Experience with acute diaphragmatic trauma and multiple rib fractures using routine thoracoscopy
Introduction
Traumatic diaphragmatic injuries are difficult to diagnose in the acute trauma setting but easily treated once diagnosis has been made. Establishing the diagnosis of a traumatic diaphragmatic injury has been a dilemma that has plagued acute care surgeons for centuries. Diaphragmatic rupture was first described in 1541 (1,2). A high clinical index of suspicion is needed to diagnose and effectively manage diaphragmatic rupture (1).
Despite advances in imaging and technology we still miss traumatic diaphragmatic injuries. It is believed that the incidence of missed or delayed diagnosis of traumatic diaphragmatic injuries is approximately 30% (3). Chest radiograph and ultrasound have a low diagnostic yield in the diagnosis of an acute diaphragm injury (4) and computed tomography (CT) has a diagnostic yield of 61–72% (5-8).
Most of the findings that a radiologist uses to make the radiographic diagnosis of an acute traumatic diaphragm injury rely upon associated abdominal injuries. This stems from the proposed mechanism of a traumatic diaphragm injury.
Diaphragmatic injuries in the blunt trauma patient have traditionally been thought of as an intra-abdominal injury. The mechanism by which these injuries occur have been explained as an abrupt change in the intra-abdominal pressure causing rupture of the diaphragm upwards into the chest cavity (9,10). This has led to an entire algorithm for the management of traumatic diaphragm injuries based on an intra-abdominal process (11).
In our trauma center we have a well-established chest wall injury program and an algorithm used to monitor and treat patients felt to be at greatest risk from blunt chest trauma. We provide surgical rib fixation for patients with flail chest injuries or severe multiple rib fractures. We use routine thoracoscopy in the surgical management of these patients. We have diagnosed and treated several acute diaphragmatic injuries in our chest wall injury patient population. This experience has prompted us to perform a review of our experience with acute traumatic diaphragmatic injuries in our chest wall injury population.
Methods
A retrospective review of medical records was performed on all patients admitted to our facility with traumatic diaphragmatic injuries. We looked at our trauma experience between January 2015 and January 2018 in our level II trauma center located in Mission Viejo, California.
Potential patients were identified by performing a query of the trauma database to ascertain a list of all trauma patients with rib fractures and or diaphragmatic injuries using ICD-9 and ICD-10 codes. Once this list was obtained we reviewed all medical records and identified the frequency of associated thoracic and abdominal injuries. Attention was focused on methods of diagnosis, preoperative imaging, intraoperative findings and surgical approach. Patients were excluded if they expired within twenty-four hours of admission.
Results
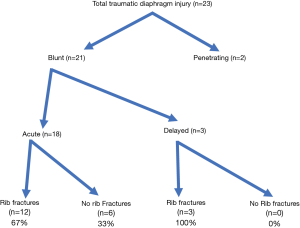
A total of 566 patients were admitted to our facility with multiple rib fractures and or diaphragmatic injuries. A total of 23 patients were seen at out facility with traumatic diaphragmatic injuries. Twenty-one (91%) of the diaphragmatic injuries were from blunt trauma while only 2 (9%) were from penetrating trauma. Of the 21 blunt traumatic diaphragmatic injuries, a total of 15 (71%) of them had associated rib fractures. Six (29%) of the blunt traumatic diaphragm injuries did not have associated rib fractures but had evidence of intra-abdominal injuries.
There were three cases of a delayed diagnosis of a diaphragmatic injury. The delayed cases all had significant rib fractures at time of trauma. One had surgical fixation of rib fractures without thoracoscopy and the other two did not have surgical fixation at time of original blunt trauma, and were treated non-operatively.
Acute diaphragmatic injury
Sixty-seven percent of patients in the acute blunt trauma diaphragmatic injury group had associated rib fractures, while only 33% did not have rib fractures but instead had major abdominal injuries. Fifty-five percent of patients in this group were diagnosed at the time of surgery with an acute diaphragmatic injury despite preoperative imaging. Eighty percent of these intraoperative diagnoses were made with thoracoscopy, the thoracoscopy was being used for the surgical management of multiple rib fractures and flail chest injuries.
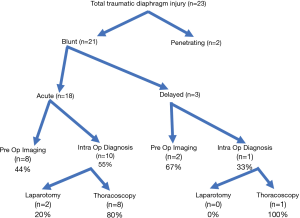
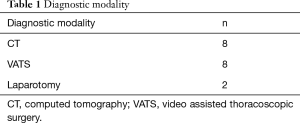
Eight cases were diagnosed with preoperative imaging. Ten cases were diagnosed intraoperatively at time of surgery (Table 1, Figure 1).
Full table
Acute diagnostic modality
CT was the most consistent preoperative diagnostic tool. Thoracoscopy was the most common intraoperative diagnostic modality.
All of the patients, in the acute injury group, diagnosed preoperatively with CT scan went on to have surgical repair of diaphragm rupture. Seven had laparotomy and 1 had thoracoscopy (Figure 2).
Technique for thoracoscopic diaphragm repair in acute setting
Routine thoracoscopy is performed in the surgical management of rib fractures in our center. We use a 5 mm port placed in the posterior axillary line at approximately the level of the 8th intercostal space. Using a thoracoscope, additional ports are placed under direct visualization, one 5 mm port in the high anterior axillary line and an additional port in the lower anterior chest just above the level of the diaphragm. The lungs are carefully inspected, the diaphragm and other structures are assessed for injury. Hemothorax is evacuated and the rib fractures are reduced at this time using a thoracoscopic grasper to reduce the fractures with radial outward pressure. Using a separate muscle sparing incision, approximately 4–5 cm in size, the rib fractures are stabilized by placing a plate and screw on the external aspect of the ribs in the submuscular space. If there is evidence of a diaphragmatic injury, the repair is performed immediately. The diaphragmatic lacerations range in size from 2–5 cm, depending on the severity of rib displacement. The repair of the diaphragm is done using the ports already placed for thoracoscopy. The repair is performed using interrupted 0-vicryl sutures. No thoracotomy is performed at any point for the procedure.
The transabdominal approach for diaphragm repair in the acute setting is usually done through a laparotomy incision secondary to associated intra-abdominal injuries related to the blunt trauma.
Transthoracic repair of the diaphragm has traditionally been reserved for chronic diaphragm injuries and are typically done through a thoracotomy. However, video assisted thoracoscopic surgery (VATS) is an option. In the chronic setting, patients will often have significantly more adhesions related to the initial injury requiring extensive decortication to release the lungs from the diaphragm. The diaphragmatic defect, in the chronic setting, tends to also be scarred and retracted at the edges which can also be adherent to underlying intra-abdominal organs which require extensive dissection. The chronic diaphragmatic lacerations are often difficult to repair primarily due to retraction and may require a patch for repair.
Delayed diaphragmatic injury
There were only three diagnoses of delayed diaphragmatic injury in our study group. In the delayed group, patients presented with various symptoms. One presented with a repeat blunt trauma injury and additional associated rib fractures, several years after the original trauma. One patient presented within 30 days after discharge from trauma center with persistent rib pain following non-operative management of multiple rib fractures. One patient presented, after 30 days, with persistent chest and abdominal pain after repair of rib fractures at an outside facility. Thoracoscopy was not used during the initial rib fixation surgery.
Diagnosis of delayed diaphragmatic injuries was made at time of thoracoscopy in 1 case and with preoperative imaging in two cases. All of the delayed diaphragmatic injures were repaired thoracoscopically.
Conclusions
In our series, we identified a group of patients with diaphragmatic injuries admitted to our facility over a three-year period. We tested our theory that diaphragmatic injuries may be more closely associated with chest trauma as opposed to what has been previously described as an abdominal injury. We recognize that our facility sees a disproportionately larger number of blunt trauma patients as opposed to penetrating trauma. We also recognize that many diaphragmatic injuries may have significant intra-abdominal catastrophe leading to patient demise prior to diagnosis and treatment.
Our series of patients appears to show a significant number of diaphragmatic injuries in association with multiple rib fractures. We also noted that the patients with multiple rib fractures and diaphragmatic injuries tended to have ribs involving the lower chest wall. This would explain the mechanism of injury being more of a penetrating injury from the fractured rib puncturing and tearing the diaphragm as opposed to a pressure gradient seen in major abdominal trauma.
Most of our patients were diagnosed at the time of thoracoscopy as opposed to preoperative imaging. Pre-operative imaging in the intra operative diagnosis group of patients did not yield a diagnosis of diaphragmatic trauma or a suspicion for diaphragmatic trauma.
We believe the incidence of diaphragmatic injuries may be higher than previously described. We also believe that occult diaphragmatic injuries may be more closely associated with chest wall trauma and multiple rib fractures.
Transthoracic management of traumatic diaphragmatic injuries has traditionally been reserved for delayed or chronic diaphragm injuries. Diaphragmatic injuries in the acute setting have traditionally been managed using a transabdominal approach. We have seen excellent outcomes in our patient population using a thoracoscopic approach for the surgical management of acute and chronic diaphragm injuries.
Many diaphragmatic injuries are diagnosed and managed at the time of abdominal exploration for other injuries. The increasing use of interventional radiology in the management of splenic lacerations and liver lacerations has led to a decrease in the need for abdominal explorations in stable patients. This may potentially lead to an increase in missed or delayed diagnosis of diaphragmatic injuries (12).
Thoracoscopy may be strongly considered in the early diagnosis of diaphragmatic injuries in the acute setting and may allow for a simple thoracoscopic repair of the injury.
We recognize that not all facilities perform routine thoracoscopy in the management of multiple rib fractures. However, we conclude that thoracoscopy may prove to be helpful in the algorithm for the work up of an occult diaphragmatic injury. We also conclude that the diagnostic yield of thoracoscopy, in the diagnosis of acute diaphragm injuries, appears to be greatest in patients with multiple rib fractures involving the lower chest wall, even in the absence of intra-abdominal injuries or radiographic evidence of diaphragmatic abnormalities.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by St. Joseph Health IRB (#17-087) and written informed consent was obtained from all patients.
References
- Christie DB 3rd, Chapman J, Wynne JL, et al. Delayed right-sided diaphragmatic rupture and chronic herniation of unusual abdominal contents. J Am Coll Surg 2007;204:176. [Crossref] [PubMed]
- Goh BK, Wong AS, Tay KH, et al. Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt trauma. CJEM 2004;6:277-80. [Crossref] [PubMed]
- Weyant MJ, Fullerton DA. Blunt thoracic trauma. Semin Thorac Cardiovasc Surg 2008;20:26-30. [Crossref] [PubMed]
- Mhmoud AF, Raeia MM, Elmakarem MA. Rupture diaphragm: Early diagnosis and management. J Egypt Soc 2017;25:163-70.
- Larici AR, Gotway MB, Litt HI, et al. Helical CT with sagittal and coronal reconstructions: accuracy for detection of diaphragmatic injury. AJR Am J Roentgenol 2002;179:451-7. [Crossref] [PubMed]
- Murray JG, Caoili E, Gruden JF, et al. Acute rupture of the diaphragm due to blunt trauma: diagnostic sensitivity and specificity of CT. AJR Am J Roentgenol 1996;166:1035-9. [Crossref] [PubMed]
- Killeen KL, Mirvis SE, Shanmuganathan K. Helical CT of diaphragmatic rupture caused by blunt trauma. AJR Am J Roentgenol 1999;173:1611-6. [Crossref] [PubMed]
- Bodanapally UK, Shanmuganathan K, Mirvis SE, et al. MDCT diagnosis of penetrating diaphragm injury. Eur Radiol 2009;19:1875-81. [Crossref] [PubMed]
- Scharff JR, Naunheim KS. Traumatic diaphragmatic injuries. Thorac Surg Clin 2007;17:81-5. [Crossref] [PubMed]
- Karmy-Jones R, Jurkovich GJ. Blunt chest trauma. Curr Probl Surg 2004;41:211-380. [Crossref] [PubMed]
- Asensio JA, Petrone P, Demitriades D. Injury to the diaphragm. In: Davis JW, Moore EE, Feliciano DV, et al. editors. Trauma. 5th ed. McGraw-Hill, 2003:613-6.
- Zealley IA, Chakraverty S. The role of interventional radiology in trauma. BMJ 2010;340:c497. [Crossref] [PubMed]