
Saving the split: the benefits of VATS thymectomy
Introduction
The surgical resection of the thymus for management of thymic pathology has been well described for more than 80 years (1). According to Blalock’s teachings, the standard approach to thymectomy is sternotomy; Blalock eschewed the cervical approach taken by others because he believed that “one should not rely upon the imperfect view which is obtained through an incision in the lower part of the neck” (2). The popularization of minimally invasive thoracoscopic surgery techniques in the 1990’s the landscape of thoracic surgery has shifted (3). Video-assisted thoracoscopic surgery (VATS) and robotic-assisted thoracoscopic surgery (RATS) became the standard approach for corpus procedures of general thoracic surgery such as lobectomies and esophagectomies, etc. (4,5). The benefits of minimally invasive techniques, such as decreased length of stay and post-operative pain, are well established (6,7). Previous studies have proven equivalent likelihood of an R0 resection as well as long-term oncologic outcome differences between transsternal and thoracoscopic approaches (8). When performed for myasthenia gravis, transthoracic and transsternal thymectomy yielded equivalent rates of symptomatic relief (9).
Despite the multitude of studies designed to demonstrate clinical equivalence between the two approaches, none have focused on patient centered outcomes or health care costs. In the current atmosphere of emphasis on savings and outcomes tracking, the relative efficiency and efficacy of each procedure is essential (10). The objective of this study was to evaluate the differences of short-term outcomes of invasive and transsternal thymectomy and VATS thymectomy using a large national database. We analyzed the metrics of quality and cost effectiveness by studying charges and length of stay as well as post discharge use of skilled nursing facilities.
Methods
Patient selection and data
We obtained our data from the NIS database, a multi-institutional clinical database capturing the administrative records of all payers (uninsured, Medicaid, Medicare and private insurance) (11). The 2010–2012 HCUP NIS database files provided the data for our analysis. We used the ICD-9 codes 07.8, 07.80, 07.81, 07.82 to identify patients undergoing open trans-sternal thymectomy. Patients undergoing VATS thymectomy were identified using the ICD-9 codes 07.83, 07.84. We performed multiple imputation for missing data once confirmed they were missing completely in random (12). We excluded patients younger than age 16 and also patients who had converted or had both open and thoracoscopic procedures performed. Additionally, given the relative rarity of the transcervical approach, our analysis focused only on the two most widespread approaches (13). Our study was granted an exemption by our institutional review board (IRB net exemption 1305029-1).
Data presentation
Continuous data are presented as the mean and standard deviation. Categorical data are presented as proportions and percentages. Univariate analysis included Student’s t-test or Chi-square test and for multivariate analysis we used binary logistic regression and linear regression. For our study, we considered P<0.05 as statistically significant.
Statistical analysis
Univariate and multivariate analyses controlling for demographics and comorbidities were analyzed using IBM SPSS. Multivariable logistic regression was performed with inpatient mortality as our primary outcome. We adjusted for demographics, socioeconomic status, comorbidity status, hospital size and type (urban vs. rural, teaching vs. community) and geographical location. We excluded the 4 cases of conversion to open approach in our data series to
Outcomes
Primary outcomes of interests were total length of stay (LOS), in patient mortality and charges. We also performed a subgroup analysis for patients who survived for the outcome of discharge to rehab/hospice/home with healthcare compared to discharge home. We defined optimal discharge as discharge to home with no further healthcare requirements, non-optimal discharge was defined as discharge to rehab/hospice/home with skilled care.
Results
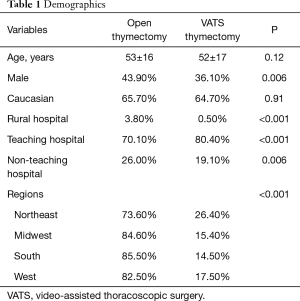
A total of 2,065 patients who underwent thymectomy were identified. Patients were divided into 2 groups based on type of surgery (open standard thymectomy via sternotomy vs. VATS thymectomy). Table 1 details the demographics of our population and provides comparison between the 2 groups. A total of 373 (18.1%) underwent VATS thymectomy and 1,692 (81.9%) underwent standard thymectomy. There was no difference in age between the two groups (P=0.12). The majority of patients in each group were Caucasian (65.5%). Just under half of the standard open approach patients were male (43.9%), while the majority of the VATS approach patients were female (36.1% male; P<0.001).
Full table
In univariate analysis, charges were higher for patients undergoing open thymectomy ($88,838±$120,892 vs. $57,251±$54,929, P<0.001) and hospital mortality was also higher in patients with open thymectomy (0.9% vs. 0%, P<0.05). Patients undergoing standard thymectomy had longer hospital LOS (6.1±6.6 vs. 3.3±3.4 d, P<0.001) in univariate analysis.
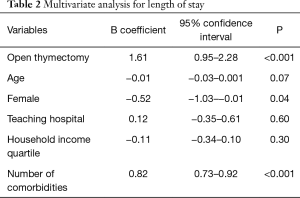
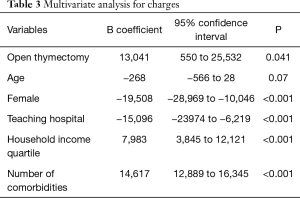
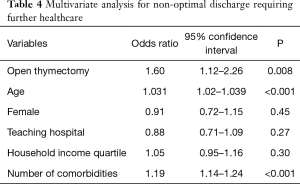
Multivariate analysis revealed thymectomy via sternotomy was independently associated with increased hospital LOS (B =1.6 d, P<0.001) and charges (B =$13,041, P=0.041) (Tables 2,3); There was no difference in mortality rate in multivariate analysis. When we looked at a subgroup of the patients who survived, patients undergoing VATS thymectomy were more likely to be discharged home compared to patients undergoing open thymectomy (87.1% vs. 77.2%, P<0.001) who were discharged to rehabilitation centers, hospice, or home with healthcare. We were also able to demonstrate a significant increased usage of discharges requiring further skilled healthcare support (odds ratio 1.6) (Table 4).
Full table
Full table
Full table
When we performed a trend analysis, there was a significant interval increase in number of patients undergoing VATS thymectomy (10% in 2010 vs. 19.2% in 2012, P<0.001). The shift to a minimally invasive approach for thymectomy was present in all regions but there was a more rapid initial adoption of the technique in the Northeast and South regions than the West and Midwest (Table 1).
Discussion
In this large retrospective U.S. database review of short-term postoperative outcomes following thymectomy, we noted a statistically increased length of stay, mortality and overall hospital charges. Furthermore, the differences in length of stay and charges held true on multivariate review based on approach. These results parallel other studies demonstrating decreased length of stay with equivalent results when comparing VATS lobectomy vs. open approach. In addition to demonstrating oncologic equivalence, minimally invasive approaches demonstrate decreased costs, secondary to decreased length of stay that make up for increased operating room time and instrument costs (14,15). Likewise, there was decreased rate of discharges requiring further skilled healthcare, representing an additional significant cost savings to the health care system (16).
Teaching hospitals were associated with decreased length of stay both in open and VATS thymectomy patients with a pronounced cost savings; likely secondary to decreased length of stay as well as decreased rate of non-optimal discharges, though these metrics failed to reach statistical significance in multivariate testing. The improved outcomes are presumed to be related to an increased volume of similar cases and potentially familiarity with minimally invasive approaches (17). Nonetheless, given the significant cost savings, these results suggest further study about whether thymectomy should be performed at high volume centers.
Interestingly, though perhaps not unexpectedly, female patients realized significant cost savings compared to matched male counterparts, presumably due to decreased length of stay. Corresponding to previously published research (18), female patients were also less likely (though not statistically significant) to utilize skilled nursing facilities post discharge. Also corresponding to earlier published research, increased household income was associated with decreased hospital charges (19); though unlike female patients there was not a statistically significant decrease in length of stay. Higher income patients were also more likely to be discharged requiring further skilled care, though again this failed to reach statistical significance.
As expected, the prevalence of the minimally invasive techniques increased during the study period. This corresponds to the increasing shift towards minimally invasive surgery both in general and when applied to thoracic surgery specifically (20,21). In line with the increasing emphasis placed on length of stay and patient satisfaction in the new bundled payment approach, the adoption of minimally invasive approaches will only continue to increase (22).
The strengths of our study are that it is nationally representative and can be applied to any hospital. The large sample size increased our statistical power and decreased likelihood of a type 2 error. Our study possesses several limitations. Firstly, NIS is an administrative inpatient sampling database, therefore long-term outcomes are unavailable. As in all large databases there is variability of data recording methods across institutions, limiting our ability to account for unrecorded comorbidities. Thirdly, the etiology behind length of stay is unclear and may be due to a confounding factor such as physician caution. Additionally, as NIS is an administrative database, collected retrospectively, the rate of conversion to open approach is unknown. Likewise, we do not have access or preoperative indications or histologic/pathologic findings in the specimens as this is a retrospective administrative database and these factors may have impacted short term outcomes Furthermore, Finally, since this is a retrospective observational study, residual confounding cannot be completely accounted for.
Conclusions
In summation, we observed a statistically significant decreased length of stay, charges and mortality comparing thoracoscopic vs. trans sternal approach to thymectomy. The choice of approach on multivariate analysis was found to favor a thoracoscopic approach as opposed to a transsternal approach. Based on these recommendations, combined with previous literature demonstrating improved outcomes for minimally invasive approach, it appears that the thoracoscopic approach is safer and more cost effective for patients. However further long term follow up is needed; as is the case in any oncologic/symptomatic resection, to ensure that any short term benefit is not at the expense of long term survival.
Acknowledgements
We thank the HCUP Data partners for their annual contributions to NIS. A full listing of participants can be found at http://hcup-us.ahrq.gov/partners.jsp.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Our study was granted an exemption by our institutional review board (IRB net exemption 1305029-1).
References
- Keynes G. The surgery of the thymus gland. Br J Surg 1946;33:201-14. [Crossref] [PubMed]
- Blalock A, Mason MF, Morgan HJ, et al. Myasthenia gravis and tumors of the thymic region: report of a case in which the tumor was removed. Ann Surg 1939;110:544-61. [Crossref] [PubMed]
- Cheng AM, Wood DE. VATS versus open surgery for lung cancer resection: moving beyond the incision. J Natl Compr Canc Netw 2015;13:166-70. [Crossref] [PubMed]
- Vannucci F, Gonzalez-Rivas D. Is VATS lobectomy standard of care for operable non-small cell lung cancer?. Lung Cancer 2016;100:114-9. [Crossref] [PubMed]
- Sihag S, Kosinski AS, Gaissert HA, et al. Minimally Invasive Versus Open Esophagectomy for Esophageal Cancer: A Comparison of Early Surgical Outcomes From The Society of Thoracic Surgeons National Database. Ann Thorac Surg 2016;101:1281-8; discussion 1288-9. [Crossref] [PubMed]
- Olavarrieta JR, Coronel P. Expectations and patient satisfaction related to the use of thoracotomy and video-assisted thoracoscopic surgery for treating recurrence of spontaneous primary pneumothorax. J Bras Pneumol 2009;35:122-8. [Crossref] [PubMed]
- Rizk NP, Ghanie A, Hsu M, et al. A prospective trial comparing pain and quality of life measures after anatomic lung resection using either thoracoscopy or thoracotomy. Ann Thorac Surg 2014;98:1160-6. [Crossref] [PubMed]
- Pennathur A, Qureshi I, Schuchert MJ, et al. Comparison of surgical techniques for early-stage thymoma: feasibility of minimally invasive thymectomy and comparison with open resection. J Thorac Cardiovasc Surg 2011;141:694-701. [Crossref] [PubMed]
- Meyer DM, Herbert MA, Sobhani NC, et al. Comparative clinical outcomes of thymectomy for myasthenia gravis performed by extended transsternal and minimally invasive approaches. Ann Thorac Surg 2009;87:385-90; discussion 390-1. [Crossref] [PubMed]
- Iorio R. Strategies and tactics for successful implementation of bundled payments: bundled payment for care improvement at a large, urban, academic medical center. J Arthroplasty 2015;30:349-50. [Crossref] [PubMed]
- Agency for Healthcare Research Quality (AHRQ) Agency for Healthcare Research Quality (AHRQ) HCUP Databases, Healthcare Cost and Utilization Project (HCUP): Overview of the Nationwide Inpatient Sample (NIS), 2013. Available online: http://www.hcup-us.ahrq.gov/nisoverview.jsp
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw 2011;45:1-67.
- Shrager JB. Extended transcervical thymectomy: the ultimate minimally invasive approach. Ann Thorac Surg 2010;89:S2128-34. [Crossref] [PubMed]
- Mafé JJ, Planelles B, Asensio S, et al. Cost and effectiveness of lung lobectomy by video-assisted thoracic surgery for lung cancer. J Thorac Dis 2017;9:2534-43. [Crossref] [PubMed]
- Swanson SJ, Meyers BF, Gunnarsson CL, et al. Video-assisted thoracoscopic lobectomy is less costly and morbid than open lobectomy: a retrospective multiinstitutional database analysis. Ann Thorac Surg 2012;93:1027-32. [Crossref] [PubMed]
- New York Department of Health. Estimated Average New York State Nursing Home Rates. Accessed 7/26/2018. Available online: https://www.health.ny.gov/facilities/nursing/estimated_average_rates.htm
- Gazoni LM, Speir AM, Kron IL, et al. Elective thoracic aortic aneurysm surgery: better outcomes from high-volume centers. J Am Coll Surg 2010;210:855-9, 859-60.
- Deakin DE, Wenn RT, Moran CG. Factors influencing discharge location following hip fracture. Injury 2008;39:213-8. [Crossref] [PubMed]
- Epstein AM, Stem RS, Weissman JS. Do the poor cost more? A multihospital study of patients' socioeconomic status and use of hospital resources. N Engl J Med 1990;322:1122-8. [Crossref] [PubMed]
- Xu T, Hutfless SM, Cooper MA, et al. Hospital Cost Implications of Increased Use of Minimally Invasive Surgery. JAMA Surg 2015;150:489-90. [Crossref] [PubMed]
- Klapper J, D’Amico TA. VATS versus open surgery for lung cancer resection: moving toward a minimally invasive approach. J Natl Compr Canc Netw 2015;13:162-4. [Crossref] [PubMed]
- Scott BC, Eminger TL. Bundled Payments: Value-Based Care Implications for Providers, Payers, and Patients. Am Health Drug Benefits 2016;9:493-6. [PubMed]


