Shanmugasegaram S, Russell KL, Kovacs AH, et al. Gender and sex differences in prevalence of major depression in coronary artery disease patients: a meta-analysis. Maturitas 2012;73:305-11. [Crossref] [PubMed]
- Connerney I, Shapiro PA, McLaughlin JS, et al. Relation between depression after coronary artery bypass surgery and 12-month outcome: a prospective study. Lancet 2001;358:1766-71. [Crossref] [PubMed]
- Celano CM, Huffman JC. Depression and cardiac disease: A review. Cardiol Rev 2011;19:130-42. [Crossref] [PubMed]
- Burg MM, Benedetto MC, Rosenberg R, et al. Presurgical depression predicts medical morbidity 6 months after coronary artery bypass graft surgery. Psychosom Med 2003;65:111-8. [Crossref] [PubMed]
- Stenman M, Holzmann MJ, Sartipy U. Antidepressant use before coronary artery bypass surgery is associated with long-term mortality. Int J Cardiol 2013;167:2958-62. [Crossref] [PubMed]
- Stenman M, Holzmann MJ, Sartipy U. Relation of major depression to survival after coronary artery bypass grafting. Am J Cardiol 2014;114:698-703. [Crossref] [PubMed]
- Blumenthal JA, Newman M, Babyak MA, et al. Depression as risk factor for mortality after coronary artery bypass surgery - Reply. Lancet 2003;362:604-9. [Crossref] [PubMed]
- Lichtman JH, Froelicher ES, Blumenthal JA, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation 2014;129:1350-69. [Crossref] [PubMed]
- Tully PJ, Baumeister H, Bennetts JS, et al. Depression screening after cardiac surgery: A six month longitudinal follow up for cardiac events, hospital readmissions, quality of life and mental health. Int J Cardiol 2016;206:44-50. [Crossref] [PubMed]
- Pizzi C, Rutjes AW, Costa GM, et al. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. Am J Cardiol 2011;107:972-9. [Crossref] [PubMed]
- de Miranda Azevedo R, Roest AM, Carney RM, et al. Individual depressive symptoms and all-cause mortality In 6673 patients with myocardial infarction: Heterogeneity across age and sex subgroups. J Affect Disord 2018;228:178-85. [Crossref] [PubMed]
- Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: analysis of the National Comorbidity Survey Replication. JAMA Psychiatry 2013;70:1100-6. [Crossref] [PubMed]
- Siu AL, Bibbins-Domingo K, Grossman DC, et al. Screening for Depression in Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2016;315:380-7. [Crossref] [PubMed]
- Subramanian DN, Hopayian K. An audit of the first year of screening for depression in patients with diabetes and ischaemic heart disease under the Quality and Outcomes Framework. Qual Prim Care 2008;16:341-4. [PubMed]
- Larsen KK, Vestergaard M, Sondergaard J, et al. Screening for depression in patients with myocardial infarction by general practitioners. Eur J Prev Cardiol 2013;20:800-6. [Crossref] [PubMed]
- Smolderen KG, Buchanan DM, Gosch K, et al. Depression Treatment and 1-Year Mortality After Acute Myocardial Infarction: Insights From the TRIUMPH Registry (Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients' Health Status). Circulation 2017;135:1681-9. [Crossref] [PubMed]
- Stenman M, Sartipy U. Depression screening in cardiac surgery patients. Heart Lung Circ 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. [Crossref] [PubMed]
- Geulayov G, Novikov I, Dankner D, et al. Symptoms of depression and anxiety and 11-year all-cause mortality in men and women undergoing coronary artery bypass graft (CABG) surgery. J Psychosom Res 2018;105:106-14. [Crossref] [PubMed]
- Mallik S, Krumholz HM, Lin ZQ, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation 2005;111:271-7. [Crossref] [PubMed]
- Carney RM, Freedland KE, Rich MW, et al. Depression as a risk factor for cardiac events in established coronary heart disease: a review of possible mechanisms. Ann Behav Med 1995;17:142-9. [Crossref] [PubMed]
- Maji S. Society and 'good woman': A critical review of gender difference in depression. Int J Soc Psychiatry 2018;64:396-405. [Crossref] [PubMed]
- Palacios J, Khondoker M, Mann A, et al. Depression and anxiety symptom trajectories in coronary heart disease: Associations with measures of disability and impact on 3-year health care costs. J Psychosom Res 2018;104:1-8. [Crossref] [PubMed]
- Afilalo J, Lauck S, Kim DH, et al. Frailty in Older Adults Undergoing Aortic Valve Replacement: The FRAILTY-AVR Study. J Am Coll Cardiol 2017;70:689-700. [Crossref] [PubMed]
- Drudi LM, Ades M, Turkdogan S, et al. Association of Depression With Mortality in Older Adults Undergoing Transcatheter or Surgical Aortic Valve Replacement. JAMA Cardiol 2018;3:191-7. [Crossref] [PubMed]