Relation of late gadolinium enhancement in cardiac magnetic resonance on the diastolic volume recovery of left ventricle with hypertrophic cardiomyopathy
Introduction
Cardiac magnetic resonance (CMR) plays an important role in the diagnosis of hypertrophic cardiomyopathy (HCM). Besides routine evaluation of cardiac structure and function, late gadolinium enhancement (LGE) of myocardium has the potential to demonstrate replacement fibrosis, a potential marker of poor outcome LGE was considered replacement of fibrosis (1). Pathologically, fibrotic myocardium is believed to be the basis of re-entrant ventricular arrhythmia as well as myocardial dysfunction. Quite a few studies (2-5) had demonstrated prognostic value of LGE in HCM recently. Presence and extent of LGE have been shown to correlate with the incidence of major adverse cardiac events (MACE), and has prognostic value which is additive to standard clinical markers.
LGE affects the prognosis of HCM patients, but the changes on cardiac structure and function associated with LGE from the fibrosis (6) may affect prognosis because of altered diastolic function. Diastolic dysfunction usually appears before systolic function in HCM (7), but is generally not assessed on clinical CMR. Left ventricular volume filling curve or volume time curve is a potential method to evaluate diastolic function, but little clinical date is available in patients with HCM. Early data from Kawaji et al. (8) and Motoyasu et al. (7) found the reduced diastolic function in HCM patients compared with normal volunteers, but the relationship of these findings to factors that have been shown related with prognosis, such as LGE, are unclear. Our study was to assess correlation between diastolic function and presence or absence of LGE.
Materials and methods
Patients population
It was a retrospective study. A total of 34 consecutive patients with HCM undergoing CMR were studied from January 2010 to November 2012. The clinical diagnosis of HCM was established with echocardiography, CMR, electrocardiogram, laboratory examination, family history and other clinical data. The patients with atrial fibrillation and claustrophobia were excluded before examination. Ten patients were excluded because of former alcohol ablation (six patients) or no contrast scan (four patients). The rest 24 patients were composed of 13 obstructive HCM patients and 11 non-obstructive HCM (three apical obstructive HCM patients). These 24 patients were divided into two groups, LGE positive group and LGE negative group. The study was approved by the institutional ethics committees, and every patient was gave informed consent before examination.
CMR protocol
CMR images were obtained on a 1.5-T system (Signa CV/i, GE Healthcare, Milwaukee, USA), using an eight channel phased array coil and electrocardiographic triggering. All patients underwent an standard examination, which included a short axis bright-blood cine sequence (Fiesta) covering the entire left ventricule with a slice thickness of 8 mm, gap of 2 mm, TR/TE =35/1.5 ms, FLIP angle =45°, FOV =360 mm × 280 mm, VPS (views per segment) =14, slice reconstructed cardiac phases =20. Myocardial delay enhancement (MDE) images were acquired about ten minutes after the injection of 0.2 mmol/kg of GD-DTPA (Magnevist, Schering, Berlin, Germany), TR =6.5 ms, TE =3.0 ms, FLIP angle =20°, FOV =360 mm × 270 mm, VPS =24, slice thickness =8 mm, gap =2 mm, TI = 170-280 ms, including two-chamber view, four-chamber view and axial images (about 6-9 slices from the apex to base).
Images analysis
Automated segmentation of left ventricle
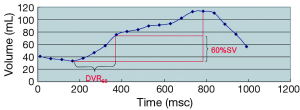
Automated segmentation of left ventricle was performed using report-card 4.0 (GE Health Care, USA). Indices obtained included end systole volume (ESV), end diastole volume (EDV), left ventricular ejection fraction (EF), peak ejecting rate (PER), normalized peak ejecting rate (NPER), time to peak ejecting rate (TPER), peak filling rate (PFR), normalized peak filling rate (NPFR), time to peak filling rate (TPFR) and diastolic volume recovery (DVR) (9) (Figure 1). Left ventricular volume was defined as the range from the apex to annulus of mitral valve, the papillary muscle was excluded from the volume and included in the left ventricular mass (10). At the base, slices were deemed to be within the left ventricle when the volume was encircled by 50% or more of ventricular myocardium (11), otherwise, they were considered to be within the left atrium and excluded. The function of LV analysis was part of report-card 4.0, it was used for analyzing the left ventricular filling curve. The endomyocardium was segmented automatically in all axial images that were defined as left ventricular volume, and the curve of left ventricular filling was generated, along with the indexes of cardiac function.
PER=△V/△T, PER is the peak rate of left ventricular ejecting, calculated from the difference between two continuous cardiac phases, then divided by the time between two cardiac phases.
NPFR=PFR/EDV, normalized PFR.
NPER=PER/EDV, normalized PER.
TPFR is the time between end systole and PFR. TPER meant the time between end diastole and PER, DVR was defined as the percent of the time of diastolic volume recovery that occupying the diastolic time.
DVR60 is the proportion of diastole required to recover 60% left ventricular stroke volume (Figure 1).
DVR10-DVR100 was calculated through Matlab R2011a (Mathworks, USA).
The wall thickening of left ventricle (WT%) = (wall thickness at end systole-wall thickness at end diastole)/wall thickness at end systole. Fractional shortening (FS) of left ventricle = (end diastole diameter-end systole diameter)/end diastole diameter ×100%, left ventricular remodeling index (LVRI) = left ventricular mass/EDV (12), left ventricular mass was the mass calculated at diastole. The ratio of wall thickness (RWT) = the thickness of hypertrophied wall/the thickness of normal wall.
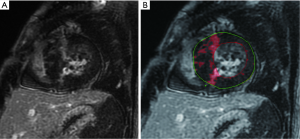
LGE analysis
Quantitative evaluation of LGE was performed with myocardial evaluation (ME), part of report-card 4.0. A region (about 50 mm2) of interest (ROI) was placed in each slice of axial MDE images, and the signal intensity was acquired [mean + standard deviation (SD)]. The extent of LGE was calculated automatically in each slice, as well as the mass of LGE, and the proportion of total left ventricular mass, according to the formula (the threshold = mean + 6SD) (13), (Figure 2A,B). The last step was to check the extent of LGE, and made some adjustment by an experienced radiologist (more than five years’ experience in CMR).
Statistical analysis
All data was presented as mean ± SD or percentage. t-test of independent samples was used to analyze the continuous data between the positive group and negative group. Non-parametric test was used to analyze the categorical variables. The correlation between variables was analyzed with Pearson correlation or Spearman correlation. The former one was for continuous data, and the latter one for categorical variables. Statistical analysis was performed using SPSS for windows (version 16.0; SPSS Inc., Chicago, IL, USA). P value <0.05 was considered statistically significant.
Results
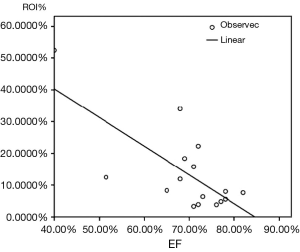
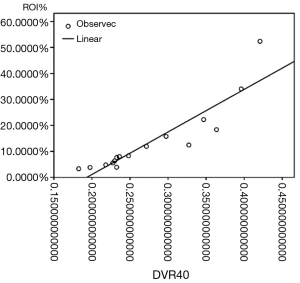
In the 24 HCM patients, 16 patients were LGE positive, and eight were LGE negative. The incidences of diabetes mellitus, hypertension, family history, and NYHA class were not significant between two groups (Table 1). The indexes of LGE positive group such as DVR10-40, DVR100, ESV, ESVI and ESD were greater than LGE negative group. The indexes of, FS, NPFR, SV, SVI, EF, CO, CI and FS were smaller in LGE positive group, but the differences were still statistically significant (Tables 2,3). In the LGE positive group, the average LGE mass (ROI) was 20.78 g, the mean LGE proportion (ROI%) was 13.67% among 16 LGE positive patients. The correlation analysis between the extent of LGE and structural and functional indexes showed that LGE (ROI%) was correlated with ESV, EF, FS, PFR, TPER, DVR20-50, DVR80, all P values <0.05 (Table 4). The most correlative index was DVR40, the correlation coefficient was 0.906. The LGE (ROI%) correlated with ESV, ESVI, EF well; the correlation coefficients were both greater than 0.7 (Figures 3,4).
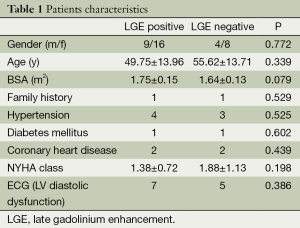
Full table
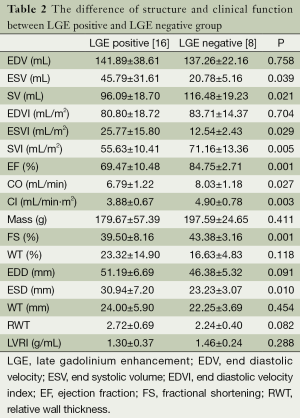
Full table
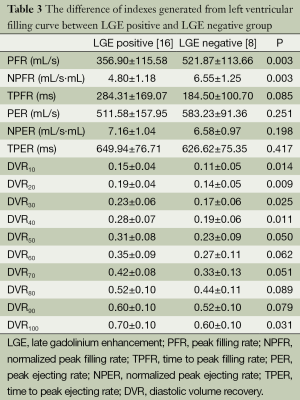
Full table
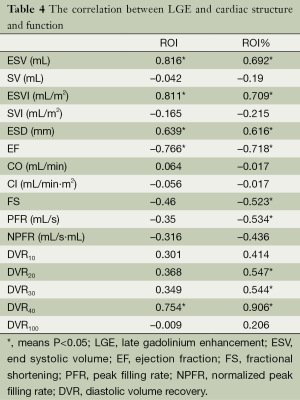
Full table
Discussion
Our study highlights the potential of novel MR markers of diastolic function to provide additional, potentially prognostic data in patients with hypertrophic cardiomyopathy. Previous work has shown it feasible to evaluate heart diseases through the left ventricular filling curve (9,14,15). Currently, there is much interest in LGE in cardiomyopathies such as HCM seen on CMR (7,8,16). The correlation between LGE and the changes of structure and function also were seen in recent studies (15,17,18). The study of Choi et al. (17) revealed the extent of LGE correlated with PFR, TPFR and NPFR. Another research done by Catalano et al. (15) showed the extent of LGE correlated with the size of left atrium. However, there were few studies on the correlation between DVR and the extent of LGE. In our study, a negative correlation between LGE and PFR was observed, and correlation between LGE and DVR was also found.
In contrast to the LGE negative group, indexes of the LGE positive group, such as ESV, DVR10-40, DVR100, ESV, ESVI and ESD were greater, and, FS, NPFR, SV, SVI, EF, CO and CI were smaller. It is possible that this is related to the extent of fibrosis revealed by LGE. We believed that the higher extent of fibrosis led to the more severely remodeling LV structure. Though EF and FS decreased more in the LGE positive group, the mean value of EF was still in normal range. Our study showed that the EF and FS was normal in LGE positive group, it was significantly lower than LGE negative positive group. The possible reason could be relative to the higher systolic function in HCM patients (higher EF and FS) compared normal individuals. The relations of LGE on diastolic function was suggested by changes in PFR, NPFR, DVR20-40, DVR100, with a decreased or increased of these indexes revealed the dysfunction of left ventricle. The ESV, ESVI, ESD were greater in LGE positive group, the probable reason may be correlated with thicker myocardium. The SV, SVI, CO, CI and FS were indexes of systolic function, and these indexes were smaller in LGE positive group. We considered the changes reflect the relations with LGE (main reflection of myocardium fibrosis). PFR, NPFR, DVR10-40 and DVR100 were indexes of diastolic function. PFR, NPFR were smaller, DVR10-40 and DVR100 were bigger, DVR100 represented the total diastolic procedure, the prolonged of DVR100 showed the diastolic restriction. Moreover, the prolonged of DVR10-40 showed early diastolic restriction. This revealed the details of diastolic restriction.
Our results suggest that the extent of LGE is related to underlying pathology which alters diastolic function and structure remodeling and that the resulting altered dysfunction can be demonstrated by MR-derived markers. The correlation coefficients of ESV, ESVI and EF were both bigger than 0.7, which show the correlation were comparatively good. The decreasing of PFR generated from the filling curve showed left ventricular diastolic restriction, the left ventricular filling curve showed more detail of diastolic restriction. LGE (ROI%) had positive correlation with the indexes of DVR20 (r=0.547), DVR30 (r=0.544), DVR40 (r=0.906), DVR50 (r=0.908), DVR80 (r=0.608), but the differences of DVR50 and DVR80 between LGE positive group and LGE negative group were insignificant. This result meant diastolic restriction was represented in rapid filling period. We considered LGE influenced early diastolic volume recovery. The limitation and pitfalls mainly lied in the comparatively small sample size from a single center study. In addition, correlation of these MR-derived parameters with clinical outcomes is needed, in order to determine whether their use provides incremental or additional prognostic information compared to standard assessment of LGE on clinical CMR.
Conclusions
Our study demonstrated correlation of MR-derived markers of diastolic dysfunction with LGE on CMR. These parameters may provide further potential for CMR to provide prognostic information in patients with HCM.
Acknowledgements
We thank Philip Young for his technical assistance. This study was supported in part by the National Natural Science Foundation of China under Grant 30870671, and by the Natural Science Foundation of Zhejiang Province under Grant R207119, and by the Health and Family Planning Commission of Zhejiang Province under Grant 201463675.
Disclosure: The authors declare no conflict of interests.
References
- Maron MS. Clinical utility of cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J Cardiovasc Magn Reson 2012;14:13. [PubMed]
- Fluechter S, Kuschyk J, Wolpert C, et al. Extent of late gadolinium enhancement detected by cardiovascular magnetic resonance correlates with the inducibility of ventricular tachyarrhythmia in hypertrophic cardiomyopathy. J Cardiovasc Magn Reson 2010;12:30. [PubMed]
- Aquaro GD, Masci P, Formisano F, et al. Usefulness of delayed enhancement by magnetic resonance imaging in hypertrophic cardiomyopathy as a marker of disease and its severity. Am J Cardiol 2010;105:392-7. [PubMed]
- Nojiri A, Hongo K, Kawai M, et al. Scoring of late gadolinium enhancement in cardiac magnetic resonance imaging can predict cardiac events in patients with hypertrophic cardiomyopathy. J Cardiol 2011;58:253-60. [PubMed]
- Appelbaum E, Maron BJ, Adabag S, et al. Intermediate-signal-intensity late gadolinium enhancement predicts ventricular tachyarrhythmias in patients with hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 2012;5:78-85. [PubMed]
- Boonyasirinant T, Rajiah P, Setser RM, et al. Aortic stiffness is increased in hypertrophic cardiomyopathy with myocardial fibrosis: novel insights in vascular function from magnetic resonance imaging. J Am Coll Cardiol 2009;54:255-62. [PubMed]
- Motoyasu M, Kurita T, Onishi K, et al. Correlation between late gadolinium enhancement and diastolic function inhypertrophic cardiomyopathy assessed by magnetic resonance imaging. Circ J 2008;72:378-83. [PubMed]
- Kawaji K, Codella NC, Prince MR, et al. Automated segmentation of routine clinical cardiac magnetic resonance imaging forassessment of left ventricular diastolic dysfunction. Circ Cardiovasc Imaging 2009;2:476-84. [PubMed]
- Mendoza DD, Codella NC, Wang Y, et al. Impact of diastolic dysfunction severity on global left ventricular volumetricfilling - assessment by automated segmentation of routine cine cardiovascularmagnetic resonance. J Cardiovasc Magn Reson 2010;12:46. [PubMed]
- Guerra M, Sampaio F, Bras-Silva C, et al. Left intraventricular diastolic and systolic pressure gradients. Exp Biol Med (Maywood) 2011;236:1364-72. [PubMed]
- Alfakih K, Plein S, Thiele H, et al. Normal human left and right ventricular dimensions for MRI as assessed by turbo gradient echo and steady-state free precession imaging sequences. J Magn Reson Imaging 2003;17:323-9. [PubMed]
- Schulz-Menger J, Abdel-Aty H, Rudolph A, et al. Gender-specific differences in left ventricular remodelling and fibrosis inhypertrophic cardiomyopathy: insights from cardiovascular magnetic resonance. Eur J Heart Fail 2008;10:850-4. [PubMed]
- Harrigan CJ, Peters DC, Gibson CM, et al. Hypertrophic cardiomyopathy: quantification of late gadolinium enhancement with contrast-enhanced cardiovascular MR imaging. Radiology 2011;258:128-33. [PubMed]
- Nojiri A, Hongo K, Kawai M, et al. Scoring of late gadolinium enhancement in cardiac magnetic resonance imaging can predict cardiac events in patients with hypertrophic cardiomyopathy. J Cardiol 2011;58:253-60. [PubMed]
- Catalano O, Moro G, Perotti M, et al. Late gadolinium enhancement by cardiovascular magnetic resonance is complementary to left ventricle ejection fraction in predicting prognosis of patients with stable coronary artery disease. J Cardiovasc Magn Reson 2012;14:29. [PubMed]
- Choudhury L, Mahrholdt H, Wagner A, et al. Myocardial scarring in asymptomatic or mildly symptomatic patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2002;40:2156-64. [PubMed]
- Choi DS, Ha JW, Choi B, et al. Extent of late gadolinium enhancement in cardiovascular magnetic resonance and its relation with left ventricular diastolic function in patients with hypertrophic cardiomyopathy. Circ J 2008;72:1449-53. [PubMed]
- Olivotto I, Maron BJ, Appelbaum E, et al. Spectrum and clinical significance of systolic function and myocardial fibrosis assessed by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. Am J Cardiol 2010;106:261-7. [PubMed]