
Single-port thoracoscopic wedge resection using the Endo GIA Radial Reload: outcome of 15 cases
Introduction
Single-port thoracoscopic surgery has recently emerged as an approach for procedures such as lobectomy, wedge resection, pneumothorax surgery, and other thoracic surgeries (1-3). Although lung wedge resection is a relatively simple procedure, some specific techniques are necessary when using an endostapler because it is difficult to approach the lung tissue behind the lesion with an articulating endostapler during single-port thoracoscopic surgery (4).
We have previously described the procedure for single-port thoracoscopic wedge resection using the Endo GIATM Radial Reload device (Medtronic, Minneapolis, MN, USA) (5). The GIA Radial Reload has a curved cut line that is perpendicular to the direction of instrument insertion, which facilitates the approach to the lung tissue behind the lesion. Herein, we report the outcomes from 15 cases using this procedure.
Methods
This research study was approved by the institutional review board (No. 2013-3). We included patients who underwent wedge resection for peripheral lesions with a diameter of 20 mm or less for this procedure. Between August 2016 and February 2018, 15 patients underwent single-port thoracoscopic wedge resection with the Endo GIA Radial Reload device. Of the 15 patients, 9 (60%) were male and 6 (40%) were female. Age ranged from 45 to 75 years, with a mean age of 62.5 years. Seven patients had a history of smoking. Three patients underwent lung resection for primary lung cancer, seven patients for pulmonary metastasis from tumors in another organ, two patients for pulmonary arteriovenous fistula, two patients for undiagnosed pulmonary nodule, and one patient for pulmonary hamartoma. Lesion diameter ranged from 3 to 18 mm. The distance from the surface of the lung to the lesion ranged from 0 to 14 mm. Background characteristics of the study patients are shown in Tables 1 and 2.
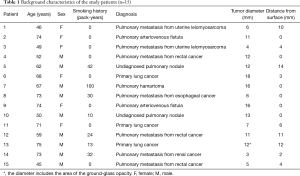
Full table

Full table
General anesthesia was induced and separate lung ventilation was established with a double-lumen endotracheal tube. The patient was placed in the recumbent position. We made the incision near the lesion so it can be palpated. Single-port thoracoscopic surgery was performed through a 3–5-cm incision. The incision was covered with an Alexis Wound Protector/RetractorTM X-small (Applied Medical, Rancho Santa Margarita, CA, USA) or small or extra small SurgiSleeveTM Wound Protector (Medtronic). We used a rigid scope of 5 mm in diameter with a 30° angle. We used finger palpation to find the lesion when it was not visible through the visceral pleura. When we could not find the lesion through the incision, we extended the incision to find the lesion through finger palpation. For the first stapler, we used a purple (medium) or black (large) GIA Radial Reload cartridge (Figure 1). For the second and subsequent staplers, we used the GIA Radial Reload cartridge or a straight cartridge, depending on the direction of the cut. Intercostal block or epidural anesthesia was used for postoperative pain management. Oral non-steroidal anti-inflammatory drugs were administered starting on the next day of surgery. Details of the procedure have been described previously (5).

Results
The details of each procedure are shown in Table 3. General anesthesia was used for all patients. Before wound closure, an intercostal block was routinely performed using ropivacaine hydrochloride hydrate. Since some patients complained of pain on the day of surgery, epidural anesthesia was used in three patients later in the series instead of an intercostal block. Continuous epidural infusion was performed for at least 1 day after surgery.

Full table
The duration of the procedure ranged from 24 to 55 minutes. The length of the skin incision ranged from 3 to 5 cm. In general, the length of skin incision was 3 cm for benign lesions and 4 cm for malignant lesions. We made longer incisions for malignant lesions in order to achieve sufficient surgical margins.
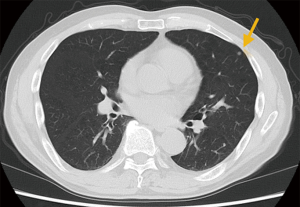
In Patient 14, we started the operation with a 5-cm skin incision. However, the lesion was too small to find (Figure 2). Therefore, we extended the incision to 7 cm and performed video-assisted thoracotomy. In all cases, 1 or 2 Radial Reload cartridges were used. The type of cartridge (black or purple) was selected based on the location and size of the lesion. In Patient 10, a stitch of suture and a polyglycolic acid sheet used as a covering were added to control air leakage identified after resection (Figure 3A).
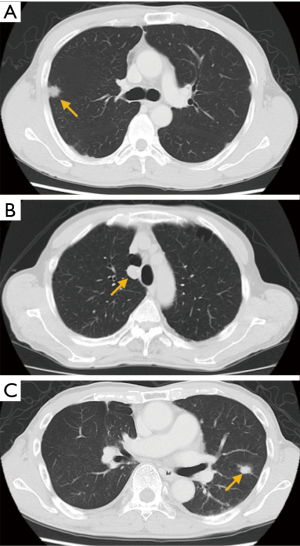
The postoperative course is shown in Table 4. In 13 of 15 patients, the chest drain was removed on postoperative day 1. In our clinical pathway, the duration of postoperative hospital stay was set to 3 or 4 days. Three patients whose chest tubes were removed on postoperative day 1 stayed in the hospital for 6 days for the following reasons. One patient has diabetes mellitus and one patient has interstitial pneumonia. We observed these patients for longer than usual because of their comorbidities. The other patient stayed longer due to postoperative pain. In 2 patients (Patients 7 and 13), chest drainage lasted for 9 and 5 days, respectively, due to prolonged air leakage. Both patients had a history of smoking and had evidence of pulmonary emphysema on computed tomography (Figure 3B,C). In Patient 7, air leakage resolved without any additional procedures. In Patient 13, chemical pleurodesis and coagulation factor XIII concentrate were needed to control air leakage. Brain infarction occurred after the resolution of air leakage during hospitalization. The duration of postoperative hospital stay ranged from 2 to 16 days, with a mean of 4.8 days. In one patient, wound infection occurred after discharge.
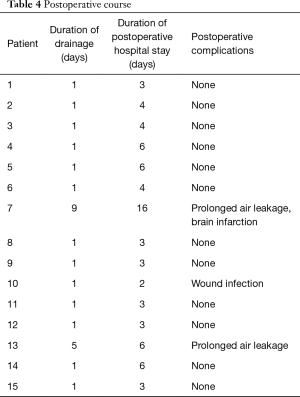
Full table
The duration of the postoperative follow-up ranged from 128 to 674 days. During this follow-up period, no local tumor recurrences were observed.
Discussion
We reported 15 cases of single-port thoracoscopic lung wedge resection, which included one case converted to thoracotomy. At first, we used general anesthesia with an intercostal block for this procedure, because single-port thoracoscopic surgery is less painful than multi-port thoracoscopic surgery, as previously reported (6). However, patients often complained of pain after the intercostal block wore off. Therefore, we switched to general and epidural anesthesia during the more recent cases. Although single-port thoracoscopic surgery is less painful, epidural anesthesia is still useful for pain management.
The minimum length of the skin incision was 3 cm. For the nodules adjacent to the pleura, a 3-cm incision is sufficient when it is not necessary to use palpation to locate the nodule. A longer incision is needed to find nodules distant from the pleura. One advantage of this procedure is that we can palpate the nodule with two fingers through the port, while only one finger is generally used in multi-port thoracoscopic surgery (7). In Patient 14, who had a 3-mm nodule that was 2 mm from the pleura, we could not find the lesion through a 5-cm port, so we extended the incision to find it. In such cases, it is easy to extend and widen the incision, which is another advantage of this procedure.
Air leakage occurred in three patients, including one intraoperative leak and two postoperative leaks. All three patients with air leakage were smokers and had evidence of emphysema on computed tomography. Although air leakage frequently occurs in patients with emphysema, the Radial Reload cartridge may not be a good choice for the resection of emphysematous lung. In patients with a history of heavy smoking or emphysema, we should consider using other staplers such as the Endo GIA™ Reinforced Reload (Medtronic).
In conclusion, this procedure is suitable for the resection of small nodules, because palpation with two fingers is easy. For pain management, general anesthesia combined with epidural anesthesia is recommended. Care must be taken in patients with emphysema; the GIA Radial Reload cartridge may not be a good choice for emphysematous lung.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: This research study was approved by the institutional review board (No. 2013-3). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Hirai K, Takeuchi S, Usuda J. Single-port video-assisted thoracic surgery for early lung cancer: initial experience in Japan. J Thorac Dis 2016;8:S344-50. [PubMed]
- Sano A, Kawashima M. Thoracoscopic reoperation for recurrent pneumothorax after single-incision thoracoscopic surgery. Asian J Endosc Surg 2015;8:480-2. [Crossref] [PubMed]
- Ocakcioglu I. Single-port thoracoscopic surgery for a hudge hydatid cyst. Gen Thorac Cardiovasc Surg 2017;65:235-8. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Sano A, Yotsumoto T. Single-port thoracoscopic lung wedge resection using the Endo GIA Radial Reload. Surg Today 2018;48:248-51. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Nakajima J, Murakawa T, Fukami T, et al. Is finger palpation at operation indispensable for pulmonary metastasectomy in colorectal cancer? Ann Thorac Surg 2007;84:1680-4. [Crossref] [PubMed]


