
Will minimally invasive sleeve resection become the future trend for treatment of advanced lung cancer?
Caso et al. reported their outcomes of minimally invasive sleeve resection (1). Although the cohort is small, their outcomes were feasible and comparable to those of the open approach. However, will minimally invasive sleeve resection really become the next trend for treating advanced lung cancer, as is the case for video-assisted thoracoscopic surgery (VATS) lobectomy for early stage lung cancer?
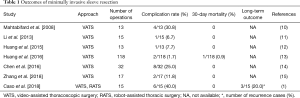
Until now, many studies and meta-analyses have shown that VATS is currently the growing trend for treating early stage lung cancer (2-6). Indeed, in Japan, 70.8% of total lung cancer surgeries are performed by VATS (7). However, sleeve resection by minimally invasive approaches, such as VATS or robot-assisted thoracic surgery (RATS), remains a challenging procedure in Japan and is only performed in limited institutions as a part of a clinical trial. Sleeve resections using minimally invasive approaches do not gain popularity in Japan probably because institutes require very high levels of patient safety and the occurrence rate of perioperative complications after sleeve resections with the open approach is already quite low (8). Also, another reason would be that long-term outcome after sleeve resection in Japan is also potentially acceptable in its present state (9). Therefore, in order for minimally invasive sleeve resection to become a feasible and standard procedure both in Japan and worldwide, the short- and long-term outcomes should be at least significantly better than the current outcome of sleeve resection performed by the open approach. So far, there are no large-scale analyses of short- and long-term outcomes after sleeve resection which compared the open approach with the minimally invasive approaches (Table 1) (10-15).
Full table
The data by Caso et al. have shown that short- and long-term outcomes of minimally invasive sleeve resection are potentially acceptable. However, it included heterogeneous types of patients, such as age, tumor histology and tumor extension, and we think the poor long-term outcome for lung cancer is disturbing, especially for adenocarcinoma. On the contrary, it is interesting that the outcomes are good for diseases that require only a minimal degree of lymph node dissection, such as carcinoid, adenoid cystic carcinoma, and metastatic lung tumors. We speculate that adequate and sufficient lymph node dissection for advanced lung cancers have led to the good long-term prognosis after sleeve resection. Since sleeve resection is usually required for advanced-stage lung cancers, the surgeons are required to perform not only sufficient lymph node dissection but also to preserve adequate blood flow to the bronchial anastomosis site. This is one reason why Japanese surgeon may prefer to do a sleeve resection by open thoracotomy rather than by minimally invasive approach. The concept of sufficient lymph node dissection with concomitant preservation of adequate blood flow is conflicting and the procedure thus requires a subtler technique and careful attention when compared to lobectomy.
Nonetheless, as shown in this paper by Caso et al., minimally invasive sleeve resection can be a suitable procedure for diseases that require only a minimal degree of lymph node dissection such as carcinoid, adenoid cystic carcinoma, and metastatic lung tumors. Furthermore, although there were only 2 cases of RATS sleeve resection in this study, the RATS approach has the potential to offer a similar level of lymph node dissection and residual blood flow to the anastomosis site, even when compared with the open approach. From this point of view, RATS may have to be considered separately from VATS, and it may become the future trend in this field of minimally invasive surgery.
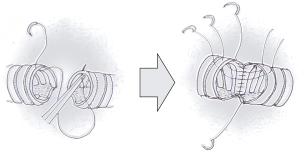
Furthermore, Caso et al. proposed to do the anastomosis by running suture using absorbable thread. We agree with the use of absorbable thread which is also widely used in Japan. However, the running suture method is not common amongst Japanese thoracic surgeons operating for lung cancer. The reason is mainly oncological, that is, when the lung cancer stage is advanced, it requires more extended lung resection and lymph node dissection. Therefore, although, the running suture method may allow easier suturing of the deepest point, simpler handling of threads, and shorter suturing time. Japanese surgeons prefer the interrupted suture method because it is more advantageous when adjusting difference in bronchus diameter and preserving blood flow. On the contrary, running suture is often used during lung transplant, because transplant does not require extensive lymph node dissection and the bronchus does not often need adjustment of diameter during anastomosis. For these reasons, the use of a hybrid anastomosis is rapidly gaining popularity in Japan (16). For the hybrid method, the deepest anastomosis point is anastomosed by running suture up to two fifths or half of the bronchus and the remaining bronchus is anastomosed by interrupted sutures (Figure 1). The hybrid method enables not only easier and quicker suturing for the deepest part of the anastomosis, but also allows diameter adjustment and better blood flow for the shallow part of the anastomosis.
In conclusion, the report by Caso et al. presented the feasibility of minimally invasive sleeve resection, especially for diseases other than advanced-stage lung cancer. Their study provided valuable information for selecting patients that may benefit from minimally invasive sleeve resection. They further showed the usefulness of running sutures and absorbable thread. However, for minimally invasive sleeve resection to become the growing trend for treatment of advanced-stage lung cancer, further data must be acquired concerning short- and long-term outcomes. Also, from an oncological viewpoint, we believe that RATS may outrun VATS and become the preferred approach amongst thoracic surgeons.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Caso R, Watson TJ, Khaitan PG, et al. Outcomes of minimally invasive sleeve resection J Thorac Dis 2018;10:6653-9. [Crossref] [PubMed]
- Kirby TJ, Mack MJ, Landreneau RJ, et al. Lobectomy--video-assisted thoracic surgery versus muscle-sparing thoracotomy. A randomized trial. J Thorac Cardiovasc Surg 1995;109:997-1001; discussion 1001-2. [Crossref] [PubMed]
- Sugi K, Kaneda Y, Esato K. Video-assisted thoracoscopic lobectomy achieves a satisfactory long-term prognosis in patients with clinical stage IA lung cancer. World J Surg 2000;24:27-30. [Crossref] [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Cai YX, Fu XN, Xu QZ, et al. Thoracoscopic lobectomy versus open lobectomy in stage I non-small cell lung cancer: a meta-analysis. PLoS One 2013;8:e82366. [Crossref] [PubMed]
- Hamaji M, Lee HS, Kawaguchi A, et al. Overall Survival Following Thoracoscopic vs Open Lobectomy for Early-stage Non-small Cell Lung Cancer: A Meta-analysis. Semin Thorac Cardiovasc Surg 2017;29:104-12. [Crossref] [PubMed]
- Masuda M, Kuwano H, Okumura M, et al. Thoracic and cardiovascular surgery in Japan during 2013. Gen Thorac Cardiovasc Surg 2015;63:670-701. [Crossref] [PubMed]
- Nagayasu T, Sato S, Yamamoto H, et al. The impact of certification of general thoracic surgeons on lung cancer mortality: a survey by The Japanese Association for Thoracic Surgery. Eur J Cardiothorac Surg 2016;49:e134-40. [Crossref] [PubMed]
- Okada M, Yamagishi H, Satake S, et al. Survival related to lymph node involvement in lung cancer after sleeve lobectomy compared with pneumonectomy. J Thorac Cardiovasc Surg 2000;119:814-9. [Crossref] [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ. Video-Assisted Thoracic Surgery Sleeve Lobectomy: A Case Series. Ann Thorac Surg 2008;85:S729-32. [Crossref] [PubMed]
- Li Y, Wang J. Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg 2013;44:1108-12. [Crossref] [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Huang J, Li S, Hao Z, et al. Complete video-assisted thoracoscopic surgery (VATS) bronchial sleeve lobectomy. J Thorac Dis 2016;8:553-74. [Crossref] [PubMed]
- Chen H, Xu G, Zheng B, et al. Initial experience of single-port video-assisted thoracoscopic surgery sleeve lobectomy and systematic mediastinal lymphadenectomy for non-small-cell lung cancer. J Thorac Dis 2016;8:2196-202. [Crossref] [PubMed]
- Zhang Z, Huang Q, Liao Y, et al. Application of the "continuous suture dividing and equal suture tightening" method in video-assisted thoracoscopic surgery sleeve lobectomy. J Thorac Dis 2018;10:5199-207. [Crossref] [PubMed]
- Hishida T, Aokage K, Yoshida J, et al. Extended bronchoplasty for locally advanced left lower lobe lung cancer: surgical technique and outcomes. Interact Cardiovasc Thorac Surg 2018;27:602-5. [Crossref] [PubMed]


